Radiographic grading of the patellofemoral joint is more accurate in skyline compared to lateral views
Introduction
Osteoarthritis (OA) of the knees is a major cause of functional disability worldwide. The nature of OA involves a degenerative “wear-and-tear” of the joint cartilage; as such it is closely associated with aging. This problem is especially prevalent in individuals who perform activities that place higher stresses on the patellofemoral joint, such as kneeling, as has been demonstrated in epidemiological as well as biomechanical studies (1,2). It has been found that patellofemoral stresses are more than 3 times that of the body weight during stair ascent and descent, and up to 8 times more on squatting (3). The patellofemoral joint is perhaps the most commonly involved compartment in OA of the knee. Overloading of the patellofemoral joint is also considered to be a risk factor for the development of tibiofemoral joint OA (4,5). Patients with patellofemoral osteoarthritis (PFOA) typically present with mechanical anterior knee pain; in fact, many of the symptoms of pain and disability associated with knee OA can be attributable to or worsened by the presence of PFOA (6-8).
Finding a less invasive yet accurate means of determining PFOA severity is a conundrum. Various methods have been used, ranging from radiographs to magnetic resonance imaging to direct visualization with knee arthroscopy. Radiographic studies are routinely ordered and are seen as the first-line investigations for PFOA, as they are the least invasive and least expensive methods of determining the severity PFOA, and studies have shown a correlation of symptoms with radiographic findings (9,10). The skyline and lateral views are commonly ordered for evaluating disease in the patellofemoral compartment.
In an attempt to quantify the severity on radiographs, many grading scales have been developed (11-13). Of these scales, the most widely used scale is the Kellgren-Lawrence (K&L) scale (13). Several studies have evaluated the correlation between K&L scale and arthroscopic findings of tibiofemoral OA (14,15). However, there are very few studies that have studied the correlation between radiographic and arthroscopic grading of PFOA.
In this study, we aim to determine the correlation of the K&L grading scale on both the skyline and lateral views with arthroscopic visualization of articular cartilage damage. We also aim to determine the diagnostic accuracy of radiographs in detecting PFOA. We hypothesized that the K&L grading will correlate with arthroscopic findings and that the skyline view will be more accurate than the lateral view in doing so.
Materials and methods
This is a retrospective study of prospectively collected data that was performed in compliance to local regulations. Our Institutional Review Board approved this study. Consent for subjects was waived as no identifiable data was collected.
The study group consisted of 63 patients (21 male and 42 female; age range, 37-67 years; average age, 52.48 years) with OA of the patellofemoral joint. Patients were investigated for OA based on their clinical signs and symptoms and diagnosis was confirmed either on radiographic or arthroscopic evaluation. A diagnosis of PFOA was made when patients complained of anterior mechanical knee pain for more than 2 months with radiographic evidence and was found to have articular cartilage degeneration of the patellofemoral joint at arthroscopy. These diagnostic criteria were used in previous studies correlating radiographic findings with arthroscopic findings in the tibiofemoral joint (12,14-17). All patients who underwent knee arthroscopy for symptomatic OA, and who had arthroscopic evidence of OA were included in this study.
The patients were selected from a database of all arthroscopic procedures performed at our institution between January 2006 and December 2010 by the senior author. There were a total of 956 patients who underwent knee arthroscopy for a variety of indications. Hospital records of these patients were reviewed to identify our study group of 63 patients who had arthroscopic evidence of PFOA and had originally presented with symptoms compatible with the diagnosis of OA. We excluded patients who had a history of trauma to the knee or other knee pathologies besides OA (such as meniscal lesions), previous knee surgery or instrumentation and other forms of arthritis (such as inflammatory, septic or gouty arthritis).
Each patient had weight-bearing skyline and lateral view radiographs of the symptomatic knee obtained with a standardized radiographic technique and positioning; lateral radiograph of the knee was taken in 30° flexion, and skyline radiograph of patellofemoral joint was taken in 30° flexion (18). All patients underwent arthroscopy of the affected knee within 1 month of the radiographic examination. The senior author of this study performed all the arthroscopic procedures. All patients were operated in supine position under general anesthesia and standard arthroscopic portals were used. At arthroscopy, the patellofemoral compartment of each patient was graded according to a modified Outerbridge classification (Table 1). The surgeon was not blinded to the clinical and radiographic findings at the time of surgery.
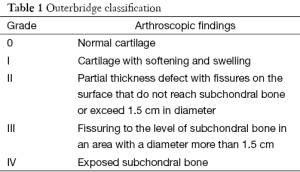
Full table
Two musculoskeletal radiologists performed a blinded review of the skyline and lateral radiographs. The radiologists were not aware of the clinical or arthroscopic findings at the time of reporting of the radiographs. The radiologists utilized the K&L grading scale (Table 2) to determine the presence and severity of OA of the patellofemoral joint in each patient for both lateral and skyline views. The radiologists were not blinded to their individual scoring and a conclusively agreed upon score was presented to the clinicians for further evaluation.

Full table
The radiographic grade of PFOA was represented by the numerical value of the K&L grade. The arthroscopic grade of articular cartilage degeneration in the patellofemoral compartment of the knee according to the Outerbridge classification was assigned as the numerical severity of OA in the patellofemoral joint.
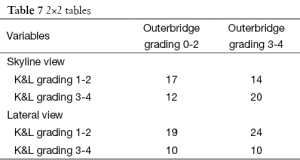
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) Version 20 (IBM® SPSS Statistics, Armonk, New York, USA). The alpha was set to 0.05 for our statistical analyses. The correlation between K&L grading of lateral and skyline radiographs and severity of articular cartilage degeneration were evaluated using the Spearman’s correlation. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were evaluated with 2×2 tables that were drawn up comparing the test results (i.e., K&L grading) with the true disease status (i.e., the arthroscopically visualized Outerbridge grading) for both skyline and lateral views. From these tables, the true positives (a), true negatives (d), false positives (b) and false negatives (c) were used to calculate the sensitivity, specificity, PPV, NPV and accuracy. The formulae used for the various parameters are as such: PPV = a/(a+b), NPV = d/(c+d), sensitivity = a/(a+c), specificity = d/(b+d) and accuracy = (a+ b)/(a+b+c+d).
Results
Table 3 shows the mean numeric values (with standard deviation) demonstrating the severity of articular cartilage degeneration within the patellofemoral joint for skyline and lateral radiographic grade of OA respectively according to the K&L scale. In general, the higher the K&L grading on skyline and lateral radiographs, the greater the severity of articular cartilage degeneration on arthroscopy.
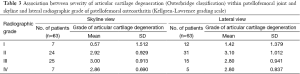
Full table
The Spearman correlation coefficients illustrating the relation between the Outerbridge Classification and the K&L grading scale was 0.263 (P<0.037; 95% CI, 0.017-0.479) for skyline radiographs and 0.222 (P=0.040; 95% CI, 0.027-0.445) for lateral radiographs. This suggests that increasing K&L grade accounts only for 26.3% (on skyline view) and 22.2% (on lateral view) of the variation of severity of arthroscopically determined articular cartilage degeneration. Figures 1,2 illustrate the disparity between radiographic and arthroscopic findings.
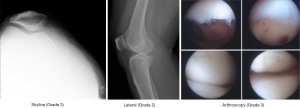
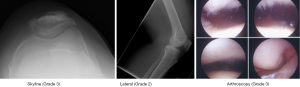
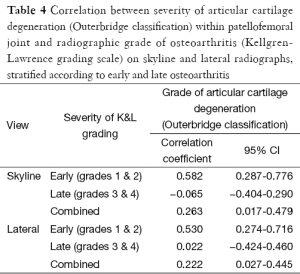
Table 4 shows the correlation coefficients after stratification according to severity of radiographically graded OA. The patients were stratified into early OA (K&L grades 1 and 2) and late OA (K&L grades 3 and 4) and analyzed. On both skyline and lateral views, radiographs with early OA had higher correlation coefficients than radiographs with late OA. The correlation coefficients are 0.582 (P<0.01; 95% CI, 0.287-0.776) and 0.530 (P<0.01; 95% CI, 0.274-0.716) for skyline and lateral radiographs respectively.
Full table
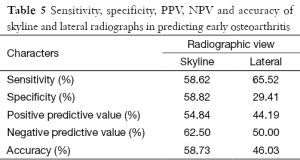
Table 5 shows the sensitivity, specificity, PPV, NPV and accuracy of skyline and lateral radiographs in predicting early OA. Skyline radiographs were superior to lateral radiographs in terms of specificity (58.82% vs. 29.41%), PPV (54.84% vs. 44.19%) and NPV (62.50% vs. 50.00%), but inferior in terms of sensitivity (65.52% vs. 58.62%). The accuracy of skyline radiographs was determined to be superior to that of lateral radiographs (58.73% vs. 46.03%).
Full table
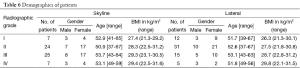
Table 6 shows the demographic details of our subjects with a trend of higher body mass index with increased radiographic grades. Table 7 shows the 2×2 contingency tables categorizing early and late staged of OA by radiography and arthroscopy.
Full table
Full table
Discussion
Of the many scales used to classify severity of radiographic OA, the most widely used is the K&L grading scale. There are studies, which have evaluated the correlation between K&L scale and arthroscopic findings in tibiofemoral OA, but to our knowledge, no studies have been done on PFOA (12-20). Studies by Brandt et al. and Blackburn et al. found that plain radiographs were insensitive tools in detecting articular cartilage damage (12,14). However, a study by Jones et al. did allude that skyline radiographs were more reproducible and allowed for more precise localization of change than lateral radiographs (18). With this information in mind, we aimed to determine the correlation of the K&L grading scale on both the lateral and skyline views with arthroscopic visualization of articular cartilage damage as well as the diagnostic accuracy of radiographs in detecting PFOA.
Based on the results of our study, there is a positive correlation between K&L grade and arthroscopic cartilage degeneration in both skyline and lateral radiographs. There is a general trend of increasing arthroscopic grade of articular cartilage degeneration as K&L grade increases. However, we find that there is a discrepancy between the radiographic grades and arthroscopic grades and this could possibly be explained by a disparity in the sample size, as is observed by the fact that skyline grade 3 radiographs and lateral grade 2 radiographs have the highest numbers as compared to the other grades.
The correlation between K&L grading and arthroscopic grading in our study has been found to be about 40% on skyline radiographs and 29% on lateral radiographs; this figure is low compared to previous studies that looked at the tibiofemoral joint. In a recent study by Kijowski et al., the K&L grade and arthroscopic grade had a correlation coefficient of 0.49 (20). Our study shows a correlation coefficient of 0.40 and 0.29 for the skyline and lateral view respectively. This is a rather weak correlation but it is unsurprising, as a similar trend has been reported in the literature between radiographic findings and arthroscopic findings (19). The figure is in a similar range as previous studies that looked at the tibiofemoral joint (12-20). The authors of these studies criticized the K&L scale for placing too much emphasis on presence of osteophytosis over joint space narrowing, which is thought to reflect the degree of wear of the cartilage, a key pathologic process in the development of OA. Kallman et al. state that according to the K&L grading, if osteophytes are not present, “the joint must be graded as negative for OA” (21). Thus in the absence of osteophytes, the K&L grading fails to account adequately for joint space narrowing or sclerosis. We postulate that some patients may have more joint space narrowing than osteophyte growth. This is a possible explanation for the relatively weak correlation seen between radiographic K&L grading and arthroscopic articular cartilage degeneration seen in our study.
Interestingly, after stratification of the K&L grading of radiographs according to early and late OA, there is a significant increase in the correlation coefficient of radiographically determined early OA and arthroscopically graded articular cartilage degeneration. This may imply that radiographs are more useful in assessing the severity of OA in the early stage of the disease, and other modalities might be better suited to picking up late stage OA. There is no evidence in the literature that could offer an explanation for our observation. We postulate that it could be the fact that radiographs with early disease and minimal damage to the joint are more easily recognized and graded than radiographs with late disease with extensive osteophytes and joint space narrowing. It is probably easier to grade a pristine joint with the K&L scale than it is to grade a joint with multiple osteophytes, in which the assessor has to decide if the osteophyte is “moderate” or “large” in size, or if the joint space shows “definite narrowing” or “marked narrowing”. Furthermore, due to the two dimensional nature of radiographs, it may be difficult to distinguish the size of an osteophyte from a single view; whereas in terms of early OA, it is easy to decide if there is an absence of osteophytes, or if there is just a tiny osteophyte.
Statistical analyses of our results showed that skyline radiographs were superior to lateral radiographs in terms of specificity, PPV, NPV and accuracy, losing out only in terms of sensitivity. In particular, skyline radiographs were over 10% more accurate than lateral radiographs. This finding is supported by previous radiographical studies, which concur with the preferential use of skyline over lateral radiographs (22). Mid-flexion lateral radiographs were found to have poor reproducibility in assessing in joint space narrowing, and authors have suggested that it is of little value in detecting OA progression (23,24). Furthermore, it has been shown that skyline radiographs, as compared to lateral radiographs, are significantly better at identifying symptomatic OA, detecting joint space loss and osteophytosis as well as assessing progression of PFOA (25-27).
Our study identifies a closer correlation of radiographic grade with arthroscopic grade in early, rather than late, OA. This is an important finding, as it would help in decision-making with regards to investigation of PFOA. Since correlation is better with early OA, these patients can probably be evaluated satisfactorily with plain radiographs. On the other hand, perhaps other modes of diagnostic imaging should be utilized in evaluating patients with characteristic symptoms of PFOA (persistent anterior knee pain that is made worse with climbing and squatting) but minimal evidence of PFOA. This is assuming that patients with late PFOA present with persistent anterior knee pain. Magnetic resonance imaging and diagnostic/therapeutic arthroscopy are viable but more expensive options. One author has even suggested the use of outpatient arthroscopy as a modality of investigation for PFOA (14).
Contrary to our results, McDonnell et al. found that “skyline patellofemoral radiographs can only exclude late stage degenerative changes” (26). McDonnell et al. (26) compared radiographic grading of patellofemoral OA using the Ahlback score, with operative assessment of cartilage using the modified Collins grade (11,27). An Ahlback score of 1 or more (evidence of joint space narrowing) was taken as a positive radiographic diagnosis of arthritis; a Collins Grade of 4 was taken as the cutoff for late cartilage degeneration. They identified that their study was limited by the fact that none of the radiographs were graded as Ahlback 3 or more. However, we feel it is inaccurate to claim that skyline patellofemoral radiographs can only exclude late stage degenerative stages, as there were no cases of severe radiographic OA to compare to. We present a study sample with a diverse range of grading, and thus may provide a more accurate view on radiographic evaluation of patellofemoral OA.
A limitation of our study was the presence of possible selection bias. Due to the needs of our study, we only included symptomatic patients who had arthroscopic evidence of PFOA. This contributes to selection bias rendering our study population to be non-representative of the actual population of patients with PFOA. In addition, our sample size is small (63 patients), which could have possibly influenced the precision of the results. The reason for a small sample size is because there is a hesitancy to offer arthroscopic surgery for patients with PFOA due to a lack of evidence that supports the routine application of arthroscopy. A recent paper by Kirkley et al. shows that arthroscopic surgery for OA provides no additional benefit (28). Another criticism that is to be expected from our readers is the application of the K&L grading system in evaluating PFOA. The original paper by Kellgren and Lawrence, did not include skyline and lateral radiographs in the grading system (13). In addition, Crossley et al. claimed that most radiographic scoring systems may not be reliable for the patellofemoral joint, as they were originally developed to assess tibiofemoral OA (29). We acknowledge these points, but we note that in the case of Crossley et al., there were no studies quoted to support his claim and thus was likely the author’s own opinion. We feel that since the original description of K&L grading was theoretically sound in reflecting the pathophysiology of PFOA and the fact that K&L grading has been used in previous radiographic studies, it could be applied satisfactorily to the evaluation of skyline and lateral radiographs (25).
Conclusions
Radiographs generally have a poor correlation with arthroscopic findings in PFOA. However, they seem to have a better correlation in early PFOA. The skyline view has a better accuracy than the lateral view in assessing PFOA. We advocate the use of radiographs, especially the skyline view in of the assessment of early OA. Further studies are needed to evaluate other modalities of imaging in the assessment of both early and late PFOA to guide management strategies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jensen LK. Knee osteoarthritis: influence of work involving heavy lifting, kneeling, climbing stairs or ladders, or kneeling/squatting combined with heavy lifting. Occup Environ Med 2008;65:72-89. [PubMed]
- Kajaks T, Costigan P. The effect of sustained static kneeling on kinetic and kinematic knee joint gait parameters. Appl Ergon 2015;46 Pt A:224-30.
- Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand 1972;43:126-37. [PubMed]
- Szebenyi B, Hollander AP, Dieppe P, et al. Associations between pain, function, and radiographic features in osteoarthritis of the knee. Arthritis Rheum 2006;54:230-5. [PubMed]
- Mazzuca SA, Brandt KD, Katz BP, et al. Comparison of quantitative and semiquantitative indicators of joint space narrowing in subjects with knee osteoarthritis. Ann Rheum Dis 2006;65:64-8. [PubMed]
- Duncan R, Peat G, Thomas E, et al. How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatology (Oxford) 2008;47:1704-7. [PubMed]
- Englund M, Lohmander LS. Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Ann Rheum Dis 2005;64:1721-6. [PubMed]
- McAlindon TE, Snow S, Cooper C, et al. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis 1992;51:844-9. [PubMed]
- Cicuttini FM, Baker J, Hart DJ, et al. Choosing the best method for radiological assessment of patellofemoral osteoarthritis. Ann Rheum Dis 1996;55:134-6. [PubMed]
- Lanyon P, O'Reilly S, Jones A, et al. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis 1998;57:595-601. [PubMed]
- Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968.Suppl 277:7-72. [PubMed]
- Brandt KD, Fife RS, Braunstein EM, et al. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum 1991;34:1381-6. [PubMed]
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [PubMed]
- Blackburn WD Jr, Bernreuter WK, Rominger M, et al. Arthroscopic evaluation of knee articular cartilage: a comparison with plain radiographs and magnetic resonance imaging. J Rheumatol 1994;21:675-9. [PubMed]
- Wada M, Baba H, Imura S, et al. Relationship between radiographic classification and arthroscopic findings of articular cartilage lesions in osteoarthritis of the knee. Clin Exp Rheumatol 1998;16:15-20. [PubMed]
- Fife RS, Brandt KD, Braunstein EM, et al. Relationship between arthroscopic evidence of cartilage damage and radiographic evidence of joint space narrowing in early osteoarthritis of the knee. Arthritis Rheum 1991;34:377-82. [PubMed]
- Lysholm J, Hamberg P, Gillquist J. The correlation between osteoarthrosis as seen on radiographs and on arthroscopy. Arthroscopy 1987;3:161-5. [PubMed]
- Jones AC, Ledingham J, McAlindon T, et al. Radiographic assessment of patellofemoral osteoarthritis. Ann Rheum Dis 1993;52:655-8. [PubMed]
- Kijowski R, Blankenbaker D, Stanton P, et al. Correlation between radiographic findings of osteoarthritis and arthroscopic findings of articular cartilage degeneration within the patellofemoral joint. Skeletal Radiol 2006;35:895-902. [PubMed]
- Kijowski R, Blankenbaker D, Stanton P, et al. Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol 2006;187:794-9. [PubMed]
- Kallman DA, Wigley FM, Scott WW Jr, et al. New radiographic grading scales for osteoarthritis of the hand. Reliability for determining prevalence and progression. Arthritis Rheum 1989;32:1584-91. [PubMed]
- Buckland-Wright C. Which radiographic techniques should we use for research and clinical practice? Best Pract Res Clin Rheumatol 2006;20:39-55. [PubMed]
- Cooper C, Cushnaghan J, Kirwan JR, et al. Radiographic assessment of the knee joint in osteoarthritis. Ann Rheum Dis 1992;51:80-2. [PubMed]
- Altman RD, Fries JF, Bloch DA, et al. Radiographic assessment of progression in osteoarthritis. Arthritis Rheum 1987;30:1214-25. [PubMed]
- Cahue S, Dunlop D, Hayes K, et al. Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum 2004;50:2184-90. [PubMed]
- McDonnell SM, Bottomley NJ, Hollinghurst D, et al. Skyline patellofemoral radiographs can only exclude late stage degenerative changes. Knee 2011;18:21-3. [PubMed]
- Collins DH, Mcelligott TF. Sulphate (35SO4) uptake by chondrocytes in relation to histological changes in osteoarthritic human articular cartilage. Ann Rheum Dis 1960;19:318-30. [PubMed]
- Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 2008;359:1097-107. [PubMed]
- Crossley KM, Hinman RS. The patellofemoral joint: the forgotten joint in knee osteoarthritis. Osteoarthritis Cartilage 2011;19:765-7. [PubMed]


