Robotic thymectomy in patients with myasthenia gravis by vascular skeletonization
Introduction
Surgical resection of the thymus is indicated in the presence of myasthenia gravis (MG) and thymectomy is frequently used in the treatment of MG.
The traditional invasive surgical approach was median sternotomy. The patients showed a slow recovery for the trauma. Robot-assisted thymectomy is a safe and minimally invasive operation.
Surgical technique
The patient was intubated with a left-side double-lumen tube and was placed supine with the middle part of the right side lifted up with a cushion to 30 degrees. A 12-mm port in the 5th intercostal space in the midaxillary line was made for camera. Other two incisions 8 and 25 mm were made in the 3rd intercostal space in the midaxillary line for arm 2, in the 6th intercostal space in the anterior axillary line for arm 1 and an assistant instrument, respectively. The three incisions formed an isosceles and obtuse triangle with at least 8 cm per side.
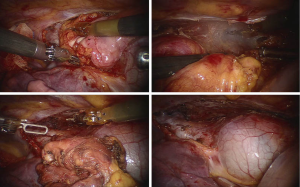
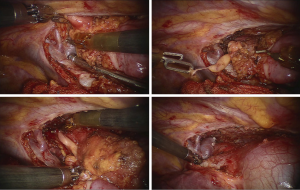
Resection of all the thymic and fat tissue started from the right phrenic nerve up to the left. The bodies and the hind parts of the thymus were dissected in the jugular direction until the brachiocephalic vein was reached (Figure 1). Vascular skeletonization followed by reaching the upper poles of the two sides. Thymic veins were cut with cautery. The branches of internal thoracic vein may be clipped to get a better visualization (Figure 2). Lift the specimen up from the major vessels to complete dissection. The specimen was removed en bloc in gloves through the anterior axillary incision.
Comment
Since the totally endoscopic robotic thymectomy was initially reported by Dr. Ashton in 2003, this new procedure for patients with MG has been gradually accepted among the world. Some series show that it is safe to perform robotic thymectomy in patients with an early stage thymoma. While the issue that whether video-assisted thoracoscopic surgery (VATS) is appropriate to the patients with MG is still under discussion, the robotic procedure has brought dawn to the future. With the extremely flexible Endowrist and high definition 3D images, the matters which are the potential disadvantages for the VATS compared to the sternectomy, such as the incidence of uncompleted resection, the small space for manipulation would have opportunities to turn off by the robotic techniques. The 3D visualization also facilitates an easy, safe and precise dissection of thymic tissue from the major vessel structures and phrenic nerve to reduce the intraoperative complications even in vascular skeletonization.
More positive evidences have been published by the researchers from the North American, the Europe and China. However, as the initial etiology of the MG it is, whether the robotic thymectomy could replace the VATS or even open surgery should be critically evaluated. A long term follow-up is needed to consider this new procedure as a standard approach definitively. The neurologic outcome and prognosis for the patients with MG is still in the top priority instead of the fashion of technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.