
Outcomes of arthroscopic bone graft transplantation for Hepple stage V osteochondral lesions of the talus
Introduction
Osteochondral lesions of the talus (OLT) are a commonly seen injury, which can occur in up to 50% of acute ankle sprains and fractures (1,2). Based on MRI imaging findings, OLT can be classified into 5 stages, in which stage V represents OLT with subchondral cyst formation. It has been reported that stage V lesions are consistent with the severest symptoms, which pose the greatest treatment challenge and the have the worst prognosis (3).
Many surgical methods have been reported to treat stage V OLT, including arthroscopic microfracture surgery, chondrocyte transplantation, and bone or osteochondral transplantation techniques (autograft or allograft) (4,5). Surgeons widely favor arthroscopic microfracture surgery because of its advantages of minimal invasiveness and quick recovery. Nevertheless, it presents a specific problem because drilling or debridement alone cannot reestablish the structure of bony defects and subchondral support (6). For OLT patients with a large subchondral cyst, researchers have recommended the use of autologous/allogeneic osteochondral or autologous chondrocyte transplantation as the initial procedures since these patients do not do well with conventional marrow stimulation techniques (7). As many studies have reported good results using these methods previously, osteochondral autograft or allograft transplantation may be a reasonable choice for these patients (8-10). However, the need for osteotomy or open surgery, donor site complications, and secondary operations are still problems. Therefore, a more minimally invasive and effective method needs to be developed to reduce surgical trauma while ensuring surgical efficacy when treating stage V OLT.
This study aimed to retrospectively evaluate the postoperative clinical scores and imaging results of a novel method with arthroscopic calcaneus bone graft transplantation for patients with Hepple stage V OLT. This study hypothesized that this method could achieve satisfying clinical and radiographic results for these patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-21-2006).
Methods
Patients
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Huashan Hospital. Individual consent for this retrospective analysis was waived. All patients involved in the follow-up study were diagnosed with Hepple stage V OLT based on clinical manifestations and MRI results. All patients accepted conservative treatment for at least 6 months and still had persistent pain. Patients with a history of affected side ankle joint surgery, ankle fracture, degenerative joint disease, inflammatory joint disease, or joint infection were excluded.
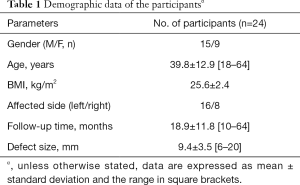
From June 2014 to December 2018, a total of 28 patients underwent arthroscopic bone graft transplantation surgery. During the follow-up period, 4 patients were lost to follow-up. Finally, 24 patients were included in this study. The demographic data of the participants are presented in Table 1.
Full table
Surgical technique
After general or spinal anesthesia, the patient was placed in a supine position, with the knees bent and put on a unique triangular pillow. A tourniquet was tied at the upper thigh.
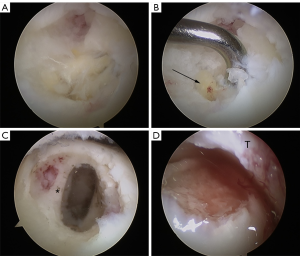
The conventional anteromedial and anterolateral approaches were made, and the ankle joint was thoroughly detected. All the combined lesions, including synovitis, osteophytes, loose bodies, and ligament injury, were treated. The osteochondral lesion was confirmed, and the injured cartilage was removed (7,11). Then, the bone cysts were scraped with a curette and shaver until the healthy bone bed was exposed. The size of the lesion was measured with a probe. Then, a 1.5 cm transverse incision was made at 2.5 cm below the lateral malleolus. A calcaneal bone pillar with an 8 mm diameter was taken out using the osteochondral autograft transfer system (OATS; Arthrex, Naples, FL, USA), and an absorbable gelatin sponge (Ethicon) was placed into the donor site to promote hemostasis. Afterward, the autologous calcaneous cancellous bone was implanted into the location of OLT arthroscopically, and fixed with fibrin glue (Figure 1).
Patients were encouraged to start the rehabilitation exercises the day after the operation. Patients could walk with partial weight-bearing at 4 weeks after the surgery and with full weight-bearing at 8 weeks after the surgery.
Clinical and MRI evaluation
Four clinical scores, including the American Orthopedic Foot and Ankle Society (AOFAS) score, the Karlsson Ankle Function Score (KAFS), the Tegner score, and the visual analogue scale (VAS), were used for clinical evaluation (12-15). A total of 14 patients completed the MRI examination, 2 experienced musculoskeletal radiologists evaluated the MRI data, and the average Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) 2.0 score was obtained according to the 7 variables proposed by Schreiner et al. (16).
Statistical analysis
The data were examined by GraphPad Prism statistical software (version 7.00, GraphPad Software Inc.). All data are expressed as mean ± standard deviation. The paired t-test was then used to compare the clinical scores before and after the operation. A P value of less than 0.05 was considered statistically significant.
Results
A total of 24 patients met the inclusion criteria and were included in this study. There were 15 male patients and 9 female patients with a mean age of 39.8 (range, 18–64) years (Table 1). The mean postoperative follow-up time was 18.9 (range, 10–64) months. All 24 patients with clinical scores were followed up at this time, of which 14 patients accepted MRI examinations at follow-up. Among the 24 patients, 18 patients had isolated OLT, while the other 6 patients had concomitant lateral ankle ligament injury and underwent ligament repair or reconstruction. There were no intraoperative and postoperative complications during the entire study.
Clinical outcome
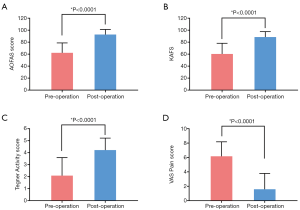
As shown in Figure 2, a significant increase was noted in AOFAS score (P<0.0001), KAFS (P<0.0001), Tegner activity score (P<0.0001), and the VAS pain score (P<0.0001) (preoperatively: 62.2, 60.4, 2.1, and 6.2, respectively; postoperatively: 92.8, 88.5, 4.2, and 1.6, respectively).
MRI evaluation
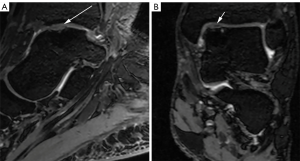
A total of 14 patients underwent MRI examinations postoperatively, with an average follow-up time of 20.1±14.1 months. The average MOCART score of postoperative MRI was 68±14.8 (Figure 3).
Discussion
The most important finding of the present study is that arthroscopic calcaneus bone graft transplantation could obtain satisfying clinical and radiologic outcomes for patients with Hepple stage V OLT.
For the management of OLT, many factors need to be considered when choosing the surgical method, including age, defect size, cyst formation, and cyst size, which all play a crucial role in predicting prognosis (5,17). Although several surgical methods for OLT patients have been described, the best treatment for patients with Hepple stage V OLT has not been established. Normally, bone marrow stimulation techniques under arthroscopy, including microfracture and drilling, are commonly used treatments for small to medium symptomatic OLT (18,19). Nevertheless, drilling or debridement alone cannot restore the structure of bone defects and subchondral supports, presenting a particular problem. As patients with OLT with subchondral cysts greater than 6 mm in depth do not do well with conventional marrow stimulation techniques, autologous/allogeneic osteochondral or autologous chondrocyte transplantation is recommended (7,20). Although osteochondral autograft or allograft transplantation may be a reasonable option for Hepple stage V OLT (21), it still has problems such as undesirable donor site morbidity, which was reported in 16.9% of cases in the knee-to-ankle procedure (22), malunion, or non-union. Therefore, the objective of this study was to retrospectively evaluate the postoperative clinical scores and MRI findings of a novel method with calcaneus bone graft transplantation for patients with Hepple stage V OLT under arthroscopy.
In the present study, patients with Hepple stage V OLT had good clinical results postoperatively in terms of AOFAS score, KAFS, Tegner activity score, and VAS pain socre. Previously, Zhu et al. (23) reviewed 13 patients who had autologous osteochondral transplantation (AOT) combined with cancellous allograft to manage large cystic OLT, and found that 100% obtained good to excellent clinical results at a mean follow-up of 25.4 months. Another study by Sawa et al. (24) demonstrated that using autologous bone graft to treat OLT with large subchondral cysts improved the AOFAS score from 65.7 preoperatively to 92 postoperatively. However, in these studies, surgeons obtained grafts from other parts of the patient and performed osteotomy or open surgery on patients to better expose the surgical field, which leads to donor site morbidity, additional damage to the normal tibia, and the need for a second operation to remove the screws used for fixation. It has been reported that malleolus osteotomy may lead to malunion or non-union (25) and avoiding osteotomy would eliminate the risk of altering joint congruity and non-union or malunion of the osteotomy site (26). Furthermore, a systematic review by Shimozono et al. showed that the common complications of AOT for OLT are the morbidity of the donor site as well as nerve damage, symptomatic hardware, anterior ankle impingement, and non-union of the graft or osteotomy site (27). In comparison, the surgery in this study was a fully arthroscopic operation, which avoids the disadvantages of open surgery or osteotomy while obtaining similar clinical outcomes as other treatments. Furthermore, it is much more economical than osteochondral transplantation and provides a feasible approach for treating patients with Hepple stage V OLT.
Currently, if bone grafting is used alone to treat OLT, fibrocartilage tissue may form at the lesion site instead of hyaline tissue, so researchers have considered using a scaffold overlying the bone graft to restore osteochondral integrity (28). Many scaffolds have been reported, including periosteum (29), collagen powder (30), type I collagen membrane (31), type I/III collagen membrane (32), collagen gel (33), and fibrin gel (34), among others. Previously, Sadlik et al. (35) reported that good results were obtained after a modified “sandwich” technique combining autologous bone chips, fibrin glue, and collagen matrix for large osteochondral lesions of the talar dome. We only used fibrin glue to fix the injury site after implantation. However, our results show that this fixation method can also obtain satisfactory clinical results, which may be due to the excellent blood oozing condition that provides abundant bone marrow stem cells. This procedure provides us with a cost-saving, effective, minimally invasive method. In future studies, we will consider combining other scaffold materials to explore their clinical application value based on this study. Nonetheless, the highlight of this study is that implantation and fixation of the graft were completed under arthroscopy, which can overcome the drawbacks of osteotomy or open surgery in other research (35,36).
Moreover, it has been reported that the results of studies on AOT for the treatment of large OLT showed that the MOCART score at 12 months after surgery was 68.3±22.4 (21). Sadlik et al. (35) investigated 10 large OLT patients with a modified “sandwich” technique combining autologous bone chips, bone marrow mesenchymal stem cells, and fibrin glue, and found that the average MOCART score was 69.5±16.7 at a mean follow-up of 46.4 months. In this study, with arthroscopic bone transplantation and fixation with fibrin glue, our MRI-based MOCART score of the lesion site was 68±14.8 points. This phenomenon indicates that, in the short-term MRI follow-up, the quality and state of the repair tissue at 18.9 months after bone transplantation is similar to that of the repair tissue at 12 months after AOT or 46.6 months after a modified “sandwich” technique. It was demonstrated that it takes longer for OLT patients after treatment with bone chip and fibrin glue to achieve similar MOCART scores of AOT. However, patients’ postoperative clinical outcomes in this study were significantly improved compared with those before surgery. Therefore, a longer MRI follow-up is needed to determine the radiological changes in patients after surgery.
There were several limitations to this study. Firstly, this study was a retrospective case series, and there was a lack of a control group in the experimental design. Secondly, the follow-up time in this study varied considerably, which might have introduced confounding bias to the results. For future research, to better verify the efficacy of arthroscopic calcaneal cancellous bone treatment in this patient population, research with a high level of evidence needs to be performed to determine a robust conclusion.
Conclusions
Arthroscopic calcaneal cancellous bone graft is an effective treatment for patients with Hepple stage V type OLT and can obtain satisfying clinical and radiological results at short-term follow-up.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-21-2006
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-21-2006
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-21-2006). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Huashan Hospital. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Santrock RD, Buchanan MM, Lee TH, et al. Osteochondral lesions of the talus. Foot Ankle Clin 2003;8:73-90. viii. [Crossref] [PubMed]
- Saxena A, Eakin C. Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med 2007;35:1680-7. [Crossref] [PubMed]
- Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int 1999;20:789-93. [Crossref] [PubMed]
- Aurich M, Albrecht D, Angele P, et al. Treatment of osteochondral lesions in the ankle: a guideline from the Group "Clinical Tissue Regeneration" of the German Society of Orthopaedics and Traumatology (DGOU). Z Orthop Unfall 2017;155:92-9. [PubMed]
- Gu W, Li T, Shi Z, et al. Management of Hepple Stage V Osteochondral Lesion of the Talus with a Platelet-Rich Plasma Scaffold. Biomed Res Int 2017;2017:6525373 [Crossref] [PubMed]
- Kolker D, Murray M, Wilson M. Osteochondral defects of the talus treated with autologous bone grafting. J Bone Joint Surg Br 2004;86:521-6. [Crossref] [PubMed]
- Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med 2008;36:1750-62. [Crossref] [PubMed]
- Ahmad J, Jones K. Comparison of osteochondral autografts and allografts for treatment of recurrent or large talar osteochondral lesions. Foot Ankle Int 2016;37:40-50. [Crossref] [PubMed]
- Hurley ET, Murawski CD, Paul J, et al. Osteochondral Autograft: Proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int 2018;39:28S-34S. [Crossref] [PubMed]
- Smyth NA, Murawski CD, Adams SB Jr, et al. Osteochondral Allograft: Proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int 2018;39:35S-40S. Erratum in: Foot Ankle Int 2021;42:248. [Crossref] [PubMed]
- Li H, Hua Y, Li H, et al. Treatment of talus osteochondral defects in chronic lateral unstable ankles: small-sized lateral chondral lesions had good clinical outcomes. Knee Surg Sports Traumatol Arthrosc 2018;26:2116-22. [Crossref] [PubMed]
- Cline ME, Herman J, Shaw ER, et al. Standardization of the visual analogue scale. Nurs Res 1992;41:378-80. [Crossref] [PubMed]
- Karlsson J, Peterson L. Evaluation of ankle joint function: the use of a scoring scale. The Foot 1991;1:15-9. [Crossref]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Crossref] [PubMed]
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985;43-9. [Crossref] [PubMed]
- Schreiner MM, Raudner M, Marlovits S, et al. The MOCART (Magnetic Resonance Observation of Cartilage Repair Tissue) 2.0 Knee Score and Atlas. Cartilage 2019; Epub ahead of print. [Crossref] [PubMed]
- Zengerink M, Struijs PA, Tol JL, et al. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc 2010;18:238-46. [Crossref] [PubMed]
- Becher C, Malahias MA, Ali MM, et al. Arthroscopic microfracture vs. arthroscopic autologous matrix-induced chondrogenesis for the treatment of articular cartilage defects of the talus. Knee Surg Sports Traumatol Arthrosc 2019;27:2731-6. [Crossref] [PubMed]
- Dahmen J, Lambers KTA, Reilingh ML, et al. No superior treatment for primary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc 2018;26:2142-57. [Crossref] [PubMed]
- Scranton PE Jr, Frey CC, Feder KS. Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br 2006;88:614-9. [Crossref] [PubMed]
- Nguyen A, Ramasamy A, Walsh M, et al. Autologous osteochondral transplantation for large osteochondral lesions of the talus is a viable option in an athletic population. Am J Sports Med 2019;47:3429-35. [Crossref] [PubMed]
- Andrade R, Vasta S, Pereira R, et al. Knee donor-site morbidity after mosaicplasty - a systematic review. J Exp Orthop 2016;3:31. [Crossref] [PubMed]
- Zhu Y, Xu X. Osteochondral autograft transfer combined with cancellous allografts for large cystic osteochondral defect of the talus. Foot Ankle Int 2016;37:1113-8. [Crossref] [PubMed]
- Sawa M, Nakasa T, Ikuta Y, et al. Outcome of autologous bone grafting with preservation of articular cartilage to treat osteochondral lesions of the talus with large associated subchondral cysts. Bone Joint J 2018;100-B:590-5. [Crossref] [PubMed]
- Kreuz PC, Steinwachs M, Edlich M, et al. The anterior approach for the treatment of posterior osteochondral lesions of the talus: comparison of different surgical techniques. Arch Orthop Trauma Surg 2006;126:241-6. Erratum in: Arch Orthop Trauma Surg 2007;127:311. [Crossref] [PubMed]
- Orr JD, Dutton JH, Nelson JR, et al. Indications for and early complications associated with use of temporary invasive distraction for osteochondral graft transfer procedures for treatment of lateral osteochondral lesions of the talus. Foot Ankle Int 2014;35:50-5. [Crossref] [PubMed]
- Shimozono Y, Hurley ET, Myerson CL, et al. Good clinical and functional outcomes at mid-term following autologous osteochondral transplantation for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 2018;26:3055-62. [Crossref] [PubMed]
- Rothrauff BB, Murawski CD, Angthong C, et al. Scaffold-Based Therapies: Proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int 2018;39:41S-7S. Erratum in: Foot Ankle Int 2021;42:248. [Crossref] [PubMed]
- Desando G, Bartolotti I, Vannini F, et al. Repair potential of matrix-induced bone marrow aspirate concentrate and matrix-induced autologous chondrocyte implantation for talar osteochondral repair: patterns of some catabolic, inflammatory, and pain mediators. Cartilage 2017;8:50-60. [Crossref] [PubMed]
- Buda R, Vannini F, Cavallo M, et al. One-step bone marrow-derived cell transplantation in talarosteochondral lesions: mid-term results. Joints 2014;1:102-7. [PubMed]
- Aurich M, Bedi HS, Smith PJ, et al. Arthroscopic treatment of osteochondral lesions of the ankle with matrix-associated chondrocyte implantation: early clinical and magnetic resonance imaging results. Am J Sports Med 2011;39:311-9. [Crossref] [PubMed]
- Kubosch EJ, Erdle B, Izadpanah K, et al. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop 2016;40:65-71. [Crossref] [PubMed]
- Volpi P, Bait C, Quaglia A, et al. Autologous collagen-induced chondrogenesis technique (ACIC) for the treatment of chondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 2014;22:1320-6. [Crossref] [PubMed]
- Lee KT, Kim JS, Young KW, et al. The use of fibrin matrix-mixed gel-type autologous chondrocyte implantation in the treatment for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 2013;21:1251-60. [Crossref] [PubMed]
- Sadlik B, Kolodziej L, Blasiak A, et al. Biological reconstruction of large osteochondral lesions of the talar dome with a modified "sandwich" technique-Midterm results. Foot Ankle Surg 2017;23:290-5. [Crossref] [PubMed]
- Valderrabano V, Miska M, Leumann A, et al. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am J Sports Med 2013;41:519-27. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)


