Is fixation an option for comminuted femoral head fracture?
Introduction
Femoral head fractures are rare but can be associated with dislocation and poor functional outcome (1). Complexity of fractures is dependent on location, size, comminution and position of hip at incidence of fracture. They usually result from stress, trauma, avulsion or more commonly sports injury and car accidents (2). They can also occur either anteriorly (leading to neck fracture and impaction of femoral head) or posteriorly (leading to femoral head fracture and eventually dislocation). Common complications with femoral head fractures are injury of sciatic nerve and ligamentous instability of the affected limb (3).
According to radiographic findings, femoral head fractures are classified by Pipkin into 4 classes: Class I, fracture inferior to fovea; Class II, fracture superior to fovea; Class III, fracture of both femoral head and neck; Class IV, fracture of femoral head and acetabulum (4).
There is no definitive optimal treatment for femoral head fractures. Non-operative treatment is limited to cases where reduction and stability of the hip joint are achieved or when the fracture is inferior to the fovea (5). While surgical intervention is mandatory in case of non-anatomic reduction of the femoral head due to existence of bone fragments or if stability of the hip is not achieved (6).
In this report, the author presents a case with class IV Pipkin fracture and the outcome of the surgical procedure immediately and 6 years after surgery.
Case presentation
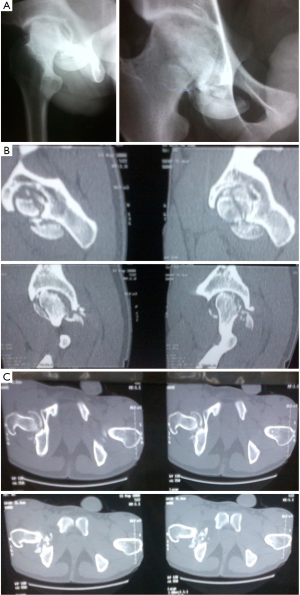
A 22-year-old male patient presented at our hospital with multiple fractures following a high-speed car accident. The patient was a driver; and he was under the treatment of chronic depression. He was slim with no history of other medical diseases. He had three fractures in his left tibia and ankle and a fracture dislocation in the right femoral head (Figure 1). There was no neurovascular deficit. The right hip joint was initially reduced in emergency department under sedation. His left ankle was swollen with compromised peripheral circulation that improved after initial reduction, plaster application and cold packs.
Fixation for all fractures was done within 12 hours from presentation (Figure 2). Fixation of the femoral head was done firstly with 4 Herbert and 2 cancellous screws through posterior approach. The hip joint was cleaned and washed to remove any debris. The large fragments were fixed while the small ones (<2 cm) were excised (Figure 3). The technique was designed in a way to avoid further damage to the articular surface. First, the large fragments were anatomically positioned leaving gaps for the missing and small fragments. Cancellous screws were introduced from entry points outside articular surface. We had to fix some relatively thin articular fragments using screws that were introduced from entry points in the articular surface. For this purpose, Herbert screws were used and buried under the articular surface. The location of the screws was designed to provide stable and rigid fixation in criss-cross manner. The hip surgery was followed by fixation of the fractures in left tibia and ankle using plates and screws.
The patient was satisfied with fixation of his left leg fractures but unhappy with the right hip fixation. He had a second opinion that created concerns about the type of hip surgery and he was questioning the possibility of having primary hip replacement rather than fixing a fracture that does not heal. He did not continue with follow up.
After 6 years, the patient showed up again at our clinic and he was thankful that the femoral head survived for 6 years and may survive longer without hip replacement. He was cured of depression but complained of pain during squatting and kneeling and inability to complete a football game. His hip was painful at extreme range of motion with no shortening of the leg.
The overall outcome was satisfactory for the patient and radiological findings were also good with united fractures although the patient had signs of arthritis in his right hip (Figure 3). He was advised to continue follow up every 6 months to evaluate any progression of arthritis and the need for hip replacement.
Discussion
Pipkin fracture is a serious injury and has been documented to have poor postsurgical outcome. The majority of cases occur as a result of car accidents in adolescence age which is young for total hip arthroplasty (THA) (1). Diagnosis of such case should not only rely on X-rays but also on CT scanning to inspect for susceptible bone fragments or major defects in the femoral head that necessitate surgical intervention. Proper diagnosis and evaluation of the patient’s conditions/comorbidities should give good understanding of the case and accurate treatment planning and help in anticipating the post-treatment results or potential complications.
Limb shortening is usually associated with fractured hip due to increased muscle forces and ligamentous instability following hip dislocation. The affected limb should be examined for any sort of skin damage, open wound or sciatic-nerve injury. The onset of intervention (either surgical or not) is crucial to alleviate pain during coma/unconsciousness period that usually follow car accidents or high-energy traumas.
Age, gender, onset and time from injury to surgery are other determining factors for successful management of Pipkin fractures (7). Fracture/dislocation of the femoral head can be determined in anteroposterior (AP) radiographic X-ray. Closed reduction has been documented to have good impact on patients with Pipkin Class I or Class II fractures (8). However, it is more believed that achieving anatomic reduction and hip joint stability can be difficult without surgical intervention. Still there is controversy in case of existence of bony fragments at the fracture site: whether bony fragments should be fixed internally or totally removed.
In the case presented, the patient showed with Pipkin Class IV fracture which usually necessitates THA. However, the patient was too young for THA and fixation seemed a more appropriate option. The outcome of the surgery was satisfactory. The fracture healed and the osteoarthritis is not severe enough to warrant joint replacement after 6 years. The functional outcome of the patient is satisfactory and he may continue on conservative treatment for several years before resorting to hip replacement.
Selecting the appropriate treatment approach is crucial to ensure restoring the joint’s function. Several treatment options were suggested for Pipkin Class IV fractures, including observation and traction or fragment excision in cases with femoral head comminution (9); a modified anterior (Smith-Petersen) treatment of isolated, displaced femoral head fractures (10); and repairing the posterior wall fracture to restore joint’s stability (11). THA has been also suggested for Pipkin Class IV fractures although it could be combined with a higher risk of infection, component loosening, multiple ossifications and limb instability, especially in young individuals as in the case presented in this work (12).
Non-operative treatment has been thought as a doubtful option to achieve anatomic reduction or to maintain stability but the experience has proven that good knowledge of anatomy of the hip and well anticipation of potential complications could help in achieving the treatment objectives without the need for surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Epstein HC, Wiss DA, Cozen L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin Orthop Relat Res 1985.9-17. [PubMed]
- Sahin V, Karakaş ES, Aksu S, et al. Traumatic dislocation and fracture-dislocation of the hip: a long-term follow-up study. J Trauma 2003;54:520-9. [PubMed]
- Roeder LF Jr, DeLee JC. Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res 1980.121-30. [PubMed]
- PIPKIN G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am 1957;39-A:1027-42 passim. [PubMed]
- Epstein HC. Posterior fracture-dislocations of the hip; long-term follow-up. J Bone Joint Surg Am 1974;56:1103-27. [PubMed]
- Gardner MJ, Suk M, Pearle A, et al. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma 2005;19:334-42. [PubMed]
- Hu H, Yang H, Wang G, et al. Analysis of influencing factors of hip functional recovery after Pipkin fracture surgery. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2012;26:433-6. [PubMed]
- Butler JE. Pipkin Type-II fractures of the femoral head. J Bone Joint Surg Am 1981;63:1292-6. [PubMed]
- Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am 1951;33-A:746-78. passim. [PubMed]
- Brumback RJ, Kenzora JE, Levitt LE, et al. Fractures of the femoral head. Hip 1987.181-206. [PubMed]
- Routt ML, Simonian PT, Hansen ST. Young patients with femoral head fractures. In: Sledge CB, ed. Master Techniques in Orthopaedic Surgery. Philadelphia, PA: Lippincott-Raven; 1998:39-153.
- Pakos EE, Pitouli EJ, Tsekeris PG, et al. Prevention of heterotopic ossification in high-risk patients with total hip arthroplasty: the experience of a combined therapeutic protocol. Int Orthop 2006;30:79-83. [PubMed]