
Population attributable risk of excess weight, abdominal obesity and physical inactivity for type 2 diabetes in Chinese men and women
Introduction
Diabetes mellitus (DM) has become one of the most prevalent chronic diseases in the world. According to the latest data from the International Diabetes Federation, the global prevalence of diabetes is 9.3% (463 million people) in 2019 and will reach 10.2% (578 million people) in 2030 (1). The burden of diabetes in China is of high prevalence. The estimated standardized prevalence of total diagnosed and undiagnosed diabetes was 10.9% (95% CI: 10.4–11.5%) among the Chinese adult population in 2013 (2).
The prevalence of obesity was also rising rapidly in the past decades worldwide. The prevalence of obesity varies by country and ranges from 3.7% in Japan to 38.2% in the United States (3). A study based on nationally representative data demonstrated that the prevalence of abdominal obesity was 29.1% (28.6% in men and 29.6% in women) in China (4). And urban residents in China lack physical exercise, especially in the middle-aged and elderly population (5). Many studies reported that obesity and physical inactivity are associated with the incidence of T2DM. Obesity and weight gain dramatically increased the risk (6-8), and physical inactivity further increased the risk as well, independently of obesity (9,10).
Although there are many epidemiological studies on the relationship between obesity, physical activity, and diabetes, limited prospective research has been done in China to quantify the PAR of excess weight and physical inactivity on T2DM incidence. Therefore, we analyzed the data from two large prospective cohorts to evaluate the association between excess weight, physical inactivity, and the risk of T2DM and then calculated the proportion of T2DM incident cases attributable to them.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-6121).
Methods
Study population
The study was based on two ongoing, population-based prospective cohort studies, the Shanghai Men's Health Study (SMHS) and the Shanghai Women's Health Study (SWHS). These two studies recruited 61,469 eligible men aged 40–74 years (January 2002 to September 2006) and 74,940 eligible women aged 40–70 years (December 1996 to May 2000) in Shanghai. Details about studies design, scientific rationale, and demographic characteristics at baseline survey have been published previously (11,12). Participants were interviewed in-person by trained interviewers (retired nurses or physicians) using a structured questionnaire to obtain information on demographic characteristics, lifestyle, dietary habits, medical history, and anthropometric measurements (including weight, height, circumferences of waist and hips). Since the baseline survey, participants have been followed up every 3–4 years through in-person interviews to update their information about health status and lifestyle (SMHS: 2004–2008, 2008–2011, 2012–2017; SWHS: 2000–2002, 2002–2004, 2004–2006, 2007–2010, 2012–2017). Excluding participants with diabetes at baseline, missing data on BMI, waist circumference, physical activity and lifestyle factors, a total of 56,691 men and 70,849 women were included in the analysis. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All participants provided written informed consent. This study was approved by the Renji Hospital Ethics Committee of Shanghai Jiao Tong University School of Medicine (No. KY2019-196).
Lifestyle factors assessment and definition
At baseline recruitment, we applied a validated food frequency questionnaire (FFQ) and physical activity questionnaire (PAQ) to collect information on dietary habits and physical activity (13-16). Energy expenditure in standard metabolic equivalent values (METs) was used to estimate the intensity of each type of physical activity (17). Exercise/sports-related energy expenditure was estimated by the weighted average of energy expended in all activities reported during the 5 years preceding the interview. Individual non-exercise-related activities were estimated using the following standard METs: housework, 2.0 METs; walking, 3.3 METs; stair climbing, 9.0 METs; bicycling, 4.0 METs (17). We calculated total physical activity (MET-hours/week) by combining energy expenditure from all types of physical activity. Physical inactivity was defined as METs below the first quartile. Total energy intake was estimated based on dietary information from the food frequency questionnaire (13,14).
Bodyweight and height were measured twice during the baseline survey by a trained interviewer following a standard protocol. Overweight and obesity were defined according to the recommendation of previous studies for Chinese people as a BMI of 24.0 to 27.9 kg/m2 and a BMI of ≥28.0 kg/m2 (18,19). Abdominal obesity was defined as WC ≥90 cm in men and ≥80 cm in women using criteria recommended by the International Diabetes Federation (IDF) for Chinese adults (20). Excess body weight was defined as BMI ≥24.
Diabetes ascertainment
We conducted a follow-up survey every 3–4 years to record the occurrence of T2DM. Information collected includes the diagnosis of diabetes by a physician, fasting blood glucose level, postprandial blood glucose level, diabetes symptoms, and medical treatment (hypoglycemic agent or insulin). In this study, the participant was considered as an incident case of T2DM if he/she was been diagnosed by a physician and met at least one of the following criteria: (I) fasting glucose level ≥7 mmol/L; (II) blood glucose 2 hours after meal ≥11.1 mmol/L; (III) use of insulin or hypoglycemic agents; and (IV) had symptoms of diabetes. Self-reported diabetes in our two cohorts was proved sufficiently valid (21).
Statistical analysis
Differences in demographic characteristics between diabetes and non-diabetes groups were assessed using a t-test for continuous variables and the Chi-square test or rank-sum test (Wilcoxon) for categorical variables. The person-year was determined by calculating the interval between the baseline time and the date of diagnosis of T2DM, death, or latest follow-up, whichever came first. We utilized the Cox proportional hazards regression model to estimate the risk of T2DM with lifestyle factors, in age-adjusted (model 1) and multivariate-adjusted (model 2) models. Relevant variables that might have confounded the relationship to the risk of T2DM in model 2 included age (continuous), education (category), income (category), occupation (category), BMI (category), physical activity (quartiles, MET-h/week), family history of diabetes (yes/no), energy intake (quartiles), history of cigarette smoking (never, past, current), history of alcohol drinking (never, past, current), hypertension (yes/no), menopausal status (for women; yes/no). The proportional hazards assumption for the Cox model was checked using Schoenfeld residuals, and no violation was found. Considering the multicollinearity of the variables, we fitted the data linearly, and the variance inflation factor was 1.4. Considering the interaction between obesity and physical activity, we stratified the analysis according to BMI.
The PAR refers to the proportion of incident cases in a particular population that can be reduced after selected risk factors are eliminated within a certain period (22). T2DM is a multifactorial chronic disease so the PAR must be calculated while the distribution of other relevant factors is unchanged. To quantify the public health impact of lifestyle factors, we performed a model-based estimation of PAR as proposed by Dahlquist and Zetterqvist (23) with adjustment of the potential confounders. The time node of PAR was from baseline to the latest date of follow-up. PAR analysis was conducted in (R version 3.6.1); another analysis was performed using SAS software (version 9.2 SAS Institute, Inc., Cary, North Carolina). All tests of statistical significance were based on P values of 0.05 (two-sided) probabilities.
Result
After removing all participants with diabetes at the baseline survey, 70,849 females and 56,691 males were included in the current analysis. During 13.9 years (981,504 person-years) and 9.2 years (519,157 person-years) of follow-up, 5,925 female and 3,315 male incident cases of T2DM were identified in two cohorts. Corresponding density incidence rates of women and men were 6.0/1,000 person-years and 6.4/1,000 person-years.
The demographic characteristics of participants by T2DM status are shown in Table 1. The prevalence of overweight and obesity was 34.26% and 11.76% in women, and 37.32% and 7.96% in men. The proportions of women and men with abdominal obesity were 39.55% and 29.05%. The smoking rate was very high (60%) among men. Both in men and women, participants with T2DM were older, more likely to have lower levels of education, higher waist circumference, and higher BMI than participants without T2DM. In addition, participants with a family history of diabetes were also more likely to develop T2DM during subsequent follow-up. For women, participants with T2DM were more likely to be manual workers and have lower income than those without T2DM, but these associations were not seen in male participants.
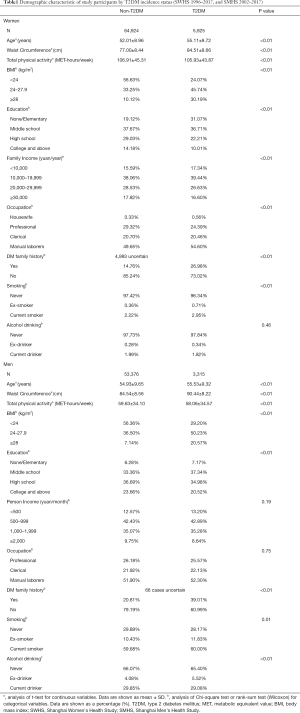
Full table
Table 2 shows the relationships between BMI, waist circumference, physical activity and T2DM. The BMI and waist circumferences were positively correlated with the risk of T2DM (Ptrend<0.01). The HR of T2DM was 3.06 (95% CI: 2.87, 3.25) for excess weight women and was 2.61 (95% CI: 2.42, 2.82) for men, compared with participants with BMI less than 24. The risks of T2DM were 4.58 (95% CI: 4.25, 4.93) and 4.09 (95% CI: 3.69, 4.54) times as high in women and men with BMI ≥24 as those with BMI <28. Compared with subjects with normal waist circumference, the HR of T2DM in abdominally obese women was 3.58 (95% CI: 3.36, 3.81) and that in men was 2.53 (95% CI: 2.35, 2.72). After adjustment for confounders, as physical activity levels increased, the risk of T2DM decreased in both women and men (Ptrend<0.01). The HRs across quartile of total physical activity were 1.00, 0.93, 0.84, 0.84 in men and 1.00, 0.99, 0.92, 0.88 in women, respectively.
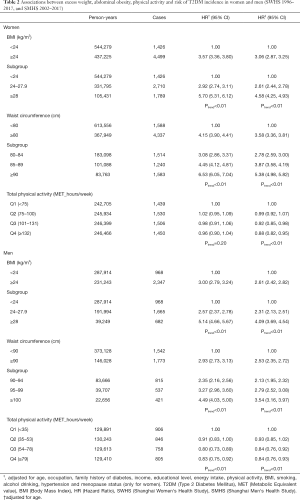
Full table
Analysis stratified according to BMI was shown in Table 3. Among overweight women, physical activity was associated with a decreased risk of T2DM (HRQ4|Q1 =0.87, 95% CI: 0.78, 0.97, Ptrend<0.01). Among men with a BMI of less than 24, physical activity was associated with a decreased risk of T2DM (HRQ4|Q1=0.66, 95% CI: 0.55, 0.80, Ptrend<0.01). However, this association was not found in overweight or obese men.

Full table
In men, the estimated proportions of T2DM incident cases attributable to excess weight, abdominal obesity, physical inactivity were 41.5% (95% CI: 38.5%, 44.6%), 30.3% (95% CI: 27.8%, 32.8%), and 3.6% (95% CI: 1.7%, 5.5%) as shown in Table 4. In women, the estimated proportions of T2DM incident cases attributable to excess weight, abdominal obesity and physical inactivity were 48.6% (95% CI: 46.3%, 50.9%), 50.4% (95% CI: 48.3%, 52.5%) and 1.7% (95% CI: 0.4%, 3.0%). Furthermore, we explored the contributions of factors with different age groups. According to their baseline age, age group 40-49 was found to have the highest PARs of excess weight; age group 50-59 was found to have the highest PARs of physical inactivity in both women and men.
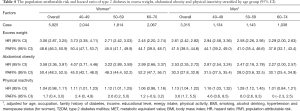
Full table
Discussion
In these two large prospective cohort studies, we found that excess body weight and abdominal obesity were major risk factors for T2DM incidence among middle-aged Chinese. Besides, we observed that physical activity had a protective effect on the development of T2DM in middle-aged adults. These large observational cohort studies suggested that exposures to unfavorable levels in BMI, waist circumference, physical activity were attributable for 48.6%, 50.4% and 1.7% cases of incident T2DM in women and 41.5%, 30.3% and 3.6% in men.
We found that excess body weight and abdominal obesity were associated with a dramatically increased risk of T2DM among middle-aged Chinese, consistent with previous studies (6-8). It has been reported that obesity was an independent risk factor and a major cause of T2DM (24). A study of 154,989 subjects from Asian, New Zealand, and Australian populations in the Asia-Pacific region found that baseline BMI was positively associated with T2DM risk, with a 27% reduction in diabetes risk for each 2 kg/m2 reduction in BMI (7). The biological mechanism underlying this effect is that adipocytes secrete signaling molecules that increase insulin resistance and glucose intolerance, and that levels increase in diet-induced obesity as well as in genetic models of obesity and insulin resistance (25). In our study, there was a gender difference in the association between excess body weight, abdominal obesity and risk of T2DM. Women with excess body weight or abdominal obesity had a higher risk of developing T2DM than men. The reason may be related to the menopausal status of female subjects, increased visceral fat deposition among women after menopause may promote increased insulin resistance and elevated incidence of the metabolic syndrome in older women (26,27).
In PAR analysis, we found that almost half of T2DM cases could be attributed to excess body weight (women: 48.6%, men: 41.5%). Previous studies also showed a large proportion of T2DM cases attributable to excess body weight. In Tehran, the PARs adjusted for family history of diabetes, age, triglycerides, systolic blood pressure was 23.3% for overweight, and 37.1% for obesity (28). In our study, 50.9% female and 31.2% male T2DM were attributed to abdominal obesity. A cohort study conducted in a sample of 24,996 Chinese adults aged 35–74 years, found that 28.1% incident diabetes among men and 41.2% among women would theoretically not have occurred if all people had no abdominal obesity (29). In Australia, the percentage of diabetes incident cases attributable to obesity (BMI combined waist circumference) was 47% according to the results from the Australian Diabetes, Obesity and Lifestyle Study (30).
Previous epidemiological studies have suggested that physical activity was associated with a reduced risk of T2DM (9,10,31). Our study also found a similar result. Similarly, a sedentary lifestyle was a risk factor for T2DM. Bennet DA conducted a follow-up of 512,000 Chinese for 9 years and found that more physical activity and less leisure time could reduce the risk of T2DM, and sitting an additional hour per day increased the risk of T2DM by 5% (31). Among the middle-aged population in Shanghai, we found that total physical activity in women was higher than men, which may be related to women doing more housework and lack of exercise for both men and women. In men with normal BMI, total physical activity was protective against T2DM but not found in other BMI groups. The possible reason was that obese men need more physical activity than normal-weight men to have protective effects against T2DM.
The PARs of T2DM caused by physical inactivity in men and women were 3.6% and 1.7%. The possible reason was that men have lower levels of physical activity than women and that the criteria for physical inactivity differed between men and women. Furthermore, The HR and PAR of T2DM caused by inadequate physical activity were highest in men aged 50–59 years. Therefore, men aged 50–59 years were priority populations who needed to improve their lifestyle on health intervention. There are few studies on PAR of physical activity on T2DM and the criteria for physical activity are different. Hosein Fallahzadeh (32) estimated PAR of T2DM by Bayesian methods based on the cohort study of chronic diseases in the adults of Yazd city, which showed that 17.92% women and 18.53% men cases were attributable to physical inactivity in Iran. In Finland, PARs for absence of exercise ranged from 3% (95% CI: −11.0, 16.0) in men to 7% (95% CI: −9.0, 20.0) in women (33).
Strength and limitations
Our study was based on two large population-based cohort studies with high quality exposure data and high recruitment and high follow-up rates (>90%), which minimized selection bias. Another advantage is the availability of detailed information including lifestyle factors, and the total energy intake of subjects was estimated according to a food frequency questionnaire, which allowed us for a more comprehensive evaluation of PAR. However, several possible limitations of this study warrant consideration. The main concern for our study is its reliance on self-reported T2DM, misclassification and undiagnosed are likely. Also, our research is based on Chinese adults aged 40–74, thus, more studies are needed to investigate the PAR of excess body weight on T2DM incidence by other groups of age.
Conclusions
In conclusion, our findings from the two prospective cohorts revealed that excess weight and abdominal obesity were associated with a significant increase in the risk of T2DM incidence in Chinese adults. Excess weight and abdominal obesity could explain nearly 50% of T2DM cases. Insufficient physical activity accounted for a small part of T2DM cases. Weight control and promotion of physical activity should be conducted through various ways to reduce the burden of T2DM in China.
Acknowledgments
We would like to thank the participants and the staff from the Shanghai Women's and Men’s Health Studies for their contribution to this research.
Funding: This work was supported by the Research Grant from the State Key Laboratory of Oncogenes and Related Genes (#91-1708), and the cohorts were supported by the grants from the US National Institutes of Health [UM1 CA182910, UM1 CA173640].
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-6121
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-6121
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-6121). Dr. Xiang reports grants from Research Grant from the State Key Laboratory of Oncogenes and Related Genes (#91-1708), and the cohorts were supported by the grants from the US National Institutes of Health [UM1 CA182910, UM1 CA173640], during the conduct of the study. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Renji Hospital Ethics Committee of Shanghai Jiaotong University School of Medicine (KY2019-196) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 2019;157:107843. [Crossref] [PubMed]
- Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017;317:2515-23. [Crossref] [PubMed]
- Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 2019;15:288-98. [Crossref] [PubMed]
- Zhang L, Wang Z, Wang X, et al. Prevalence of Abdominal Obesity in China: Results from a Cross-Sectional Study of Nearly Half a Million Participants. Obesity 2019;27:1898-905. [Crossref] [PubMed]
- Muntner P, Gu D, Wildman RP, et al. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health 2005;95:1631-6. [Crossref] [PubMed]
- Paul S, Thomas G, Majeed A, et al. Women develop type 2 diabetes at a higher body mass index than men. Diabetologia 2012;55:1556-7. [Crossref] [PubMed]
- Ni MC, Parag V, Nakamura M, et al. Body mass index and risk of diabetes mellitus in the Asia-Pacific region. Asia Pac J Clin Nutr 2006;15:127-33. [PubMed]
- Field AE, Coakley EH, Must A, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 2001;161:1581-6. [Crossref] [PubMed]
- Helmrich SP, Ragland DR, Leung RW, et al. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med 1991;325:147-52. [Crossref] [PubMed]
- Hu FB, Sigal RJ, Rich-Edwards JW, et al. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA 1999;282:1433-9. [Crossref] [PubMed]
- Shu XO, Li H, Yang G, et al. Cohort Profile: The Shanghai Men's Health Study. Int J Epidemiol 2015;44:810-8. [Crossref] [PubMed]
- Zheng W, Chow WH, Yang G, et al. The Shanghai Women's Health Study: rationale, study design, and baseline characteristics. Am J Epidemiol 2005;162:1123-31. [Crossref] [PubMed]
- Shu XO, Yang G, Jin F, et al. Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women's Health Study. Eur J Clin Nutr 2004;58:17-23. [Crossref] [PubMed]
- Villegas R, Yang G, Liu D, et al. Validity and reproducibility of the food-frequency questionnaire used in the Shanghai men's health study. Br J Nutr 2007;97:993-1000. [Crossref] [PubMed]
- Matthews CE, Shu XO, Yang G, et al. Reproducibility and validity of the Shanghai Women's Health Study physical activity questionnaire. Am J Epidemiol 2003;158:1114-22. [Crossref] [PubMed]
- Jurj AL, Wen W, Xiang YB, et al. Reproducibility and validity of the Shanghai Men's Health Study physical activity questionnaire. Am J Epidemiol 2007;165:1124-33. [Crossref] [PubMed]
- Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000;32:S498-504. [Crossref] [PubMed]
- Wang H, Zhai F. Programme and policy options for preventing obesity in China. Obes Rev 2013;14 Suppl 2:134-40. [Crossref] [PubMed]
- Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci 2002;15:245-52. [PubMed]
- Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet 2005;366:1059-62. [Crossref] [PubMed]
- Li HL, Fang J, Zhao LG, et al. Personal characteristics effects on validation of self-reported type 2 diabetes from a cross-sectional survey among Chinese adults. J Epidemiol 2020;30:516-21. [Crossref] [PubMed]
- Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum 1953;9:531-41. [PubMed]
- Dahlqwist E, Zetterqvist J, Pawitan Y, et al. Model-based estimation of the attributable fraction for cross-sectional, case-control and cohort studies using the R package AF. Eur J Epidemiol 2016;31:575-82. [Crossref] [PubMed]
- Astrup A, Finer N. Redefining type 2 diabetes: 'diabesity' or 'obesity dependent diabetes mellitus'?. Obes Rev 2000;1:57-9. [Crossref] [PubMed]
- Steppan CM, Bailey S-T, Bhat S, et al. The hormone resistin links obesity to diabetes. Nature 2001;409:307-12. [Crossref] [PubMed]
- Gurka MJ, Vishnu A, Santen RJ, et al. Progression of Metabolic Syndrome Severity During the Menopausal Transition. J Am Heart Assoc 2016;5:e003609. [Crossref] [PubMed]
- Janssen I, Powell LH, Crawford S, et al. Menopause and the metabolic syndrome: the Study of Women's Health Across the Nation. Arch Intern Med 2008;168:1568-75. [Crossref] [PubMed]
- Hosseinpanah F, Rambod M, Azizi F. Population attributable risk for diabetes associated with excess weight in Tehranian adults: a population-based cohort study. BMC Public Health 2007;7:328. [Crossref] [PubMed]
- Xue H, Wang C, Li Y, et al. Incidence of type 2 diabetes and number of events attributable to abdominal obesity in China: A cohort study. J Diabetes 2016;8:190-8. [Crossref] [PubMed]
- Tanamas SK, Permatahati V, Ng WL, et al. Estimating the proportion of metabolic health outcomes attributable to obesity: a cross-sectional exploration of body mass index and waist circumference combinations. BMC Obes 2016;3:4. [Crossref] [PubMed]
- Bennett DA, Du H, Bragg F, et al. Physical activity, sedentary leisure-time and risk of incident type 2 diabetes: a prospective study of 512 000 Chinese adults. BMJ Open Diabetes Res Care 2019;7:e000835. [Crossref] [PubMed]
- Fallahzadeh H, Ostovarfar M, Lotfi MH. Population attributable risk of risk factors for type 2 diabetes; Bayesian methods. Diabetes Metab Syndr 2019;13:1365-8. [Crossref] [PubMed]
- Al Tunaiji H, Davis JC, Mackey DC, et al. Population attributable fraction of type 2 diabetes due to physical inactivity in adults: a systematic review. BMC Public Health 2014;14:469. [Crossref] [PubMed]


