Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer
Introduction
Currently, lobectomy is the prior intervention to treat early-stage non-small cell lung cancer (NSCLC) (1). As a minimally invasive technique, thoracoscopic lobectomy has been widely used in thoracic surgery (2). Although single-port complete thoracoscopic lobectomy has been introduced to treat NSCLC, no literature was available as to compare its feasibility and safety with triple-port complete thoracoscopic lobectomy. Our operation team performed the first one of single-port complete thoracoscopic lobectomy in May 2014. After the preliminary exploration of 20 cases of surgery, we can coordinate by tacit agreement and the operation time tended stably. Then, we conducted a retrospective comparison study between single-port and triple-port complete thoracoscopic lobectomy for NSCLC enrolled from August 2014 to October 2014 to investigate the feasibility and safety of single-port complete thoracoscopic lobectomy.
Methods and materials
General information
A total of 82 patients with NSCLC who underwent complete thoracoscopic lobectomy from August 2014 to October 2014 in Department of Thoracic Surgery, Fujian Medical University Union Hospital were included in this retrospective study. There were 33 cases in single-port complete thoracoscopic lobectomy group (single-port group) and the other 49 ones in triple-port complete thoracoscopic lobectomy group (triple-port group). The selection criteria between single-port and triple-ports were not special or different. All patients underwent associated examinations such as thoracic computed tomography (CT), cerebral magnetic resonance imaging (MRI), skeletal emission computed tomography (ECT), and abdominal and cervical color Doppler ultrasound (CDU). Positron emission tomography-CT (PET-CT) might also need to be conducted when routine exam can’t make sure to rule out the underlying metastasis. Electrocardiogram, cardiac CDU, and pulmonary function test were applied to assess cardiopulmonary function. The inclusion criteria include: (I) the patients with clinical TNM stage I-II NSCLC; (II) no thoracic surgery history; (III) the patients’ cardiopulmonary function test reveal that the lobectomy is workable (The patient have the FEV1 1.0 L and MVV 40% in the pulmonary function test as least, while the cardiac CDU show no structure deficiency. Exercise testing as well used in judging the cardiopulmonary function by more than two floors); (IV) preoperative comorbidities have been stably controlled.
Anesthesia and surgical procedure
All patients were given general anesthesia. Double-lumen endobronchial tubes (DLT) intubed in both groups, and the one lung ventilated. For single-port group, a 3.5-4.5 cm incision was made on the 4th or 5th intercostal space along the anterior axillary line. For triple-port group, a 1.5 cm observation port was on the 7th intercostal space of midaxillary line, a 2.0-4.0 cm operation port was on the 4th intercostal space of anterior axillary line and a 1.5-2.5 cm vice-operation port was on the 7th intercostal space of scapular line. For peripheral lesions, pulmonary wedge resection was conducted to remove the focus. Once the resection samples were confirmed as malignant tumor by fast frozen pathology, the following standard lobectomy and mediastinal lymphadenectomy would be employed. For central lesions, lobectomy was conducted. After confirmed as malignant one, the following mediastinal lymphadenectomy would be employed. Electrocautery and ultrasonic scalpel were used to distract the vessels and bronchus. Linear stapler was used to deal with the great vessels such as pulmonary veins, pulmonary artery and so on. No definite order was made to conduct the lobectomy, which mostly depended on the development of interlobar fissure. Analgesia pumps were used for the two groups. There were no drug addiction patients. We have no previous medication. The patients’ intra-operative and post-operative pain management was the same. And all the patients were given the same vein analgesic protocol, and the POP-VAS score was asked by the same anesthetist. The POP-VAS score ‘0’ means no pain, and the ‘10’ great pain. Indications for withdrawing the chest drainage (without vacuum) included: (I) 24 h drainage volume was less than 100 mL; (II) postoperative chest X-ray show that the left lung recruitment, and no effusion deposited. The discharge criteria in our study were that the patients recovered to normal mobility status, without obvious fever, after withdrawing the chest drainage.
Observation data
The observation data included: (I) perioperative parameters: operation time, estimated blood loss, chest drainage duration, POP-VAS, postoperative hospital stay and perioperative complications; (II) oncologic outcomes: total lymph node harvest, positive lymph node, total mediastinal lymph node harvest, and dissection of mediastinal lymph node groups .
Statistical analysis
Statistical software SPSS 16.0 was conducted to analyze the data. Quantitative data was showed as mean ± standard deviation, and independent t-test was used to test the group comparisons. Enumeration data was presented as rate, and chi-square test was compared. Statistical significance was set as P<0.05.
Results
Clinical characteristics
There were no significant differences in sex, age, tumor location, pathological type, tumor invasion, visceral pleura invasion, and tumor classification between the two groups (P>0.05, Table 1). In addition, there were no significant differences in total lymph node harvest, positive lymph node, total mediastinal lymph node harvest, and dissection of mediastinal lymph node groups (P>0.05, Table 2).
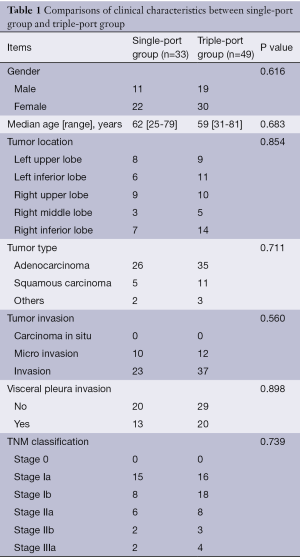
Full table
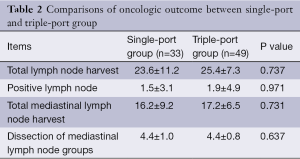
Full table
Perioperative parameters
All patients underwent the complete video-assisted thoracoscopic lobectomy without conversion to open thoracotomy. No patient deaths occurred during perioperative period in either group. However, there were a total of eight cases with postoperative complications, three cases (one case of arrhythmia, one case of systemic infection and one case of air leakage) in single-port group (9.1%), and another five cases (two case of arrhythmia, one case of air leakage, one case of chylothorax and one case of pneumonia) in triple-port group (10.2%). There were no significant differences in complications between the two groups (P>0.05). Additionally, no significant differences in intraoperative blood loss, postoperative chest drainage duration and postoperative hospital stay were observed (P>0.05). However, operation time in single-port group was longer than that in triple-port group (181.3±27.5 vs. 149.5±30.9 min, P<0.05). In this study, all patients need frozen section and it occupied about 30 min. POP-VAS in single-port group was lower than that in triple-port group (3.6±0.7 vs. 5.5±1.0, P<0.05). The summary information was included in Table 3.
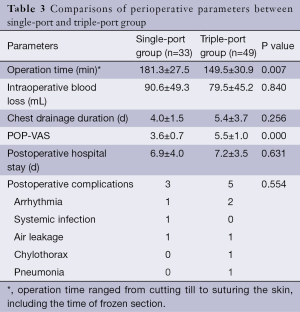
Full table
Discussion
Single-port thoracoscopic technique was first described to management non-complicated pleura-related disease in 2003 (3). In 2004, it was reported in pulmonary wedge resection by Rocco (4). Several years later, Gonzalez applied it in lobectomy and lymphadenectomy (5). Since then, it was applied gradually in pulmonary segmentectomy, pneumonectomy, bronchial sleeve resection and angioplasty of pulmonary arteries (6-9). However, most available literature focused on the feasibility and safety of single-port thoracoscopic lobectomy, and no studies compared those with triple-port one. The presented study retrospectively investigated the differences of clinical data between single-port thoracoscopic lobectomy and triple-port thoracoscopic lobectomy for NSCLC. Jiang compared 160 thoracoscopic lobectomies with 247 conventional open surgeries, they found no significant differences in perioperative mortality (0.6% vs. 2.8%) and complications (9.4% vs. 11.7%, P>0.05) (10). It indicated that thoracoscopic lobectomy was technically safe to treat NSCLC. Similarly in our study, the postoperative complications rates were 9.1% and 10.2% for single-port group and triple-port group respectively. However, it was no perioperative mortality in our study. Therefore, our study could conclude that single-port lobectomy was at least technically safe as well as the triple-port group.
The important focus of single-port thoracoscopic lobectomy used in treating NSCLC was on the dissection of lymph node. Jiang found no significant differences in dissection of mediastinal lymph node groups (2.4±1.5 vs. 2.6±1.6) and mediastinal lymph node harvest (9.8±6.2 vs. 9.9±5.9) between thoracoscopic lobectomy group and conventional open surgery group (P>0.05) (10). Similarly, Zhang et al. found no significant differences in total lymph node harvests (14.6±7.5 vs. 15.2±4.5) between video-assisted thoracoscopic surgery group and video-assisted thoracoscopy group (11). That was to say, the lymph node dissection by thoracoscopy was at least equivalent to that by open surgery. In the presented study, there were no significant differences in total lymph node harvest (23.6±11.2 vs. 25.4±7.3), mediastinal lymph node harvest (16.2±9.2 vs. 17.2±6.5), and dissection of mediastinal lymph node groups (4.4±1.0 vs. 4.4±0.8) between the single-port group and triple-port group. These results suggested that the lymph node harvest was not less than that reported in the previous studies. In other words, the dissection of lymph node by single-port thoracoscopic lobectomy met the oncologic require. However, the long-term outcomes need further studies to confirm.
The incision of single-port thoracoscopic lobectomy was located on 4th or 5th intercostal space along anterior axillary line, which, unlike triple-port one, canceled the observation port and vice-operation port. After comparing 20 cases of triple-port and 10 cases of single-port thoracoscopic surgery in treating interstitial lung disease, Chen et al. found that POP-VAS in single-port group was significantly lower than that in triple-port group (4.95±0.39 vs. 4.5±0.7, P=0.03) (12). Similarly in our study, POP-VAS in single-port group was significantly lower than that in triple-port group (3.6±0.7 vs. 5.5±1.0, P<0.05).
In the presented study, the operation time in single-port group was significantly longer than that in triple-port group (181.3±27.5 vs. 149.5±30.9 min, P<0.05). The reasons included: (I) all the operating instruments and thoracoscopy went through the single port, which might interfere each other, especially when the focus located near the dorsal cavity and diaphragm; (II) single-port thoracoscopic lobectomy had a strict skill requirement of qualified camera assistant to accommodate the geometrical changes of uniportal VATS (13). The camera assistant was supposed to know how to cooperate with the operator, how to allocate the space within the incision, and how to keep the camera stable. However, we believed that the operation time would be shortened with the improvement of operating instruments which can better suit single-port operation.
In summary, the feasibility and safety of single-port thoracoscopic lobectomy were similar to triple-port thoracoscopic lobectomy for NSCLC. With the development of instruments, the optimization of surgical procedure, and the accumulation of surgical experience, the operation time would likely be shortened gradually. At that time, single-port complete thoracoscopic lobectomy was supposed to be popularized with its merits of minimal invasiveness.
Acknowledgements
Authors’ contributions: Y Zhu and M Liang are co-first authors, and they made equal contributions to the work. C Chen designed the study. W Wu, J Zheng, B Zheng, and G Xu participated in the data-collection part of this research. W Zheng and Z Guo participated in all the operations. All authors read and approved the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Shigemura N, Akashi A, Funaki S, et al. Long-term outcomes after a variety of video-assisted thoracoscopic lobectomy approaches for clinical stage IA lung cancer: a multi-institutional study. J Thorac Cardiovasc Surg 2006;132:507-12. [PubMed]
- Wu W, Chen C, Lin R, et al. Complete Video-assisted thoracic surgery lobectomy: Clinical Analysis of 32 Cases. Journal of Fujian Medical University 2010;44:49.
- Migliore M. Efficacy and safety of single-trocar technique for minimally invasive surgery of the chest in the treatment of noncomplex pleural disease. J Thorac Cardiovasc Surg 2003;126:1618-23. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [PubMed]
- Jiang W, Xi J, Wang Q, et al. Complete Video-assisted Thoracoscopic Surgery versus Open Mediastinal Lymphadenectomy for Non-small Cell Lung Cancer. Chinese Journal of Minimally Invasive Surgery 2012;12:969-72.
- Zhang T, Yu L, Jiang J, et al. Video-assisted Thorascopic Lymphadenectomy for Non-small Cell Lung Cancer. Chinese Journal of Minimally Invasive Surgery 2009;9:696-9.
- Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg 2011;6:58. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]


