
Analysis of the factors influencing retrograde removal of double J ureteral stents using a simple snare technique in female patients
Introduction
The long-term patency of a double J ureteral stent is known to be limited due to calcium salt deposition or stent displacement/fracture thus requiring regular removal or replacement (1-3).
Although urologists traditionally remove and insert double J stents using a cystoscope (4), fluoroscopy-guided antegrade or retrograde removal and replacement of a double J stent has gradually been developed and is considered an effective alternative to cystoscopic procedures (5-11).
Four different technical modifications have been proposed to remove a double J stent, although there is no clear indication for each modification (12). The duration of the fluoroscopy procedure also varies widely in previous reports, from 1.0 to 67.6 minutes, which most likely reflects the status of the double J stent within the bladder (13).
Fluoroscopy-guided retrograde removal of a double J stent using a snare is most commonly used in female patients (12,13). However, there is limited published data analyzing factors such as the position of the double J stent, the number of curls in the double J stent end, the stent indwelling time, the presence or absence of obvious stent incrustation, and the ease of removal of a double J stent using a simple snare technique. Therefore, the purpose of this study is to identify the factors related to the effectiveness of retrograde removal of double J ureteral stents using a simple snare technique in female patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-21-1113).
Methods
Patient characteristics
The Ethics Committee of The Affiliated Cancer Hospital of Zhengzhou University approved this retrospective observational study and informed consent was waived. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki declaration (as revised in 2013). Of a total of 143 patients who underwent fluoroscopy-guided, retrograde double J stent removal and/or replacement from June 2012 to August 2017 and after excluding 15 male patients, 128 female patients were retrospectively analyzed. During the study period, all double J stent removal procedures were usually performed by interventional radiologists.
The inclusion criteria were: (I) female patients who underwent the placement of a double J stent for pelvic malignant ureteral obstruction without urinary bladder involvement; (II) a Karnofsky performance status ≥70; and (III) absence of bleeding disorders.
Analysis and definitions
The cause of the ureteral stricture, stent indwelling time, fluoroscopy time, position of the tip of the double J stent in the urinary bladder, number of curls in the tip of the double J stent in the bladder, obvious incrustation of the double J stent end, technical success rate of the stent removal, and procedure-related complications were evaluated.
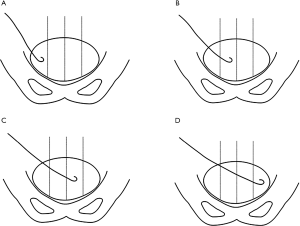
The position of the tip of the double J stent was classified as position type A, B, C, or D according to its location within the bladder (Figure 1). The bladder was equally divided into four quadrants. For types A to D, the tip of the double J stent was located in the ipsilateral lateral, ipsilateral medial, contralateral medial, and contralateral lateral quadrants of the urinary bladder, respectively.
Technical success was defined as the successful grasp of the tip of the double J stent within the urinary bladder and removal of the entire double J stent out of the urethral orifice. The fluoroscopy time was defined as the time required for the removal of one double J stent from the urethral orifice under fluoroscopy and measured from the hospital digital subtraction angiography image data and time information. The stent tip in the bladder had a tendency to curl to form one or more circles. If the stent tip formed one circle, the curl number was marked as one; if the stent tip formed two circles or more, the curl number was marked as two; if the curl of the stent tip was less than one circle, the curl number was marked as zero.
Complications were assessed through patient interviews and review of medical records during the follow-up of one month after the stent removal. Complications were classified as major or minor according to the guidelines of the Society of Interventional Radiology Standards of Practice Committee (14). Major complications were defined as complications requiring an unplanned increase in level of care or prolonged hospitalization, permanent adverse sequelae, or patient death. Minor complications were defined as complications requiring no nominal therapy, including overnight admission for observation only (14).
Double J stent removal procedures
The patients were placed in a supine position with the perineal area exposed and sterilized in the conventional manner. An injection of 5 mL of 2% lidocaine was administered through the urethral orifice in order to anesthetize the urethra and the bladder.
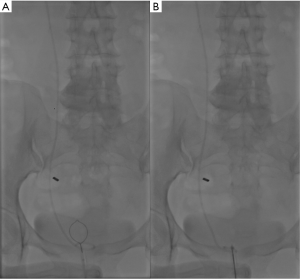
Interventional procedures were performed under fluoroscopic guidance using a digital subtraction angiography unit (FD20, Philips, Holland). The simple snare technique was utilized to remove the double J stent from the bladder. A 5F angiographic sheath (Radifocus, Terumo, Japan; length 10 cm) was inserted over a 0.035-inch guide wire (Radifocus, Terumo, Japan). The urinary bladder was distended with 3 mL of contrast medium (iopromide injection, Bayer Schering Pharmaceutical, Germany) diluted with 300 mL of normal saline. A snare system (JiYi-Snare; Shanghai, China; ring diameter of 2 cm) was inserted through the sheath after removing the guide wire (Figure 2A). The tip of the double J stent (Cook, Cook Corp., IL, USA; 6F/4.7F, 26 cm) was snared (Figure 2B) and the double J stent, snare system, and sheath were withdrawn together through the urethral orifice. Antibiotic prophylaxis was not performed prior to the double J stent removal.
If a double J stent was being replaced, a 0.035-inch guide wire was advanced through the indwelling double J stent, now located in the urethral orifice, into the renal pelvis. The double J stent was then removed, and a 5F vertebral catheter (Radifocus, Terumo, Japan) was advanced over the hydrophilic wire into the renal pelvis in order to opacify it. A stiff, 0.035-inch wire (Radifocus, Terumo, Japan) was then left in the renal pelvis, and a new double J stent (Cook, Cook Corp., IL, USA; 6F, 26 cm) was advanced into the renal pelvis. The pigtails of the new double J stent were deployed in the standard manner, and the indwelling wire was removed.
Statistical analysis
One-way analysis of variance was used to compare the fluoroscopy times according to the different position types, the different stent indwelling times, and the different curl numbers of the stent. The least significant difference test was used for subsequent comparisons of position type with fluoroscopy times.
The two-sample t test was used to compare the fluoroscopy times according to the presence or absence of obvious stent end incrustation. Furthermore, multiple stepwise linear regression was used to analyze the interaction of the significant factors with the fluoroscopy time. Two-sided tests were used, and P<0.05 was considered statistically significant. SPSS statistical software (SPSS version 17.0, SPSS, Chicago, IL, USA) was used for the data analysis.
Results
One hundred and twenty-eight patients were enrolled in this study (all females; average age: 50.48±10.57 years; age range: 24.0–75.0 years). Cervical cancer was the most common cause of ureteral stricture (n=80), followed by colorectal cancer (n=17), endometrial carcinoma (n=12), ovarian cancer (n=9), gastric cancer (n=4), ureteral cancer (n=3), pelvic sarcoma (n=2), and non-Hodgkin lymphoma (n=1).
A total of 312 procedures were performed during the study period, and a mean of 2.44 procedures were performed per patient. Fifty-three double J stents were removed, and 259 double J stents were replaced. The overall success rate of the procedures was 97.44% (304/312). Eight double J stent removal procedures failed, and all of these occurred in the position type D patients. These patients proceeded to have successful double J stent removal by cystoscopy.
Of the 304 successful double J stent removal procedures, the mean fluoroscopy time was 12.68±7.34 minutes (range, 1.00–50.00 minutes). The mean fluoroscopy times according to the different position types and the curl numbers of the stent tip in the bladder differed significantly (P=0.001 and P=0.003), whereas the mean fluoroscopy times according to different stent indwelling times or the presence or absence of obvious stent incrustation did not differ significantly (P=0.483 and P=0.607, one-way analysis of variance) (Table 1). Furthermore, multiple stepwise regression analysis demonstrated that the position type and the curl numbers of the double J stent were factors independently influenced the fluoroscopy time (respectively, P=0.001).
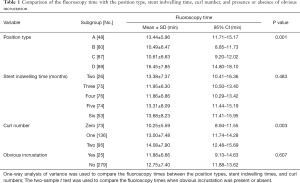
Full table
According to the p value of the least significant difference test, as illustrated in Table 2, the mean fluoroscopy times for types B and C were not statistically significant, but the mean fluoroscopy times for the other two position types differed significantly. Type D exhibited the longest fluoroscopy time followed by types B and C, and type A had the shortest fluoroscopy time.

Full table
According to the P value of the least significant difference test, as illustrated in Table 2, the mean fluoroscopy times for one curl and two curls were not statistically significant, although the mean fluoroscopy times for zero curl and one curl or zero curl and two curls differed significantly. The fluoroscopy time for zero curl was shorter compared with the fluoroscopy time for one curl or two curls, although the fluoroscopy time for one curl did not differ from the fluoroscopy time for two curls.
Although there were no major complications, such as bladder perforation or urinary tract infection, a minor post-procedure complication was pain in the urethral orifice or gross hematuria during the follow-up of one month after the stent removal. The incidence of pain in the urethral orifice was 5.1% (16/312), the incidence of gross hematuria was 3.2% (10/312), and the total complications rate was 8.3% (26/312). In all cases, both urethral orifice pain and gross hematuria were mild and resolved without medication within 24 hours.
Discussion
Since double J stent diameter is small and susceptible to encrustation, sludge and external compression, stent obstruction is not uncommon during follow-up. Therefore, careful clinical observation of urinary obstruction symptoms such as decreased urine out or flank pain is required, and if abnormalities are suspected, imaging studies such as ultrasound or CT are also required. Nevertheless, if a double J stent malfunction occurs, it needs to be removed.
It is important to grasp the tip of the ureteral double J stent with a snare within the bladder when retrograde double J stent removal/replacement is performed under fluoroscopic guidance. We found that the position type and number of curls in the double J stent in the bladder in female patients can help an operator to recognize the ease of grasping the tip of the double J stent with a snare.
According to our experience in this study, the possible factors influencing the fluoroscopy time included the number of curls in the tip of the stent in the bladder, the stent indwelling time, or the incrustation on the stent. All of these factors, together with the position type, were analyzed by one-way analysis of variance and further multiple regression analysis, and our results demonstrated that the position type and the curl numbers were factors independently influenced the fluoroscopy time.
According to statistical analysis, the stent indwelling time and obvious stent incrustation had no significant influence on the fluoroscopy time. A long stent placement duration might cause stent incrustation and possibly block the stent, which could cause difficulty exchanging the double J stent. However, we found that the incrustation on the stent surface did not influence snaring the stent which is the most important step for stent removal. Therefore, the stent indwelling time and stent incrustation were not factors affecting the ease of retrograde removal of double J stents using a simple snare technique.
According to statistical analysis, the number of curls at the tip of the stent had a significant influence on the fluoroscopy time. If the tip of the stent in the bladder formed a circle, the tip of the stent was within the center of the circle, and it was, therefore, difficult for the snare ring to grasp the stent end. If the tip of the stent formed less than a circle, it was easier for the ring to grasp the stent end. Therefore, the number of curls in the tip of the stent in the bladder was an influencing factor regarding the ease of the double J stent removal from the bladder.
According to our clinical experience and statistical analysis, the position of the tip of the stent in the bladder had a significant influence on the fluoroscopy time. It was easiest to grasp the tip of the stent in position type A compared with the other position types; position types B and C were easier than position type D, which was the most difficult and had the greatest possibility of removal failure.
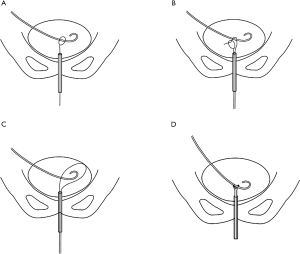
Four different techniques have been reported as useful in fluoroscopy-guided, retrograde removal of double J stents in female patients, i.e., the simple snare technique discussed in this study, the modified snare technique, the guide-wire lasso technique, and the forceps grasping technique (Figure 3) (12). Knowing the factors that influence effective retrograde double J stent removal in the bladder will assist an operator in choosing the most suitable method of stent removal.
In this study, the simple snare technique was deemed safe as there were no major complications and a low incidence of minor complications. There were some instances of transient hematuria which resolved spontaneously. Urinary tract infection after the procedure was reported in other studies, it was controlled by intravenous antibiotic treatment (10,12). No severe complications occurred, such as bladder perforation or massive hemorrhage from the bladder.
The current study has several limitations. First, the retrospective nature of the study may have limited the detection of more subtle complications. Second, we reported the experience of only one institution without considering the heterogeneity across practices. Third, small sample size may have limited the power of the study to detect small differences between the position types of the tip of the double J stent. Prospective randomized studies are expected to be needed in the future. Fourth, male patients were excluded due to the small sample size, but their different anatomy compared with females may have increased the fluoroscopy time.
In conclusion, the position type and the curl numbers of the tip of the double J ureteral stent in the bladder have a significant influence on the ease of retrograde removal of double J stents using a simple snare technique in female patients.
Acknowledgments
Funding: This study was supported by Natural Science Foundation of Henan Province (Grant No. 202300410463).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-21-1113
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-21-1113
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-21-1113). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The research protocol was approved by the institutional ethics committee of the Affiliated Cancer Hospital of Zhengzhou University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki declaration (as revised in 2013). Written informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sakamoto H, Matsuda A, Kanno T, et al. Retrospective analysis of the long-term indwelling ureteral stent. Hinyokika Kiyo 2012;58:269-72. [PubMed]
- Venkatesan N, Shroff S, Jeyachandran K, et al. Effect of uropathogens on in vitro encrustation of polyurethane double J ureteral stents. Urol Res 2011;39:29-37. [Crossref] [PubMed]
- Turgut B, Bayraktar AM, Bakdık S, et al. Placement of double-J stent in patients with malignant ureteral obstruction: antegrade or retrograde approach? Clin Radiol 2019;74:976.e11-7. [Crossref] [PubMed]
- Karthikeyan VS, Keshavamurthy R, Mallya A, et al. Efficacy of preprocedural diclofenac in men undergoing double J stent removal under local anesthesia: A double-blind, randomized control trial. Indian J Urol 2017;33:53-7. [PubMed]
- Uthappa MC, Cowan NC. Retrograde or antegrade double-pigtail stent placement for malignant ureteric obstruction? Clin Radiol 2005;60:608-12. [Crossref] [PubMed]
- Grasso RF, Faiella E, Cazzato RL, et al. Retrograde fluoroscopy-guided trans-urethral exchange of ureteral stents: Comparison of direct grasping vs. modified snare. Indian J Radiol Imaging 2013;23:347-50. [Crossref] [PubMed]
- Ozkan O, Akinci D, Bozlar U, et al. Retrograde ureteral stent exchange under fluoroscopic guidance. Diagn Interv Radiol 2009;15:51-6. [PubMed]
- Shin JH, Yoon HK, Ko GY, et al. Percutaneous antegrade removal of double J ureteral stents via a 9-F nephrostomy route. J Vasc Interv Radiol 2007;18:1156-61. [Crossref] [PubMed]
- Yedlicka JW Jr, Aizpuru R, Hunter DW, et al. Retrograde replacement of internal double-J ureteral stents. AJR Am J Roentgenol 1991;156:1007-9. [Crossref] [PubMed]
- Carrafiello G, Laganà D, Mangini M, et al. Fluoroscopically guided retrograde replacement of ureteral stents. Radiol Med 2007;112:821-5. [Crossref] [PubMed]
- de Baere T, Denys A, Pappas P, et al. Ureteral stents: exchange under fluoroscopic control as an effective alternative to cystoscopy. Radiology 1994;190:887-9. [Crossref] [PubMed]
- Park SW, Cha IH, Hong SJ, et al. Fluoroscopy-guided transurethral removal and exchange of ureteral stents in female patients: technical notes. J Vasc Interv Radiol 2007;18:251-6. [Crossref] [PubMed]
- McCarthy E, Kavanagh J, McKernan S, et al. Fluoroscopically guided transurethral removal and/or replacement of ureteric stents in women. Acta Radiol 2015;56:635-40. [Crossref] [PubMed]
- Angle JF, Siddiqi NH, Wallace MJ, et al. Quality improvement guidelines for percutaneous transcatheter embolization: Society of Interventional Radiology Standards of Practice Committee. J Vasc Interv Radiol 2010;21:1479-86. [Crossref] [PubMed]


