Two cases of gastrointestinal stromal tumor of the small intestine with liver and bone metastasis
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract. Most gastrointestinal soft tissue neoplasms were classified as leiomyomas, schwannomas, leiomyoblastomas, or leiomyosarcomas. They are now classified as GISTs based on immunohistochemistry, histology and molecular study. They originate from the multipotential mesenchymal stem cells and differentiate to interstitial Cajal’s cells (1).
Based on size, mitotic index and anatomic location, GISTs are categorized as low, intermediate, and high risk. GISTs are generally defined as c-KIT (CD117; a tyrosine kinase receptor) positive tumors with a characteristic set of histologic features. CD34 (70%), variable expression of smooth muscle actins (SMA) (20-30%) and S100 protein (10%) are commonly positive and desmin is almost uniformly negative (only 2-4% of GISTs are positive) (2).
The incidence of GIST is in the range of 20 to 40 cases per million. Over 90% of GISTs occur in adults over 40 years old, in a median age of 63 years and rarely in children in the second decade (<1%). Most GISTs are benign; malignant tumors account for 20-30% of cases. The most common location of GIST is stomach (50-60%) and small intestine (30-40%), Other less common locations are duodenum (4-5%), rectum (4%), colon and appendix (1-2%), and esophagus (<1%). Patients have different symptoms, such as abdominal pain and swelling, weakness and anemia (3).
Cases
Case 1
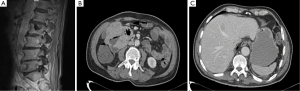
A 56-year-old male patient was examined with an abdominal swelling. The examinations and abdomen CT showed the presence of a mass in small intestine and a lesion in the liver. It was unclear whether the tumor was primary or metastatic. Sectional resection of the jejunum, ileum and liver biopsy was performed on September 2012. Histopathological examination showed epithelioid and spindle cells, 12 mitoses at 50× magnification, infiltrative growth pattern and mild cytological atypia. There was no necrosis. In the immunochemical analysis, CD 117, CD 34, SMA, EMA, CD 99 and Pan CK were positive, CK 5/6 and Glut 1 were focally positive, S100 and desmin were negative, and the Ki-67 index was 80%. Tumor diameter was 9 cm, muscle and serosal invasion were positive and the tumor persisted at the surgical margin. Pathological examination showed high-risk gastrointestinal stromal tumor of the small intestine and liver metastasis. After the surgery, Imatinib mesylate 400 mg/day was given to the patient as an adjuvant treatment. Four months after the operation, the patient had a complaint of pain in dorsal and lumbar area and right hip. MR imaging of the thorocal-lumbar vertebra and hip showed that there were metastatic lesions on the L1-L3 vertebral body and proximal of right femur. Furthermore, a PET-CT scan was performed on the patient. The results showed the existence of multiple metastatic lesions in the liver, a relapse lesion in small intestine area and increased activity in the right femur and L1-L3 vertebral body (SUVmax: 12.64). PET-CT images of patient showed in Figure 1. Palliative radiotherapy was performed at a fraction of 3 Gray (Gy) with a total dose of 30 Gy on the bone metastasis in the right femur and L1-L3 vertebral body. Afterwards, zoledronic acid 4 mg i.v. was started. Pain complaint significantly decreased after the radiotherapy. We can not take any new images after the radiotherapy because of the patient’s clinical status and he was died 2 months after the radiotherapy.
Case 2
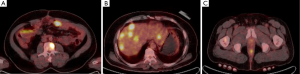
A 70-year-old male patient was examined with an abdominal pain. Examinations showed the presence of a mass in small intestine and a lesion in the liver. Afterwards, resection of the ileum and liver biopsy was performed on August 2012. Histopathological examination showed epithelioid and spindle cells, 20 mitoses at 50× magnification, infiltrative growth pattern, mild cytologic atypia and necrosis. In the immunochemical analysis, CD 117, CD 34 and SMA were positive, S100 and desmin were negative, and the Ki-67 index was 6%. Tumor diameter was 15 cm, muscle and serosal invasion were positive. Pathological examination showed high-risk gastrointestinal stromal tumor of the small intestine and liver metastasis. After the operation, Imatinib mesylate 400 mg/day was given to the patient as an adjuvant treatment. Five months after the operation the patient had a complaint of pain in lumbar area. MR imaging of the lumbar vertebras showed that there were metastatic lesions on the L2 vertebral body. MR images of patient showed in Figure 2. He had received palliative radiation therapy at the bone metastasis with a total dose of 30 Gy. Afterwards zoledronic acid 4 mg i.v. was started. Pain complaint significantly decreased after the radiotherapy. We can not take any new images, because he was died 45 days after the radiotherapy.
Discussion
Metastasis is characteristically the malignant behavior of the GIST. GISTs most frequently make metastasis to the liver and peritoneum, whereas bone and lung metastases are uncommon sites (4).
Jati et al. reported 190 GIST patients, six (3.2%) had bone metastases, four patients had multiple bone metastases, and two patients had a solitary metastasis (5).
Di Scioscio et al. reported 3 GIST cases with bone metastasis and two of them showed bone and liver metastasis at the time of disease presentation (6). In the study of Schuler at al., out of the 309 consecutive patients with metastatic GIST, 17 (5.5%) were identified to have bone metastases, 5/17 patients had synchronous metastatic disease and 17/17 patients had hepatic manifestations (7).
Our patients had liver metastasis at the time of disease diagnosis and bone metastasis in early time after the diagnosis. In our previous case study, we showed one case of GIST with bone metastasis approximately one year after diagnosis (8). CT, MRI, and especially PET-CT can be used for staging in the diagnosis and metastases scanning of GIST because of the metastasis at the same time of diagnosis and may enhance the diagnosis of tumor bone metastasis and provide more information for cancer treatment (9). Initial reports suggest F-FDG PET-CT in staging, evaluation of early response to imatinib mesylate therapy and follow-up in recurrent or metastatic GIST (10). PET-CT shows the increased metabolic activity of tumor cells and can detect both osteoblastic and osteolytic lesions at an earlier stage and useful in characterizing bone lesions that require biopsy (11). In case one, we used PET-CT after diagnosis and imatinib treatment. The results showed multiple metastatic lesions in the liver, bone metastasis and a relapse lesion in small intestine.
Limited data can be found in literature on the treatment of bone metastases in GISTs. Imatinib mesylate (Kit-selective tyrosine kinase inhibitor) can be used in the treatment of advanced, recurrent, unresectable or metastatic GIST. Imatinib mesylate has also proven efficacy in bone metastases of GIST (12,13). Other treatments include radiofrequency ablation and embolization. Radiotherapy can be used in patients with bone metastasis for palliative reasons (8).
Zoledronic acid is a bisphosphonate and penetrates osteoclast cells selectively and promotes their apoptosis by reducing bone resorption. That is the current standard therapy for osteoporosis and is used to combat hypercalcemia and bone metastases from solid tumors in the colon, breast, lung, prostate and renal cell carcinoma (14). We used zoledronic acid in both cases and the previous case.
Conclusions
In our opinion, more attention should be paid to the diagnosis of bone metastases from GIST’s in clinical practice despite the shortage of available data on the sensitivity and specificity of bone scintigraphy and PET-CT. These imaging studies must be done especially for the high-risk GISTs during the diagnosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sornmayura P. Gastrointestinal stromal tumors (GISTs): a pathology view point. J Med Assoc Thai 2009;92:124-35. [PubMed]
- Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 2006;23:70-83. [PubMed]
- Miettinen M, El-Rifai W. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol 2002;33:478-83. [PubMed]
- Bashir U, Qureshi A, Khan HA, et al. Gastrointestinal stromal tumor with skeletal muscle, adrenal and cardiac metastases: an unusual occurrence. Indian J Pathol Microbiol 2011;54:362-4. [PubMed]
- Jati A, Tatlı S, Morgan JA, et al. Imaging features of bone metastases in patients with gastrointestinal stromal tumors. Diagn Interv Radiol 2012;18:391-6. [PubMed]
- Di Scioscio V, Greco L, Pallotti MC, et al. Three cases of bone metastases in patients with gastrointestinal stromal tumors. Rare Tumors 2011;3:e17. [PubMed]
- Schuler M, Zeile M, Pink D, et al. Incidence of bone metastases in GIST: A single center analysis of 307 patients with metastatic disease. J Clin Oncol 2008;26:10565.
- Tezcan Y, Koç M. Gastrointestinal stromal tumor of the rectum with bone and liver metastasis: a case study. Med Oncol 2011;28 Suppl 1:S204-6. [PubMed]
- Van den Abbeele AD. The lessons of GIST--PET and PET/CT: a new paradigm for imaging. Oncologist 2008;13 Suppl 2:8-13. [PubMed]
- Gayed I, Vu T, Iyer R, et al. The role of 18F-FDG PET in staging and early prediction of response to therapy of recurrent gastrointestinal stromal tumors. J Nucl Med 2004;45:17-21. [PubMed]
- Peller PJ. Role of positron emission tomography/computed tomography in bone malignancies. Radiol Clin North Am 2013;51:845-64. [PubMed]
- Stamatakos M, Douzinas E, Stefanaki C, et al. Gastrointestinal stromal tumor. World J Surg Oncol 2009;7:61. [PubMed]
- Murakami M, Ebisui C, Okada K, et al. A case of liver and bone metastasis from gastrointestinal stromal tumor treated using imatinib. Gan To Kagaku Ryoho 2014;41:99-101. [PubMed]
- Machado M, Cruz LS, Tannus G, et al. Efficacy of clodronate, pamidronate, and zoledronate in reducing morbidity and mortality in cancer patients with bone metastasis: a meta-analysis of randomized clinical trials. Clin Ther 2009;31:962-79. [PubMed]