
Novel method for diagnosing lateral patellar compression syndrome using X-ray: a retrospective case-control study
Introduction
Lateral patellar compression syndrome (LPCS) covers a series of clinical symptoms and signs and is caused by an abnormal increase in lateral patellofemoral joint pressure. This occurs with the long-standing lateral inclination of the patella without dislocation, adaptive shortening of the lateral retinaculum, and chronic stress imbalance between the internal and external articular surfaces. Its pathogenesis mainly involves increasing lateral stress on the patella (1-5), with patellar cartilage injury and patellofemoral joint pain being the most important pathological change (6) and most common manifestation, respectively (5).
Because the etiology and pain mechanism of LPCS is complex and diverse, it is very difficult and controversial to accurately describe its clinical symptoms and establish definite diagnostic criteria. To date, no well-established reference for diagnosis exists. Currently, its diagnosis mainly depends on the subjective judgment of clinicians and several examination results (7-11).
Examination methods including X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and arthroscopy are used in diagnosing LPCS. Although CT can measure the position of the patella, it is inadequate to evaluate the damage of the patellar joint surface in the early stage and is thus unable to evaluate the treatment effect. Moreover, the amount of radiation exposure to patients in CT is 10 times that of X-ray. Arthroscopy can precisely diagnose articular cartilage injury. However, it is an invasive procedure and is unable to detect early-stage articular cartilage lesions (12). MRI has the advantage of stereoscopic evaluation of the joint structure in high resolution. Compared with the other methods, it is the most advanced imaging method for diagnosing and monitoring LPCS (13). However, its sensitivity for patellofemoral joint lesions in LPCS is only 70% (14), and some new technologies such as gradient echo can achieve 90% sensitivity (15). Moreover, MRI is not suitable as the first choice of examination; thus, X-ray diagnosis and its derivatives are still the first choice (16).
Although knee joint X-rays are primarily used to diagnose LPCS, their detection rate of patellar tilt by measuring the congruence angle (CA) and patellar tilting angle (PTA) is low. Currently, its detection rate for patellar tilt by using PTA is approximately 70–80% (17). Some studies suggest that the narrow space of the lateral patellofemoral joint can be easily demonstrated on axial patellar radiographs along with the following features: bone volume on the medial joint surface, sclerosis of the subchondral bone on the lateral joint surface, and development of osteophytes on the lateral joint surface. These radiographs show unique advantages in detecting early patellofemoral arthropathy, patellar displacement, tilt, and dislocation (18-20).
We investigated whether the lateral patellar curvature angle (LPCA) measured on axial patellar radiograph of the knee in 30° flexion can be used as a new index for diagnosing LPCS. We enrolled patients with LPCS, meniscus tear (MT), and patellar dislocation (PD) because they show the clinically similar symptom of anterior knee pain. The differences in imaging parameters including CA, PTA, and LPCA were analyzed among these three groups using axial patellar radiography. We thus explored the significance of relevant indicators in the diagnosis of LPCS, and the study results may provide guidance and a reference for the clinical diagnosis of LPCS.
We present the following article in accordance with the STARD reporting checklist (available at http://dx.doi.org/10.21037/atm-20-6410).
Methods
Study participants
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of Hospital (IRB00006761-M2019464) approved our study, and the ethics committee exempted the study from requiring informed consent from study participants. We enrolled 87 eligible volunteers from the Institute of Sports Medicine between February 2016 and April 2019. They were divided into the following three groups of 29 each as per diagnosis: LPCS, PD, and MT groups. They were diagnosed after therapeutic surgery by doctors from the same department, with all surgeries being unilateral and with 87 knees in total.
LPCS diagnosis
LPCS was jointly diagnosed by the surgeon and the medical team leader after thoroughly examining symptoms, signs, and results of physical examination, imaging analyses, and intraoperative arthroscopy. For diagnosis, the following manifestations were examined: (I) persistent anterior knee pain aggravated by stress on the patellofemoral joint. (II) The lateral margin or lateral retinaculum showing limited tenderness points on physical examination along with positive patellar grinding and patella elution tests. (III) Imaging examination demonstrating lateral inclination of the patella; narrowed lateral patellofemoral joint space on X-ray, CT, and MRI; and MRI T1β showing contracture and tapering of the lateral retinaculum and degenerative changes in the patellofemoral articular cartilage (3,8,9).
Inclusion criteria of LPCS group
LPCS was confirmed based on the aforementioned examination and findings of arthroscopy, symptoms of knee joint pain, and unilateral knee joint lesions.
Exclusion criteria of LPCS group
The exclusion criteria were as follows: patients with meniscal injury, ligament injury, malunion of patella fracture, free bodies in the joint, surgical contraindications, and with both knees affected.
Inclusion criteria of MT group
MT was confirmed based on MRI and arthroscopic findings, symptoms of pain and swelling of the knee joint, and unilateral knee joint lesions.
Exclusion criteria of MT group
Patients with a history of knee surgery; severe osteoporosis (according to Chinese diagnostic criteria); severe heart, liver, kidney, and other organ dysfunction; and rheumatoid arthritis or knee osteoarthritis were excluded from the MT group.
Inclusion criteria of PD group
PD was confirmed by combining medical history, signs, and radiographic findings; lateral dislocation of patella; and unilateral knee joint lesions.
Exclusion criteria for PD group
Patients with previous knee surgery or collateral ligament injury and rheumatoid arthritis were excluded from this group.
Method of patellar axial radiography
Both the case group and control groups underwent patellar axial radiography for both knees in 30° flexion. The radiographs were taken by a radiologist in accordance with standard operating procedures as follows: the knee joint was placed on a frame and was flexed at 30°, the lower limb muscles were relaxed, and the ball tube passed through the patellofemoral joint at a tangent to the foot. The imaging indexes on from these axial films were analyzed.
Image analyses
A senior radiologist and the chief physician of sports medicine used the hospital imaging system to repeatedly measure the following imaging indexes on the images for 87 patients according to a unified procedure.
Main observation indicators
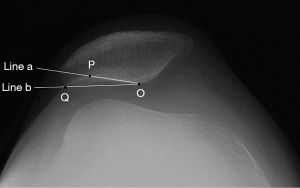
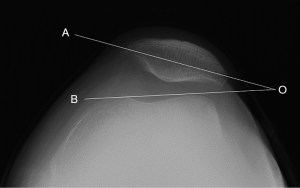
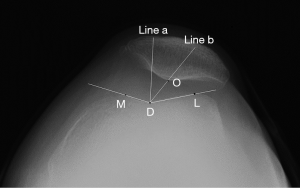
For measuring LPCA, two tangents were drawn at a tangent to the lateral articular surface of the patella from the lowest point O of the middle patellar ridge. A is the tangency from medial to lateral, and P is the tangency point. B is the tangency from lateral to medial, and its tangent point is Q (Figure 1). To measure PTA, we measured the angle between the line passing through the widest transverse axis of the patella and the line passing through the medial and lateral condyles of the femur. In the normal population, PTA is 11.0°±2.5° and should not be greater than 15° (21), which is an important index to diagnose PD (22) (Figure 2). To measure CA, we first drew the angle made by connecting the highest point of the medial and lateral condyles of femur with the lowest point of the trochlear groove of femur; we then divided the trochlear angle equally and drew the second line to connect the lowest point of the intermediate ridge of the patella to the lowest point of the trochlear groove of the femur. The angle between these two lines was the CA. CA is −8°±9° in healthy people and >16° in patients with lateral patella dislocation (23) (Figure 3).
Sample estimation
We measured LPCA in 39 patients before the study and calculated the area under the curve (AUC). We then estimated the required sample size for the cases and controls to be 29 and 58, respectively.
Statistical analysis
Measurement data are summarized as mean ± standard deviation. Univariate analysis of variance was used for the comparison of measurement data with normal distribution. The Kruskal-Wallis H test was used for comparison of measurement data with non-normal distribution. Bonferroni correction was used to analyze different indicators for different groups, and the T-test was used for index comparison within the same group. The interference of sex can be eliminated by comparing the difference in the same index in different sexes. The counting data are described as rates (percentages) and were compared using the chi-square test. We used SPSS 21.0 for statistical analysis of the data and MedCalc v19.0.7 was used for calculating the area under the receiver operating characteristic (ROC) curve. Statistical significance was set at P<0.05.
Results
Basic information
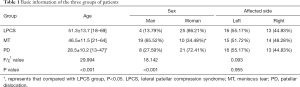
Among the 87 patients (31 men and 56 women; mean age: 42.11±15.33 years; age range: 13–69 years), no differences were observed on the affected side between the three groups (P=0.955). The age in the LPCS group was significantly higher than that in the PD group (P<0.001). A significant difference in sex was observed between the LPCS and MT groups (P<0.001) (Table 1).
Full table
Previous reports suggest that PD and LPCS are more common in adolescents (24) and older people, respectively (5,25). The sex of patients in the three groups was not completely matched. No significant sex difference in the indexes was observed in this study (P>0.05), which could eliminate sex as a confounding factor.
Comparison of imaging indexes on axial patellar radiographs between three groups
The Kruskal-Wallis H test showed significant differences among the three imaging indexes within the groups (P<0.001). No differences were observed in PTA between the LPCS and MT groups (P=0.576) or in CA between the LPCS and PD groups (P=0.451). Moreover, LPCA in the LPCS group was higher than that in the other two groups (P<0.01) (Table 2).
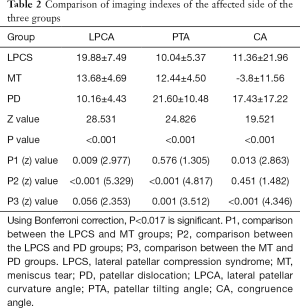
Full table
Comparison of LPCA between healthy and affected sides in the three groups
No differences were observed in LPCA between the healthy and affected sides in the MT and PD groups (paired T-test, P>0.05), whereas the LPCS group showed significant differences between the sides (paired T-test, P=0.04; Table 3).

Full table
Comparison of imaging indexes between healthy and affected sides of the LPCS group
The paired T-test showed no difference in PTA and CA between the healthy and affected sides in the LPCS group (P>0.05); however, LPCA on the affected side was higher than that on the healthy side in the LPCS group (P=0.04) (Table 4).

Full table
ROC curve of LPCA
To confirm the value of LPCA in the diagnosis and differential diagnosis of LPCS, an ROC analysis of the three imaging indexes was performed. The patients in the LPCS group were classified as the positive group, and the patients in the MT and PD groups were the negative group.
The AUC of LPCA was the largest, as observed in Table 5. The analysis showed that an LPCA of >13.9° determined the presence of LPCS with sensitivity and specificity of 89.66% (26 of 29) and 68.97% (40 of 58), respectively (AUC: 0.82, 95% confidence interval: 0.719–0.891, P<0.001).
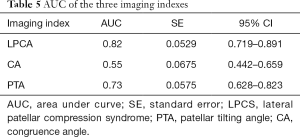
Full table
Discussion
The results of our study showed that LPCA in the LPCS group was significantly higher than that in the other two groups; the AUC of LPCA in the initial screening of LPCS was higher than that of PTA and CA.
PD is a common disease that needs to be differentiated from LPCS. It is characterized by blunt pain around the patellofemoral joint and has a higher incidence in women (24). Although its symptoms and X-ray manifestations are similar to those of LPCS, its pathogenesis is different. Therefore, it is typically used as a control group.
MT is also a common knee disease requiring surgery; however, it does not usually demonstrate a clear patellar abnormality. MTs without patellofemoral cartilage damage and patellar chondromalacia (26) are easily identified using MRI. Therefore, it is classified as a negative control group.
Although an X-ray of the knee joint is the most basic method for diagnosing LPCS, the detection rate of patellar tilt by calculating CA and PTA is low. We hoped that LPCS can be diagnosed more quickly and accurately through the axial patellar radiograph. Therefore, we examined the axial patellar radiographs of several patients with LPCS and found a unique imaging feature. The lateral articular surface of patella is deeper and more curved than that in normal people because of osteophyte formation and patellar malacia. Hence, we thought of using the new index LPCA to measure this rare characteristic, that is, the curvature of the affected lateral articular surface of the patella.
We think that LPCA can be used to evaluate the degree of deformity and osteophyte formation of the lateral patellar articular surface, thus aiding the diagnosis of LPCS. Our results showed that LPCA was significantly higher in the LPCS group than in the other two groups. This demonstrated a relatively obvious deformity of the lateral patellar articular surface consistent with the pathological characteristics of patellar malacia in LPCS (6).
The AUC of LPCA was the largest. Moreover, the positive value of LPCA was higher than its negative value when preliminary screening for LPCS was performed.
Limitations
This study has limitations. The patients’ age and sex are not matched, and the new index is lack of comparing the case group and normal population. Technical limitations may have led to errors with the manual measurement of data. The imaging indexes of our study require high-quality X-ray films, especially for axial X-ray films.
Conclusions
In our study, we demonstrated that LPCA measured using an axial patellar radiograph of the knee in 30° flexion is high in patients with LPCS, and it may be used for diagnosing LPCS.
Acknowledgments
Thank you to Wallace for academic editorial services.
Funding: This study was funded by National Key Research and Development Program of China (2019YFF0302305); 2020 Zhangjiakou Science and Technology Winter Olympics technology integration application and comprehensive demonstration project (Number: 20110004D). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-6410
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-6410
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-6410). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by The Ethics Committee of Hospital (No: IRB00006761-M2019464) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nelitz M, Theile M, Dornacher D, et al. Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc 2012;20:822-8. [Crossref] [PubMed]
- Kramer PG. Patella malalignment syndrome: rationale to reduce excessive lateral pressure. J Orthop Sports Phys Ther 1986;8:301-9. [Crossref] [PubMed]
- Wu T, Tang S, Wang F. Treatment for lateral patellar impingement syndrome with arthroscopic lateral patelloplasty: a bidirectional cohort study. J Orthop Surg Res 2017;12:173. [Crossref] [PubMed]
- Petersen W, Ellermann A, Gösele-Koppenburg A, et al. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc 2014;22:2264-74. [Crossref] [PubMed]
- Chen JB, Chen D, Xiao YP, et al. Efficacy and experience of arthroscopic lateral patella retinaculum releasing through/outside synovial membrane for the treatment of lateral patellar compression syndrome. BMC Musculoskelet Disord 2020;21:108. [Crossref] [PubMed]
- Chhabra A, Subhawong TK, Carrino JA. A systematised MRI approach to evaluating the patellofemoral joint. Skeletal Radiol 2011;40:375-87. [Crossref] [PubMed]
- Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med 2002;30:447-56. [Crossref] [PubMed]
- Jeong JH, Chang MJ, Kang SB, et al. Prevalence of excessive lateral pressure syndrome in varus osteoarthritic candidates for high tibial osteotomy. Knee 2018;25:1192-6. [Crossref] [PubMed]
- Saper MG, Shneider DA. Diagnosis and treatment of lateral patellar compression syndrome. Arthrosc Tech 2014;3:e633-8. [Crossref] [PubMed]
- Merchant AC, Fulkerson JP, Leadbetter W. The Diagnosis and Initial Treatment of Patellofemoral Disorders. Am J Orthop (Belle Mead NJ) 2017;46:68-75. [PubMed]
- Rothermich MA, Glaviano NR, Li J, et al. Patellofemoral pain: epidemiology, pathophysiology, and treatment options. Clin Sports Med 2015;34:313-27. [Crossref] [PubMed]
- Gross KD, Niu J, Stefanik JJ, et al. Breaking the Law of Valgus: the surprising and unexplained prevalence of medial patellofemoral cartilage damage. Ann Rheum Dis 2012;71:1827-32. [Crossref] [PubMed]
- Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med 2011;45:691-6. [Crossref] [PubMed]
- Sillanpää PJ, Salonen E, Pihlajamäki H, et al. Medial patellofemoral ligament avulsion injury at the patella: classification and clinical outcome. Knee Surg Sports Traumatol Arthrosc 2014;22:2414-8. [Crossref] [PubMed]
- Tompkins M, Kuenze CM, Diduch DR, et al. Clinical and Functional Outcomes following Primary Repair versus Reconstruction of the Medial Patellofemoral Ligament for Recurrent Patellar Instability. J Sports Med (Hindawi Publ Corp) 2014;2014:702358 [Crossref] [PubMed]
- Hafezi-Nejad N, Demehri S, Guermazi A, et al. Osteoarthritis year in review 2017: updates on imaging advancements. Osteoarthritis Cartilage 2018;26:341-9. [Crossref] [PubMed]
- Berruto M, Ferrua P, Carimati G, et al. Patellofemoral instability: classification and imaging. Joints 2013;1:7-14. [PubMed]
- Merchant AC. Patellofemoral imaging. Clin Orthop Relat Res 2001;15-21. [Crossref] [PubMed]
- Merchant AC, Mercer RL, Jacobsen RH, et al. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 1974;56:1391-6. [Crossref] [PubMed]
- Sanders TL, Pareek A, Johnson NR, et al. Patellofemoral Arthritis After Lateral Patellar Dislocation: A Matched Population-Based Analysis. Am J Sports Med 2017;45:1012-7. [Crossref] [PubMed]
- Goshima K, Sawaguchi T, Shigemoto K, et al. Patellofemoral Osteoarthritis Progression and Alignment Changes after Open-Wedge High Tibial Osteotomy Do Not Affect Clinical Outcomes at Mid-term Follow-up. Arthroscopy 2017;33:1832-9. [Crossref] [PubMed]
- Alaia MJ, Cohn RM, Strauss EJ. Patellar instability. Bull Hosp Jt Dis (2013) 2014;72:6-17. [PubMed]
- Suganuma J, Mochizuki R, Sugiki T, et al. Reconstruction of the Medial Patellofemoral Ligament Using a Synthetic Graft With Arthroscopic Control of Patellofemoral Congruence. Arthroscopy 2016;32:2259-68. [Crossref] [PubMed]
- Vetrano M, Oliva F, Bisicchia S, et al. I.S.Mu.L.T. first-time patellar dislocation guidelines. Muscles Ligaments Tendons J 2017;7:1-10. [Crossref] [PubMed]
- Smith BE, Selfe J, Thacker D, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PloS one 2018;13:e0190892-e.
- Nguyen JC, De Smet AA, Graf BK, et al. MR imaging-based diagnosis and classification of meniscal tears. Radiographics 2014;34:981-99. [Crossref] [PubMed]


