Diagnosis of ligamentous and meniscal pathologies in patients with anterior cruciate ligament injury: comparison of magnetic resonance imaging and arthroscopic findings
Introduction
The knee joint is the largest synovial joint in the body and is the most frequent source of musculoskeletal pain. It is the numerous structures within it and their various pathologies, which result in pain and many other symptoms such as instability and restriction in range of motion (1). Important structures within the knee joint include the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial meniscus (MM) and the lateral meniscus (LM). Knee injuries are extremely common in sports, with meniscal and ligamentous tears predominating the scope of knee pathologies. For appropriate management, identification of each injury within the knee is necessary. Magnetic resonance imaging (MRI) has become the gold standard for imaging soft tissue injuries of the knee (2). In clinical practice, MRI is routinely used to diagnose or support clinical diagnoses for meniscal or ligamentous injuries prior to offering patients arthroscopic treatment. MRI serves as a useful screening tool in patients with an acute sports knee injury, allowing orthopaedic surgeons to identify those who would benefit from surgery (3-5). However, the sensitivity of MRI for the detection of meniscal injury is not yet 100%. Sportsmen have occasionally returned to play with undiagnosed meniscal lesions on the basis of a normal MRI examination (6). The sensitivity of MRI for the diagnosis of a LM has been found to be significantly lower than that for the detection of a MM tear (7-9). The lowest MRI sensitivity has been attributed to tears of the posterior horn of the LM (10-12). De Smet et al. showed that the LM tears were more frequently missed if the tear involved only one third of the meniscus or if it was located in the posterior horn (8). The presence of ACL tears, which are often associated with longitudinal tears of the LM (13), also decreases the overall sensitivity of MRI for meniscal tear detection (8-10).
While there have been numerous studies studying accuracy of the MRI of the knee, there has been only a few that have fully investigated the diagnostic accuracy of the MRI in patients with an acute ACL injury (14). One study of 41 patients with ACL tears imaged within 6 weeks of injury reconfirmed that MRI has a low sensitivity for the detection of LM tears, with all false negative cases occurring in the posterior horn (14). Furthermore, there is a paucity of literature on this subject from the Asia-Pacific region.
The objective of our study was to assess the diagnostic parameters of MRI in the diagnosis of ligamentous and meniscal lesions in patients presenting with an acute ACL injury with arthroscopic findings as a reference standard.
Methods
Before the beginning of this study, we obtained approval and a waiver of patient informed consent from our institutional review board for this retrospective study. We reviewed a database of 320 consecutive knee MRI examinations performed between 2008 and 2012 in patients who presented with a clinical history of acute ACL injury and who subsequently underwent arthroscopy-aided ACL reconstruction by the senior author of this paper. All patients had a complete rupture of the ACL on MRI. All patients presented with an acute history of twisting knee injury with or without the classical audible “pop” and had a physical finding of either a positive anterior drawer test or a positive Lachman test. Patients with frank dislocation of the knee, associated fractures about the knee and neurological deficits of the same lower limb were excluded from this study.
Each of the 320 original MRI examinations was performed using the same protocol on a 1.5-T magnet (Signa, GE Healthcare) using a 4-channel knee phased-array coil and fast spin-echo imaging. A field view of 14 cm, slice thickness of 3 mm with a 1.5 mm interslice gap, bandwidth of 20 kHz, and matrix of 256×192 were used for all four sequences except for a matrix of 256×224 for the coronal T1-weighted images. The parameters for the coronal T1-weighted images were TR range/TE, 600-700/17, 1 signal average and echo-train length of 3. The parameters for the coronal fat-saturated proton density-weighted images were 1,800-2,000/17, 1 signal average, and echo-train length of 4. The parameters for the sagittal proton density-weighted images were 2,000-2,200/17, 1 signal average, and echo-train length of 4. The parameters for the sagittal T2-weighted fat-saturated sequence were 3,000-3,400/60, 1 signal average, and echo-train length of 6. The MRI examinations were read independently by two musculoskeletal fellowship-trained radiologists who were blinded to both the original MRI interpretation and the arthroscopic findings. Each MRI study was reviewed by the radiologists twice at two different sittings spaced 1 week apart. They evaluated the integrity of the medial and lateral menisci as well as the anterior and PCLs. The reliability of measurements was assessed by intra- and interobserver variability.
Each knee arthroscopy was performed with a consistent protocol by the senior author of this paper, who is a sports surgery fellowship-trained surgeon with more than 15 years of experience with knee arthroscopy. In all knees, the menisci were visualized from the standard anterior portals and probed to expose under and upper surface tears and to evaluate the mobility of the menisci. When visualization proved difficult, or when the MRI indicated a posterior meniscal or root tear, the posterior compartment was visualized with the arthroscope placed through the contralateral portal and passed through the intercondylar notch to look down on the meniscal root. The integrity of the cruciate ligaments were checked using probes. The surgeon was aware of the MRI findings in each case and the MRI findings were often reviewed in the operating room immediately before or during the case. The arthroscopic reports and photographs were reviewed by the authors of this paper to confirm the various pathologies in each patient.
A sample of 246 subjects were estimated based on a confidence interval (CI) of 95%, expected proportion of 80% and a CI width of 0.1. Arthroscopic findings were the diagnostic reference based on which the positive predictive value (PPV), negative predictive value (NPV), sensitivity, specificity and concordance strength of association of MRI were calculated for ACL, PCL, MM and LM injuries. True positive (a) and true negative (d) was taken with reference to arthroscopic findings. False positive (b) was a positive diagnosis on MRI but negative on arthroscopy. False negative (c) was a negative diagnosis on MRI but positive on arthroscopy. The formulae used for the various parameters are as such: PPV =a/(a+b), NPV =d/(c+d), sensitivity =a/(a+c), specificity =d/(b+d), accuracy =(a+b)/(a+b+c+d), concordance =(ad–bc)/(ad+bc). Intra- and interobserver reliability for MRI assessment were measured using one way random single-measure intraclass coefficients (ICCs) with associated 95% CI to gauge the precision of the ICCs.
Results
The demographic data and clinical details of all patients included in this study are illustrated in Table 1. The epidemiology of concomitant injuries in our patients who presented with acute ACL injuries is illustrated in Table 2. Concomitant PCL injuries were diagnosed both on MRI and arthroscopy to be a Grade 2 sprain. Diagnostic parameters of MRI can be seen in Table 3. MRI findings had a significantly strong concordance of association with arthroscopic findings for both ligamentous and meniscal injuries. The majority of missed meniscus tears on MRI affected the peripheral posterior horns.
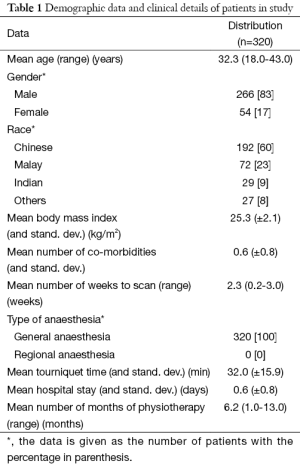
Full table
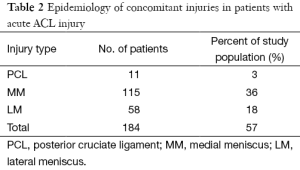
Full table
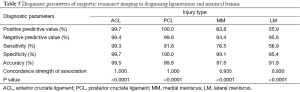
Full table
The intraclass correlation coefficient for intraobserver and interobserver reliability was 0.91 (95% CI, 0.91-0.92) and 0.87 (95% CI, 0.86-0.90). Inter- and intra-rater reliability of radiographic measurements showed excellent correlation with ICC values of more than 0.8.
Discussion
MRI has proved reliable and safe and offers advantages over diagnostic arthroscopy, which is currently regarded as the reference standard for the diagnosis of internal derangements of the knee. Arthroscopy is an invasive procedure that carries with it the risks of anaesthesia and risks of surgery such as infection, neurovascular injury and postoperative pain. It is preferably performed only for therapeutic purposes, provided that alternative non-invasive diagnostic imaging modalities such as MRI are available (15).
There have been mixed reports in current literature with regards to the diagnostic parameters of MRI when compared to arthroscopic findings. Navali et al. conducted a cross-sectional, descriptive analytical study of 120 patients with knee injury who were candidates for arthroscopy (16). The results of arthroscopy were considered as the definitive diagnosis by which the reliability of physical examination and MRI were judged accordingly. They found that both physical examination and MRI were very sensitive and accurate in the diagnosis of ligamentous and meniscal injuries with a mild preference for physical examination and concluded that MRI should be reserved for doubtful cases or complicated injuries. These findings were also resonant with that of Rayan et al. who conducted a correlational study on 131 patients with suspected traumatic meniscal or ACL injury (17). Clinical examination had better sensitivity, specificity, predictive values and diagnostic accuracy in comparison to MRI. They concluded that carefully performed clinical examination can give equal or better diagnosis of meniscal and ACL injuries in comparison to MRI scan and recommended that MRI be used to rule out such injuries rather than to diagnose them. However, Esmaili Jah et al. in their study designed to assess the value of MRI in the diagnosis of ligamentous and meniscal knee injuries in comparison with arthroscopic findings concluded that there was an excellent correlation between MRI and arthroscopic findings (18). Likewise, Khanda et al. too concluded that MRI is a good, accurate and non-invasive modality for the assessment of menisci and ligamentous injuries and that it can be used as a first line investigation in patients with soft tissue trauma to the knee (19).
In this study, all diagnostic parameters for ACL injury approached 100%. This was similar for PCL injury except that sensitivity was only 81.1%. However, the PPVs for MM and LM tears were 63.8% and 55.9% respectively. The sensitivity for MM and LM tears were 76.5% and 56.9% respectively. The overall accuracy for MM and LM tears were 87.6% and 91.8% respectively. Our results corroborates strongly with that of Sharifah et al. (20). In their study, they evaluated 65 patients with ACL injuries who underwent knee arthroscopy. Arthroscopic findings were used as the reference standard. Similar to our study, they calculated PPV, NPV, sensitivity, specificity and accuracy of MRI in the evaluation of meniscal tears. They found the sensitivity for MM and LM tears to be 83% and 82% respectively. In their study, the overall accuracy for MM and LM years were 92% and 88% respectively. The majority of missed meniscus tears on MRI affected the peripheral posterior horns, similar to our study. They concluded that the sensitivity for diagnosing a meniscal tear was significantly higher when the tear involved more than one-third of the meniscus of the anterior horn. The sensitivity was significantly lower for tears located in the posterior horn and for vertically oriented tears.
Of particular concern in our results was the low PPV and sensitivity associated with the diagnosis of LM tears. De Smet et al. conducted a study on 483 patients who had undergone MRI and arthroscopy of the knee (8). They found a significant association between a missed LM tear and a posterior horn tear or a tear involving only one third of the meniscus. They concluded that LM tears are more likely to be missed if the tear involves only one third of the meniscus or is in the posterior horn. The posterior root of the LM can be difficult to assess on MRI for multiple reasons including pulsation artefact from the popliteal artery, volume averaging and magic angle effect because of the slope of the meniscus on the tibial eminence, and the complex anatomy related to the origin of the meniscofemoral ligaments (8). Our findings come as no surprise then as all our missed LM tears were found to be in the posterior horn on arthroscopy.
Our results support the claim that combined injuries may affect the diagnosis of meniscus lesions as seen in previous studies (6-8). The accuracy of diagnosis on injured menisci, or cruciate ligaments, will depend on the quality of imaging equipment and on the skills and expertise of the radiologist and arthroscopist (18). Of particular concern is the relatively low diagnostic yield for the diagnosis of LM tears in patients with acute ACL injuries. This will be of clinical significance in decision making for patients with no residual instability who are not keen for ACL reconstruction. Decision for therapeutic arthroscopy would then depend on both clinical examination and MRI findings. The mean false positive rate for meniscal injuries in our study was 7.3%. In comparison, Chambers et at reported a false positive rate of 10.5% while Sharifah et al. reported 6.2% (20,21). Many patients presenting with an ACL tear may not have symptoms of instability and may be keen for conservative management, opting out of reconstructive surgery. In such patients, a false positive MRI finding of a torn meniscus may increase the risk of unnecessary surgery. This reiterates the adage that patient symptomatology and clinical findings are still relevant today despite the advances of medical imaging.
The strengths of our study include the standardized imaging protocol for all our knees. As all patients were from a single surgeon cohort, the effects of confounding from varying expertise of arthroscopy are also reduced. We were also adequately powered in terms of sample size. The strengths of this study must be considered in light of its limitations too. There was no control group of knees with an intact ACL. A control group would have allowed us to analyze differences in knees with and without ACL tears and further verify the statistically significant lower sensitivity of MRI for detecting meniscus tears in the setting of a concurrent ACL tear. Furthermore, there was no comparison of arthroscopic and MRI findings with clinical findings. This was due to issues related documentation in the clinical records of the patients included in this study, which made data retrieval and collection of clinical findings difficult.
Conclusions
MRI remains the gold standard for diagnosing soft tissue injuries of the knee. However, caution needs to be exercised when there is clinical evidence of a lateral meniscal injury in a patient with acute ACL injury as MRI has a relatively low PPV and sensitivity. MRI findings must always be correlated with patient symptomatology and clinical findings prior to offering surgery as there is a false positive rate ranging from 6% to 11% for meniscal tears.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Saavedra MÁ, Navarro-Zarza JE, Villaseñor-Ovies P, et al. Clinical anatomy of the knee. Reumatol Clin 2012-2013;8 Suppl 2:39-45. [PubMed]
- Kocabey Y, Tetik O, Isbell WM, et al. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy 2004;20:696-700. [PubMed]
- McNally EG, Nasser KN, Dawson S, et al. Role of magnetic resonance imaging in the clinical management of the acutely locked knee. Skeletal Radiol 2002;31:570-3. [PubMed]
- Feller JA, Webster KE. Clinical value of magnetic resonance imaging of the knee. ANZ J Surg 2001;71:534-7. [PubMed]
- Elvenes J, Jerome CP, Reikerås O, et al. Magnetic resonance imaging as a screening procedure to avoid arthroscopy for meniscal tears. Arch Orthop Trauma Surg 2000;120:14-6. [PubMed]
- Makdissi M, Eriksson KO, Morris HG, et al. MRI-negative bucket-handle tears of the lateral meniscus in athletes: a case series. Knee Surg Sports Traumatol Arthrosc 2006;14:1012-6. [PubMed]
- Oei EH, Nikken JJ, Verstijnen AC, et al. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 2003;226:837-48. [PubMed]
- De Smet AA, Mukherjee R. Clinical, MRI, and arthroscopic findings associated with failure to diagnose a lateral meniscal tear on knee MRI. AJR Am J Roentgenol 2008;190:22-6. [PubMed]
- De Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol 1994;162:905-11. [PubMed]
- Justice WW, Quinn SF. Error patterns in the MR imaging evaluation of menisci of the knee. Radiology 1995;196:617-21. [PubMed]
- Quinn SF, Brown TF. Meniscal tears diagnosed with MR imaging versus arthroscopy: how reliable a standard is arthroscopy? Radiology 1991;181:843-7. [PubMed]
- Mesgarzadeh M, Moyer R, Leder DS, et al. MR imaging of the knee: expanded classification and pitfalls to interpretation of meniscal tears. Radiographics 1993;13:489-500. [PubMed]
- Nikolić DK. Lateral meniscal tears and their evolution in acute injuries of the anterior cruciate ligament of the knee. Arthroscopic analysis. Knee Surg Sports Traumatol Arthrosc 1998;6:26-30. [PubMed]
- Rubin DA, Kettering JM, Towers JD, et al. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol 1998;170:1207-13. [PubMed]
- McMahon PJ, Dettling JR, Yocum LA, et al. The cyclops lesion: a cause of diminished knee extension after rupture of the anterior cruciate ligament. Arthroscopy 1999;15:757-61. [PubMed]
- Navali AM, Bazavar M, Mohseni MA, et al. Arthroscopic evaluation of the accuracy of clinical examination versus MRI in diagnosing meniscus tears and cruciate ligament ruptures. Arch Iran Med 2013;16:229-32. [PubMed]
- Rayan F, Bhonsle S, Shukla DD. Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. Int Orthop 2009;33:129-32. [PubMed]
- Esmaili Jah AA, Keyhani S, Zarei R, et al. Accuracy of MRI in comparison with clinical and arthroscopic findings in ligamentous and meniscal injuries of the knee. Acta Orthop Belg 2005;71:189-96. [PubMed]
- Khanda GE, Akhtar W, Ahsan H, et al. Assessment of menisci and ligamentous injuries of the knee on magnetic resonance imaging: correlation with arthroscopy. J Pak Med Assoc 2008;58:537-40. [PubMed]
- Sharifah MI, Lee CL, Suraya A, et al. Accuracy of MRI in the diagnosis of meniscal tears in patients with chronic ACL tears. Knee Surg Sports Traumatol Arthrosc 2015;23:826-30. [PubMed]
- Chambers S, Cooney A, Caplan N, et al. The accuracy of magnetic resonance imaging (MRI) in detecting meniscal pathology. J R Nav Med Serv 2014;100:157-60. [PubMed]


