Pulmonary lobectomies for patients with cognitive impairment: the importance of postoperative respiratory care
Introduction
Cognitive function is defined as the ability to learn new knowledge or recall prior acquired information, to recognize and use familiar objects, to plan or organize normal daily activities, to perform complex tasks, and to comprehend words (1). Anyone who is cognitively impaired may lack, to a greater or lesser degree, “normal” thinking facilities such as the ability to remember, learn at a normal pace, adapt behaviors to social settings, and process or understand information. People with cognitive impairment (CI) may perceive that others talk too quickly for them to understand, and may find it challenging to keep up with conversations (2).
Similarly, patients with CI undergoing thoracic surgery may face similar cognitive obstacles and may be at increased risk for postoperative complications. Several studies demonstrated impaired cognitive conditions are important predictors of postoperative complications; patients with CI are at increased risk of postoperative outcomes compared with the general hospital population (3,4). However, little is known about the impact of CI on thoracic surgery postoperative respiratory complications, as well as its corresponding treatment.
Herein, we evaluated our experience with the management of postoperative respiratory complications in patients with CI undergoing open thoracotomy.
Methods
Approval for the study was obtained from the Ethics Committee of the participated hospital. All researchers were fully complied with the following ethical standards.
Informed consent: patients or significant others signed informed consent statements for data collection and follow-up telephone contact or other interview. If eligible patients were unable to provide consent, relatives or legal representatives were asked to consent. Written informed consent was obtained from all study participants.
Confidentiality: all participants have the right for their participation to remain confidential in that only the researcher will be aware who has participated. Generally all data will also be anonymous in the final report so that nothing can be attributed back to an individual participant.
Types of cognitive impairment (CI)
CI may originate from certain types of brain disorders such as acquired brain injury, autism spectrum disorder, intellectual disability [mental retardation (MR)], organic dementia, and other neurological or psychiatric conditions.
Dementia of the Alzheimer’s type (DAT) is defined as clinical evidence of memory loss and impairment of at least one other cognitive domain, with evidence of disturbance in social or occupational function (1). MR is a disability characterized by significant limitations in both intellectual functioning and adaptive behaviors as expressed in conceptual, social, and practical adaptive skills; this disability originates before age 18 (5,6). The intellectual disability meta-syndrome (syndrome grouping) is characterized by a deficit in cognitive functioning prior to the acquisition of skills through learning (7). For the purposes of this study, diagnostic criteria for DAT and MR were based on The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) (8).
Patients
We retrospectively analyzed 1,325 patients who underwent pulmonary lobectomy via open thoracotomy for the treatment of lung cancer between January 2006 and December 2008 at Shanghai Pulmonary Hospital. Five patients in this cohort were diagnosed with CI: two patients had DAT and three patients had MR. All five patients were diagnosed by psychiatrist, the cognitive status was assessed using the Folstein mini-mental state examination (MMSE) (9). Additionally, postoperative data of 1,320 patients with normal cognition who underwent lobectomy via open thoracotomy was obtained from Shanghai Pulmonary Hospital between January 2006 and December 2008. Age, blood loss, operative times, duration of chest tube drainage, length of hospital stay, and morbidity rates were compared between the two groups. Operative time was determined as the time from beginning skin incision to closing skin incision. Length of hospital stay was defined as the date from being hospitalized to the date out of the hospital. Re-intubation time was determined as the date from operation being completed to re-intubation; tracheotomy time was determined as the date from operation being completed to tracheotomy. The post-operative complications were defined and showed in Table 1.

Full table
Preoperative assessment
Preoperative bronchoscopies were performed routinely in the five patients with CI. Adenocarcinoma was diagnosed via transbronchial biopsy in three patients. Preoperative computed tomography (CT) scan, whole body bone scan, and abdominal ultrasound were performed to exclude remote metastasis in these patients. Transbronchial biopsy and percutaneous needle lung biopsy were performed in the other two patients. In patients whose biopsies were negative, anti-inflammatory therapy was administered for 2 weeks; if there was no change in tumor size or symptoms, surgery was performed. Preoperative risk stratification was performed in all patients.
Operative approach
All five patients underwent posterolateral thoracotomy under general anesthesia. Epidural catheters were placed preoperatively. Systematic mediastinal lymph node dissection was performed if frozen sections of tumor demonstrated malignancy. Two chest tubes (32 and 24 Fr) and a small pleural catheter (6 Fr) were routinely inserted into the pleural space for postoperative lung expansion and drainage.
Postoperative management
All patients were extubated in the recovery room postoperatively. Continuous epidural analgesia was administered postoperatively for 2 days. Inferior chest tubes were removed 1 to 2 days postoperatively; superior chest tubes were removed after it was ensured that there was no residual air leak and that the lung had adequately re-expanded with chest radiograph. The small pleural catheter was removed when the drainage amount reached less than 50 mL/day.
Statistical analysis
Numerical data were expressed as the median [interquartile range (IQR)]. Statistical differences between the two groups were calculated using the nonparametric Wilcoxon Mann-Whitney test; categorical variables were compared using Fisher’s exact test. A P value <0.05 was considered to be statistically significant.
Results
Degree of impairment
The MMSE scores of five CI patients were 20, 19, 22, 18, 17, respectively; two patients were mild impairment (Scores 20-25), while three patients were moderate impairment (Scores 10-20).
Demographic data
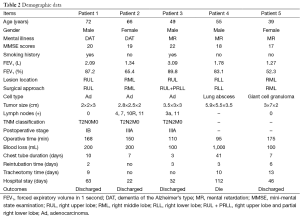
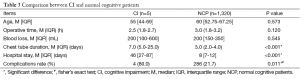
Five patients with CI (three male, two female; median ages 55; range, 39-72 years) were hospitalized due to suspected lung cancers on radiographs. Symptoms at presentation included a persistent dry cough (patients 1,5), hemoptysis (patients 2,3), and refractory fever (38 °C) (patient 4). On final pathology, adenocarcinomas were present in three patients while lung abscess and giant cell granuloma were confirmed in the other two. Patient demographic data is summarized in Table 2. When comparing the CI and normal cognitive function groups, chest tube duration, hospital stay, and complication rate were significantly different between two groups. In CI patients, chest tube duration and hospital stay were much longer compared with patients with normal cognitive function, while complication rate and hospital cost were much higher (see Table 3).
Full table
Full table
Complications and outcomes
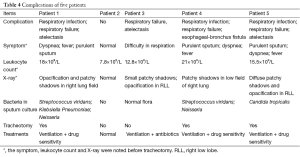
All five patients experienced dyspnea and sputum retention due to ineffective cough; bronchoscopic suctioning was required on the second postoperative day. Four patients had persistent pulmonary atelectasis after two or three bronchoscopic suctioning attempts, with significant hypoxia (PaO2 <60 mmHg) and hypercapnia (PaCO2 >50 mmHg). These four patients (80%) were re-intubated and required mechanical ventilations between postoperative days 2 through 6 (mean, 3.2 days) (Table 2). The remaining patient who did not require intubation had adequate expectoration, but only after two bronchoscopic suctioning attempts.
Of the four patients who were re-intubated, one was extubated seven days later when blood gas analysis was satisfactory (SpO2 >95%; PaO2 >80 mmHg; PaCO2 <45 mmHg). The remaining three patients continued to have high fevers and ropy sputum with unstable pulmonary function. Sputum cultures revealed opportunistic bacteria, three patients were cured with sensitive intravenous antibiotics according to antimicrobial susceptibility testing and one patient was cured with empirical intravenous antibiotics (the complications and therapy of 5 patients were revealed in Table 4); tracheotomy was required after 7 days for secondary respiratory infection. Of the three patients who required tracheotomy, two recovered from respiratory infection after antibiotic management. One patient was further development to bronchial-esophageal fistula, and died on postoperative day 112. The remaining four patients were discharged with a median hospital stay of 46 (IQR: 27-87) days.
Full table
Follow up
All patients underwent postoperative follow up every 3 months for the first 2 years after surgery, and every 6 months thereafter. The median follow-up period was 56 (range, 36-84) months and the end follow-up point was December 2011. Complete follow-up data was obtained in 4/5 cases. One patient (patient 3) died of cancer recurrence 47 months postoperatively; one patient (patient 2) died 65 months postoperatively due to respiratory infection. Two patients (patients 1,5) remained alive at the final follow-up date.
Discussion
This study shows that patients with CI had high postoperative complication rates, length of hospital stay, and hospital cost compared with patients of normal cognitive function. In our CI patient cohort, complications included respiratory failure and respiratory infection due to sputum accumulation. Postoperative retention of airway secretions is an important risk factor for atelectasis and pulmonary infection (14,16), also seen in our group. Patients with CI may also have barriers to understanding, for example, instructions to actively cough. This may result in increased retention of secretions and subsequent complications. This is especially detrimental in patients who have just undergone thoracotomy, due to the underlying pulmonary compromise from sudden loss of lung volume.
Prompt and effective sputum clearance is critical in these patients. Although bronchoscopy is commonly performed in the setting of sputum retention and atelectasis in the ICU, its role in treating atelectasis secondary to excess airway secretions or decreased cough efficiency is controversial (17). According to a review performed by Kreider et al., bronchoscopy has been shown to be moderately effective in removing retained secretions and improving atelectasis (18). Four CI patients in our study cohort required bronchoscopic suction up to three times and ultimately required re-intubation due to respiratory failure.
Mini-tracheostomy (MT) utilizes a thin un-cuffed tracheal tube (4.5 mm internal diameter), inserted through the cricothyroid membrane under local anesthesia (19). It is reported that Cricothyroid MT usually does not alter the ability to speak or swallow and thus does not compromise quality of life; MT facilitates early and regular suctioning of the tracheobronchial tree during the critical postoperative period, and is well-tolerated without significant side effects (20). Learning from peer experience, MT may be a suitable method for preventing retention of secretions and subsequent complications for patients with CI.
Postoperative pain may also result in impaired sputum clearance and reduced ventilator capacity (21). Thoracotomy can be associated with severe postoperative pain (22). Chest tubes and pleural drains represent an additional activator of pain-sensing fibers and directly influence maximum pain scores (23,24); removal reduces pain and improves ventilatory function (25). We typically position a small tube in the posterior plural cavity, in addition to apical and basal drainage. The basal drainage tube is generally removed 1 to 2 days postoperatively to reduce pain; the smaller tubes are maintained for blood and fluid drainage.
Conclusions
Patients with CI after thoracic surgery were strongly associated post-operative respiratory complications due to ineffective expectoration, sputum clearance are important for these patients. Pain-control managements or prophylactic MT may be a good option to relieve secretion retention.
Our study was a retrospective study and only five cases with CI were included; therefore, the small population may potentially influence the results. A larger number of cases are required to determine the optimal pre- and post-operative management of CI patients undergoing pulmonary lobectomy via thoracotomy.
Acknowledgements
The authors thank Mr. Bo Su (Central Laboratory, Shanghai Pulmonary Hospital, Tongji University School of Medicine) for his assistance in statistical analysis.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Castellani RJ, Rolston RK, Smith MA. Alzheimer disease. Dis Mon 2010;56:484-546. [PubMed]
- Christensen TE, what-is-cognitive-impairment, wise GEEK, Conjecture Corporation, 2003-2013. Available online: http://www.wisegeek.com/what-is-cognitive-impairment.htm
- Fukuse T, Satoda N, Hijiya K, et al. Importance of a comprehensive geriatric assessment in prediction of complications following thoracic surgery in elderly patients. Chest 2005;127:886-91. [PubMed]
- Partridge JS, Dhesi JK, Cross JD, et al. The prevalence and impact of undiagnosed cognitive impairment in older vascular surgical patients. J Vasc Surg 2014;60:1002-11.e3.
- Luckasson R, Reeve A. Naming, defining, and classifying in mental retardation. Ment Retard 2001;39:47-52. [PubMed]
- Kaufman L, Ayub M, Vincent JB. The genetic basis of non-syndromic intellectual disability: a review. J Neurodev Disord 2010;2:182-209. [PubMed]
- Salvador-Carulla L, Bertelli M. 'Mental retardation' or 'intellectual disability': time for a conceptual change. Psychopathology 2008;41:10-6. [PubMed]
- American Psychiatric Association. Electronic dsm-iv-tr plus. 1.0 ed. Washington, DC: American Psychiatric Association; 2000.
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. [PubMed]
- Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001;135:847-57. [PubMed]
- Mitchell CK, Smoger SH, Pfeifer MP, et al. Multivariate analysis of factors associated with postoperative pulmonary complications following general elective surgery. Arch Surg 1998;133:194-8. [PubMed]
- McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med 2005;171:514-7. [PubMed]
- Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010;113:1338-50. [PubMed]
- Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 2005;102:838-54. [PubMed]
- Brooks-Brunn JA. Postoperative atelectasis and pneumonia. Heart Lung 1995;24:94-115. [PubMed]
- McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest 2006;129:48S-53S. [PubMed]
- Tai DY. Bronchoscopy in the intensive care unit (ICU). Ann Acad Med Singapore 1998;27:552-9. [PubMed]
- Kreider ME, Lipson DA. Bronchoscopy for atelectasis in the ICU: a case report and review of the literature. Chest 2003;124:344-50. [PubMed]
- Merkle NM, Schlüter M, Foitzik T. Minitracheotomy: a new interventional technique for treatment of sputum retention. Surg Endosc 1992;6:199-204. [PubMed]
- Abdelaziz M, Naidu B, Agostini P. Is prophylactic minitracheostomy beneficial in high-risk patients undergoing thoracotomy and lung resection? Interact Cardiovasc Thorac Surg 2011;12:615-8. [PubMed]
- Fiore JF Jr, Chiavegato LD, Denehy L, et al. Do directed cough maneuvers improve cough effectiveness in the early period after open heart surgery? Effect of thoracic support and maximal inspiration on cough peak expiratory flow, cough expiratory volume, and thoracic pain. Respir Care 2008;53:1027-34. [PubMed]
- Wenk M, Schug SA. Perioperative pain management after thoracotomy. Curr Opin Anaesthesiol 2011;24:8-12. [PubMed]
- Mueller XM, Tinguely F, Tevaearai HT, et al. Impact of duration of chest tube drainage on pain after cardiac surgery. Eur J Cardiothorac Surg 2000;18:570-4. [PubMed]
- Alex J, Ansari J, Bahalkar P, et al. Comparison of the immediate postoperative outcome of using the conventional two drains versus a single drain after lobectomy. Ann Thorac Surg 2003;76:1046-9. [PubMed]
- Refai M, Brunelli A, Salati M, et al. The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 2012;41:820-2; discussion 823. [PubMed]


