Laparoscopic radical gastrectomy for gastric cancer: traps and strategies
Introduction
Surgeries remain the mainstream treatment for gastric cancer. Early in 1991, Kitano et al. conducted the first laparoscopy-assisted distal gastrectomy for treating early gastric cancer. In the past two decades, the surgical techniques have become more mature, along with increased surgical indications and lower incidences of surgery-related complications. However, due to the rich blood supply, multiple anatomic levels, complex lymph node dissection, and special requirements of the laparoscopy itself, this surgery is quite difficult and has high technical requirements. During the laparoscopic radical gastrectomy, it is equally important to achieve the complete resection of the tumor and to ensure the surgical safety. As the laparoscopic radical gastrectomy has increasingly been applied, it has become a priority to pay special attention to the safety of this surgical technique, so as to avoid the occurence of severe complications. Based on literature review and clinical experiences, we elucidate the challenges and strategies of laparoscopic radical gastrectomy for gastric cancer.
Complications of laparoscopic radical gastrectomy for gastric cancer
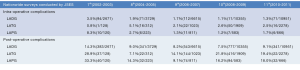
East Asia has the highest gastric cancer rates in the world. Also, the frequencies and types of the complications of the laparoscopic radical gastrectomy for gastric cancer were also similar among China, Japan, and Korea. According to a national survey conducted by the Japan Society of Endoscopic Surgery (JSES), 10,951 patients underwent laparoscopic radical gastrectomy for distal gastric cancer in 2010 and 2011, among whom the incidences of intra- and post-operative complications were 1.3% and 9.1%, respectively; 2,278 patients underwent laparoscopic total gastrectomy, among whom the incidences of intra- and post-operative complications were 2.5% and 19.4%, respectively; 666 patients underwent laparoscopic radical gastrectomy for proximal gastric cancer, among whom the incidences of intra- and post-operative complications were 1.7% and 18.0%, respectively (Figure 1). In a Korean retrospective study enrolling, 1,485 patients who had received laparoscopic radical gastrectomy for gastric cancer in 10 centers showed that the incidence of the surgery-related complications was 14.0%. The Chinese Laparoscopic Gastrointestinal Surgery Study (CLASS) group retrospectively analyzed 1,331 patients who had undergone laparoscopic radical gastrectomy in multiple centers and found the incidence of the surgery-related complications was 11.3%. Shanghai Ruijin Hospital also retrospectively analyzed 312 patients who had undergone laparoscopic radical gastrectomy and found the incidence of the surgery-related complications was 11.2%. Many retrospective studies and a few prospective studies with small sample sizes have demonstrated that the incidences of the laparoscopic radical gastrectomy-related complications are equal to those of open surgeries. Also, its pattern is also similar to that of open surgery. For example, the incidences of complications are higher after laparoscopic total gastrectomy than after radical distal gastrectomy, and are higher in patients with advanced gastric cancer than those with early gastric cancer. Thus, although the laparoscopic radical gastrectomy has been applied for treating gastric cancer for over 20 years, there are still some challenges to be addressed.
Lymph node dissection during laparoscopic radical gastrectomy for gastric cancer: challenges and strategies
Like the open surgery, the extent of lymph node dissection during the laparoscopic radical gastrectomy for gastric cancer must also follow certain rules. The Japanese gastric cancer treatment guideline (3rd edition) released by Japan in 2010 have been widely recognized as the most instructive documents in this field. In the document, the extent of lymph node dissection was dramatically changed. For the distal gastric cancer, the D1 was modified from the dissection of No. 3, 4d, 5, and 6 to the dissection of No. 1, 3, 4sb, 4d, 5, 6, and 7 (+ No. 1, 4sb and 7); for D2, the resected lymph nodes were changed from D1 + No.1, 7, 8a, 9, 11p, 12a, 14v to D1 + No. 8a, 9, 11p, and 12a (− No. 14v). The most common complication of the laparoscopic D2 lymphadenectomy for gastric cancer is intraoperative intraperitoneal hemorrhage. The following hemorrhage-prone sites are also the largest challenges during the surgery:
(I) Hemorrhage when dissociating the right gastroepiploic vein (RGEV): often due to the damage of the branches of the anterior superior pancreaticoduodenal vein (ASPDV) and subpyloric vein or the head of the pancreas. When handling RGEV from its root, dissection of No. 6 can easily damage the ASPDV and thus cause bleeding. ASPDV is typically small and prostrate at the pancreatic head and can retract back once being damaged, making the hemostasis particularly difficult. Improper hemostasis can hurt the head of the pancreas and even the right colic vein or Henle’s trunk, causing more severe bleeding. Thus, during the handling of RGEV, the fusion fascia between the descending part of duodenum and the mesentery of transverse colon should be dissociated firstly. Then, the middle colic artery can be used as a marker. It is always located at the middle-right of the mesentery of transverse colon, with obvious beating activity. With the middle colic artery as the marker, the anterior lobe of the mesentery of transverse colon was dissected upwards till the lower edge of the neck of pancreas, and then the Henle’s trunk can be visible. The Henle’s trunk usually is joined by RGEV, ASPDV, and accessory right colic vein. RGEV can be tracked along the Henle’s truck. Excessive skeletonization of this vein is unnecessary; instead, divide it after clamping with absorbable clips. Furthermore, after the division of RGEV, the lymphadenectomy along the surface of the head of the pancreas is somehow like an action of “climbing a hill”. RGEV is not closely accompanied by the right gastroepiploic artery (RGEA): the root of RGEV is often located at the lower edge of the head of the pancreas, and the root of RGEA is often close to the upper edge of the head of the pancreas. Thus, they need to be handled separately (Figure 2).
(II) Hemorrhage when dissociating the right gastric artery: the hemorrhage often occurs at the superior pancreaticoduodenal artery. Since the laparoscope can provide views from multiple angles, the operator can search for the root of the right gastric artery along the gastroduodenal artery and the proper hepatic artery and dissect the No. 5 lymph nodes, during which the superior pancreaticoduodenal artery between the duodenal bulb and the right gastric artery may be damaged. The superior pancreaticoduodenal artery often has two or three branches, and can not be clearly exposed even after the gastric antrum and duodenum are pulled upward. When it is particularly difficult to dissociate the right gastric artery backward, a frontwards approach may be adopted, which allows a more convenient and safer maneuver. In addition, during the backward division of the right gastric artery, the proper hepatic artery must be exposed firstly, so as to avoid the division of the circuitous proper hepatic artery as the right gastric artery by mistake.
(III) Hemorrhage after the spleen damage: hemorrhage is often occurs at the early stage of surgery and can be difficult to stop. It is often due to the rupture of the capsule of the spleen after the assistant pulls the greater omentum in an improper manner. Anatomically, the greater omentum often has membraneous fusions with the middle or lower capsules of the spleen. During the dissection of the No. 4sb lymph node, the assistant may excessively pull the greater omentum with an attempt to expose the dissection field more clearly; as a result, the tension at the fusion area becomes too large and thus the spleen capsule is torn. To prevent this situation from happening, the adhesions between the greater omentum with the left diaphragm/spleen capsule may be loosened before the dissection of No. 4sb lymph node, so that the dissection field can be easily and clearly exposed and meanwhile the risk of bleeding can be avoid. Another situation is: the last branch of the short gastric arteries may be extremely short in some patients. It may directly drain into the superior polar artery of the spleen. The stomach fundus is closely attached to the the upper pole of the spleen, resulting in the loss of the gap between stomach and spleen. Forceful traction by the assistant will cause the rupture of the vessel; once torn, the broken end is extremely difficult to manage, and any careless handling may lead to even heavier bleeding due to the injury of the upper pole of the spleen. If such condition occurs, it is more feasible to handle the posterior gastric artery firstly, then handle this condition after lifting the stomach fundus from the back side of the stomach; alternatively, open the the lining of the lower part of the esophagus and handle the condition after pulling the stomach fundus from the front to the lower right side.
(IV) Hemorrhage at the left gastric vein: left gastric vein, with some variations, can drain into the portal or splenic vein via the front/back side of the common hepatic artery or splenic artery. During the dissection of the lymph nodes on the upper edge of the pancreas, neglecting the anatomical variation of this vein may cause injury, resulting in massive bi-directional bleeding, which can affect the effective dissection of the lymph nodes on the upper edge of the pancreas. If the broken end retracts back after the injury, the handling will be even more difficult. Therefore, the operator must be familiar with the variations in the left gastric vein. During the exposure, the assistant need to maintain certain tension of the gastropancreatic fold but must avoid excessive traction. When an ultrasonic scalpel is used to dissect lymph nodes on the upper margin of the pancreas, tissue atomization and a small amount of capillary hemorrhage from the penetrating branches of the vein inside the lymph nodes may affect the visual field and operations of the operator. By using a small-flow intermittent suctioning technique, the assistant can clearly expose the surgical field and effectively avoid such injuries.
(V) Splenic hilar vascular hemorrhage: the No. 10 lymph node needs to be dissected during the radical total gastrectomy with D2 dissection (TG + D2). Laparoscopic spleen-conserving splenic hilar lymph node dissection is similar to the in situ splenic hilar lymph node dissection under open laparotomy in terms of surgical procedures. Nevertheless, the laparoscopy brings clearer and larger surgical field, the ultrasonic scalpel has better hemostatic effectiveness, and the surgical instruments can operate in deeper sites. All these features make the in situ splenic hilar lymph node dissection become possible under laparoscope. However, the splenic hilar area has complex vessels, deep location, and narrow space, which brings high risks of vascular injury and bleeding at the splenic pole and splenic lobes. Computed tomography angiography (CTA) should be performed before surgery to find out the course of the splenic artery and its relationship with the body and tail of the pancreas, learn the type of the terminal branches of the splenic artery, and identify the types of vessels in the splenic lobes. During the surgery, dissection of the pancreatic tissue by mistake will lead to postoperative pancreatic fistula. Also, injury of the terminal branches of the splenic artery will cause uncontrolable bleeding or splenic lobe ischemia. If hemorrhage occurs, the assistant shall assist the exposure with one hand; meanwhile, he/she shall perform small-flow intermittent suctioning with another hand, so as to expose the bleeding site. The operator should quickly and gently clamp the bleeding site with noninvasive grasping forceps to control bleeding; meanwhile, titanium clips should be applied to stop bleeding. In addition, the proper positioning of the operator is also very important. During the splenic hilar lymph node dissection, the operator can stand between patient’s legs, so as to facilitate the stable operations with the right hand. Also, this procedure should be performed by a fixed group with rich experiences in D2 laparoscopic radical resection for gastric cancer.
Digestive tract reconstruction during laparoscopic radical gastrectomy for gastric cancer: challenges and strategies
Digestive tract reconstruction is key to the success of laparoscopic radical gastrectomy for gastric cancer. Anastomotic leakage, haemorrhage, and stricture are the most common complications after the laparoscopic radical gastrectomy for gastric cancer. These three complications have common causes and are ofter correlated with each other. Digestive tract reconstruction after laparoscopic radical gastrectomy for gastric cancer is often performed using small incisions, whereas its procedures often refer to those used in conventional open surgery. However, these small incisions limit the visual field and may lead to excessive traction, thus resulting in anastomosis-related complications. It remains particularly problematic during the reconstruction after laparoscopic total gastrectomy.
(I) Digestive tract reconstruction after laparoscopic distal gastrectomy: small incision-assisted approaches are often used, with the most common surgical procedures including Billroth-I, Billroth-II, and Roux-en-Y reconstruction.
(i) Billroth-I reconstruction is recommended for tension-free anastomosis. It is easy to perform and physiologically most feasible. The incidences of postoperative complications such as reflux gastritis, dumping syndrome, malnutrition, and gall stones significantly reduced after the Billroth-I reconstruction. However, the blood supply of the anastomosis must be ensured. It can be affected by both the preservation (or not) of the short gastric vessels and posterior gastric vessels and the distance between the anastomosis and the gastric cutting line. If the Billroth-I reconstruction is applied for the anastomosis between the duodenal stump and the posterior wall of the remnant stomach, a 3-cm gap should be kept between the anastomosis and the gastric stump, so as to avoid anastomotic ischemia.
(ii) However, Billroth-I reconstruction is not feasible for anastomosis under tension. Billroth-II reconstruction will be applied instead. It is featured by tension-free anastomosis, easier performance, and smaller incisions. However, compared with Billroth-I reconstruction, it has higher incidence of complications. In particular, the leakage of the duodenal stump due to afferent loop obstruction and internal hernia must be repaired by a second surgery. Although the retrocolic anastomosis (or together with Braun anastomosis) can effectively lower the incidences of such severe complications, alkaline reflux gastritis and anastomosis inflammation will be unavoidable.
(iii) If the remnant stomach is relative small, the anastomosis has tension if treated with Billroth-I reconstruction, or the tumor is near the pylorus, we prefer to use the Roux-en-Y reconstruction instread. The Roux-en-Y reconstruction can create tension-free anastomosis and effectively lower the incidences of complications such as bile reflux, residual gastritis, anastomotic leakage, and anastomotic stricture. It may also be helpful in treating type 2 diabetes mellitus. However, the Roux-en-Y reconstruction also has some limitations. In particular, it may lead to Roux stasis syndrome, which is manifested by vomiting of food but not bile, postprandial pain, and nausea. For these patients, indwelling of gastric tube and “wait and see” will help to achieve self healing. Smaller remnant stomach and shorter Roux loop are effective prevention strategies. In our practices, we have shortened the length of the Roux loop from 40 to 30 cm, which effectively lowers the incidence of Roux stasis syndrome.
In 2002, Kanaya et al. for the first time discribed the application of Delta-shaped anastomosis in totally laparoscopic D2 radical distal gastrectomy, during which the endoscopic cutter stapler is used to complete the Billroth-I reconstruction. As a rationally designed method, it has larger inner diameter of the anastomosis, shorter reconstruction duration, and lower incidence of anastomotic leakage. As a safe and relatively easy Billroth-I reconstruction for totally laparoscopic surgeries, it is worthy of our reference. For instance, during the stomach-jejunum Roux-en-Y anastomosis, we prefer to employ an iso-peristaltic method, during which the common entry was sutured artificially; however, it is often difficult if performed totally under laparoscopy. In recent years, we begin to apply an anti-peristaltic method instead, during with the common entry is closed using the linear stapler totally under laparoscopy. It is an easy and safe procedure, and can be a useful anastomosis totally under laparoscopy.
(II) Digestive tract reconstruction after laparoscopic proximal gastrectomy: laparoscopic proximal gastrectomy is feasible for treating upper gastric cancer (Ia stage) and early gastric cancer (Ib stage, sized <2 cm). For these conditions, the digestive tract reconstruction is mainly applied for residual stomach-esophagus anastomosis using small incisions. Although the end-to-side anastomosis between the esophagus and the anterior wall of remnant stomach is simple, less time-consuming, and physiologically feasible and has a low incidence of anastomotic leakage, the high incidence of postoperative reflux esophagitis remains a big challenge. Some patients may complain of obvious retrosternal burning sensation, and a second surgery will be needed in severe cases. Therefore, although the laparoscopic proximal gastrectomy may preserve the physiological functions of some remnant stomach and the patients may benefit from quicker body weight gain and better nutrition status, many surgeons still prefer to perform total gastrectomy. In recent years, we have employed the esophagus-tubular stomach anastomosis, which can remarkably lower the incidence of reflux esophagitis. During the tubular gastroplasty, the right gastro-omental artery and vein as well as the distal branch of the right gastric artery are preserved; an anvil was placed after the esophagus was transected; a tubular stomach (15-20 cm in length and 3-4 cm in width) was made from the remnant greater curvature of stomach using the linear stapler. The pyloric canal must be preserved. The end-to-side anastomosis between the esophagus and the anterior wall of the tubular stomach was performed using a circular stapler. Since it has a single anastomosis and the operation is quite simple under the assistance of small incisions, this reconstruction been regarded as an effective method for preventing postoperative reflux esophagitis.
(III) Digestive tract reconstruction after laparoscopic total gastrectomy: during the laparoscopic total gastrectomy, the exposure of the lower esophageal is more complete, and surgical field is clearer, and the dissociation is more convenient. Small incision-assisted Roux-en-Y reconstruction is often preferred. This procedure is highly safe, easy to perform, time-saving, and economically affordable. Therefore, it has become the most commonly used reconstruction method. However, this procedure also has some limitations: it is often limited by the patients’ body shape and the tumor condition. In patients with obesity, left hepatic hypertrophy, small costal angle, or high tumor location, the esophagus is expected to be divided at relatively high level. In such cases, the small incision-assisted reconstruction is often more difficult, and the incision often has to be extended to ensure the safety of the procedure. Therefore, in difficult cases, appropriately extending the small incision is particularly important to ensure the anastomosis safety. To avoid this limitation, in recent years we have adopted the completely laparoscopic oesophagus-jejunum anastomosis, which has shown better surgical field, simpler operation, and higher safety. It may the optimal digestive tract reconstruction method after laparoscopic total gastrectomy. The completely laparoscopic oesophagus-jejunum anastomosis can be performed using two different instruments: circular stapler and linear cutter & stapler.
The most challenging tasks during this procedure include the purse-string suture and the placement of an anvil. In previous practices, after the thorough dissociation of the esophagus, part of the esophageal wall shall be dissected; then, after the purse-string suture and the placement of an anvil are peformed under the laparoscope, divide the esophagus after tightening the purse-string. This approach is safer and more effective than the placement of an anvil after the complete transection of the esophagus and then the purse-string suture, thus avoiding the retraction of the esophageal stump. In recent years, we also apply the OrVil™ system (Covidien, USA) for anastomosis. Compared with other products, the OrVil™ system is easier to grasp and enables anastomosis at higher locations; also, it can achieve higher surgical margins (compared with the purse-string suture) and ensure the complete surgical margin, safe digestive tract reconstruction, and short surgical time. This product actually is a modified circular stapler. Compared with the conventional circular stapler, the OrVil™ system allows the placement of the anvil downwards via the esophagus. Some notable points include: (i) the introducer of the OrVil™ system must be thoroughly lubricated; (ii) the placement of the OrVil™ system via mouth should be performed by an anesthesiologist; it should be conducted under the direct vision of the laryngoscopy after the release of the safety airbag of the tracheal tube; (iii) avoid making too large hole at the esophageal stump; and (iv) the introducer should be gently pulled under the laparoscopy; excessively forceful pulling may cause the avulsion of the esophagus. However, the application of the OrVil™ system is limited by its high price. Thus, we have introduced a simple and safe “anti-puncturing” approach for oesophagus-jejunum anastomosis. This approach, initially reported by Omori et al., uses a #25 tubular stapler anvil and allows a 2-0 sewing needle with stitches to penetrate through the hole on its tip; the tail of the stitches is knotted to form a 2-cm woven braid. After the thorough dissociation of the stomach and esophagus, a small incision is made at the anterior wall of the esophagus, via which the device is delivered into the lower part of the esophagus, with its head facing the oral cavity. Then, the needle with stitches is sewed reversely at the anterior wall of the esophagus over the incision. The anvil is introduced and then tightened. The closure of the esophageal stump is completed using a linear stapler under the anvil. Thus, we use the stapler to replace the conventional purse-string suture and simplify the operational steps; thus, it can achieve higher cutting edge and lower surgical cost when compared with the OrVil™ system.
The completely laparoscopic esophagus-jejunum anastomosis using linear stapler was firstly proposed by Uyama et al. and then modified by Okabe et al. in 2009. Based on Kanaya’s delta anastomosis and Okabe’s FETE anastomosis, we performed a total of seven cases of completely laparoscopic esophagus-jejunum anastomosis from July 2013 to October 2013. The average operative time was (234±23) min, and the time consumed during the anastomosis was (34±7) min. There was no post-operative complication such as anastomotic fistula, anastomotic stricture, or abdominal infection, and the short-term follow-up outcomes were satisfactory. The completely laparoscopic anastomosis using linear stapler have some advantages: (i) it avoids the two difficult steps (purse-string suture and anvil placement) in the circular stapler-based procedure; (ii) it avoids the difficulty in placing the stapler into esophagus or jejunum with small diameters; (iii) the diameter of the anastomosis is not constrained by the esophagus diameter, which lowers the risk of anastomotic stricture after the surgery; and (iv) the whole anastomosis procedure is competed under the direct vision of laparoscope. However, such procedures also have some limitations: (i) when the anastomosis level is above the esophageal hiatus, the space inside the mediastinum is relatively narrow and often blocked by bilateral diaphragm angles, making the anastomosis under the laparoscopic monitoring particularly difficult; (ii) when the anastomosis level is relatively high, the closure of the common entry after the esophagus-jejunum anastomosis, whether by using a linear stapler or artificially, will be quite difficult; (iii) during the surgery, it needs 5-7 staplers, which is a little expensive. In our opinion, the completely laparoscopic esophagus-jejunum anastomosis is quite convenient and simple, with better anastomotic vision and larger anastomotic diameter; furthermore, it will not increase the anastomotic time. Therefore, it is a relatively safe, simple, and effective anastomotic method. In a recent report, Okabe et al. reported that they had performed completely laparoscopic esophagus-jejunum anastomosis using linear stapler in 104 patients, with a median follow-up of 29.6 months and an overall survival rate of 96.5%. Among these patients, the incidence of anastomotic leakage was 2.9%, which is similar to that of conventional open surgery. No anastomotic stricture was found. Obviously, the linear cutter & stapler has its unique advantages and can dramatically improve the patients’ quality of life.
Laparoscopic radical gastrectomy for gastric cancer requires the operator to have both the solid anatomic knowledge on gastric cancer and skillful laparoscopic operation capabilities. Any problem encountered during the surgery can be addressed using a progressive strategy. During the patient selection, a less experienced operator shall choose relatively younger and thinner patients with gastric cancers still in the early stages. It is believed that, along with the accumulated knowledge on gastric cancer and the improved skills in laparoscopic operations, the laparoscopic surgical treatment for gastric cancer will be further improved and promoted in China.
Acknowledgements
Disclosure: The author declares no conflict of interest.



