Minimally invasive thoracic surgery: new trends in Italy
Presentation text (Figure 1)

Aim of my talk is to provide an overview of the most recent trends existing in Italy on minimally invasive thoracic surgery. In order to apply an objective method to investigate this multifaceted issue, a web search was made on PubMed including all articles dealing with minimally invasive thoracic surgery, which were recently published in reference journals. The key words used for the web search were minimally invasive thoracic surgery, thoracoscopy, video-assisted thoracic surgery (VATS) and Italy. This is in order to pick-up the vast majority of scientific articles dealing with minimally invasive thoracic surgery, which included at least one Italian author. The time span chosen was since January 2013 up to June 2015.
Background
Italy has quite a long and rich history regarding use of thoracoscopy and minimally invasive thoracic surgery. As it happened in other Countries, the very first thoracoscopic procedures entailed the intrapleural pneumolysis also known as the Jacobaeus operation that consisted in the division by cautery of intrathoracic pleural adhesions under thoracoscopic vision. This is in order to improve the effectiveness of the Forlanini’s artificial pneumothorax for treatment of pulmonary tuberculosis in the pre-antibiotic era.
In 1928, an iconographically appreciable atlas of thoracoscopy is that published by Felix Cova (2), which includes beautiful color art drawings illustrating the operative findings that were more frequently encountered when performing thoracoscopy (Figure 2).
Several decades later, the advent of video-technology at the end of the years 1980’s coincided with the birth of VATS. In Italy, the first papers published on this topic include in 1989 that of Torre and Belloni (3) on use of YAG laser pleurodesis by VATS for treatment of spontaneous pneumothorax, that of Roviaro and coworkers (4) who first proposed in 1992 VATS lobectomy for surgical treatment of lung cancer, and that of Peracchia and coworkers (5) who were amongst the first to report on use of VATS in esophageal surgery.
Web search
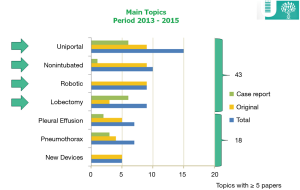
The web search identified 108 articles published on PubMed. Out of these there were 49 (45%) original articles, 8 (16%) of which were multi-institutional trials, 18 (17%) review articles and 41 (38%) case reports.
When looking at the main areas of investigation, there were 15 papers dealing with uniportal VATS, 10 papers dealing with nonintubated VATS, 8 papers dealing with robotic and other 8 with VATS lobectomy in general, respectively (Figure 3). Amongst secondary topics there were thymectomy, chest wall surgery, sympathectomy, lung metastasectomy, mediastinal biopsy, treatment of emphysema and lung cancer staging.
Looking at a geographical distribution of the corresponding authors’ Institution, according to a decreasing number of published papers there were 30 papers published from Rome, 17 from Milan and 10 from Naples whereas other cities from which there were at least 4 published articles included Turin, Pisa, Bologna and Palermo (Figure 4).
Uniportal VATS
Uniportal VATS is increasingly employed to perform thoracic surgery procedures including lobectomy and segmentectomy. So far, a widespread adoption of uniportal VATS is hampered by some limitations including the crowding of instrumentation through a single access that makes surgical maneuvering more technically demanding than with multiportal VATS, difficulty in digital lung palpation, suboptimal angulation of staple insertion for division of pulmonary vessels, and urgent management of unexpected major bleeding complications. Nonetheless, Uniportal VATS can offer the advantage of minimizing the extent of the surgical access thus resulting in less postoperative pain, early recovery and better cosmesis although so far no randomized study has been performed in an attempt to confirm potential advantages over multiportal VATS.
The largest published series is that of Rocco and coworkers (6) who reported in 2013 on 644 VATS procedures performed by this approach. It is worth noting that so far uniportal VATS in Italy has been not so commonly employed to perform lobectomy but rather for minor thoracic procedures including pulmonary wedge resection, management of recurrent pleural effusion and treatment of spontaneous pneumothorax.
In the series from Rocco and coworkers (6) conversion, mortality and morbidity rates were 3.7%, 0.6% and 2.8%, respectively whereas hospital stay ranged between 3.4 and 5.3 days.
Future perspectives of uniportal VATS include the development of novel tailored instrumentation and flexible platforms, which might significantly improve ergonomics and flexibility of this strategy.
A recent publication from Ibrahim and coworkers (7) reported on clinical experimental use of a flexible endoscope to improve visualization of hilar structures during VATS lobectomy. This preliminary series entailed 15 operated patients. The mean operative time was 112 minutes, there was no major morbidity whereas drainage time and hospital stay were 2.8 and 3.2 days, respectively.
In a further noteworthy study, Bertolaccini and coworkers (8) performed an ergonomic assessment of single-port versus 3-ports access VATS procedures in 100 patients (50 patients per group) excluding from the analysis major lung resections. A multidimensional scoring system developed by the National Aeronautics and Space Administration (NASA) has been employed in this study to grade amongst the thoracic surgeons who performed the procedures, 6 main domains including mental demand, physical demand, temporal demand, effort, performance and frustration level. The study results showed that physical demand was greater in 3-ports VATS whereas the frustration level was higher in single-port VATS leading the authors to conclude that the surgeon can maintain a more neutral body posture during uniportal VATS by standing straight and facing the monitor with only minimal neck extension/rotation. On the other hand, the frustration originated by the greater difficulty in surgical maneuvering during single-port VATS is also of concern.
Non-intubated thoracic surgery (NITS)
NITS is aimed at offering an ultra-minimally invasive surgical management by adding to the advantages of minimally invasive thoracic surgery approaches, those achievable by operating through regional anesthesia methods in fully awake or mildly sedated, spontaneously ventilating patients. This is to avoid side-effects of intubated general anesthesia with single-lung mechanical ventilation and, ultimately, fasten recovery, reduce costs and optimize outcomes.
The main physiologic difference between NITS strategies and intubated general anesthesia is that with the latter the diaphragm is pharmacologically paralyzed and ventilation is mechanically driven, whereas with the formers spontaneous ventilation and an efficient contraction of the diaphragm are preserved.
There are several theoretical advantages of NITS including an easier acceptance of surgery; a reduced need of high-dependency stay postoperatively; a better respiratory function in the early postoperative period; reduced mortality and morbidity; shorter hospital stay; lower procedure-related costs; an attenuated early stress hormone and immune response; and possibly a better survival in oncologic surgery.
Several studies have shown optimal feasibility and satisfactory results of a number of NITS procedures ranging from simple management of pleural effusion and of spontaneous pneumothorax to more demanding procedures such as lung volume reduction surgery, thymectomy, lobectomy and even sleeve lobectomy, and tracheal resection.
Rates of conversion to intubated general anesthesia were reported to be from 2.3% to 10.0%, depending both on the type of procedure and the experience of the surgical team.
Despite the evidence of optimal feasibility and tolerability, indications for NITS are far to be definitively delineated.
The analysis of the most recent literature indicated some promising useful applications of NITS strategies. One entails the treatment of patients with impaired pulmonary function such as those with emphysema who are candidate for lung volume reduction surgery or lung cancer resection (9) for whom general anesthesia per se can carry significant risks of morbidity. Another entails hemodynamically stable patients with haemothorax suitable of thoracoscopic exploration particularly if they suffer of concomitant sepsis and respiratory failure for which NITS management could reduce the risk of ICU stay, intubation and ventilator assistance. In a recent study from our institution (10), patients requiring VATS lung biopsy due to undetermined interstitial lung disease proved optimal candidates for NITS since this patients’ subgroup has been shown to carry significant risks of morbidity and mortality in series entailing surgical biopsy under general anesthesia.
Contraindications for NITS include, hemodynamic instability, morbid obesity with body mass index >25; non-compliant patients; and in centers that are performing lung cancer resections, the presence of large and centrally located tumors greater than 6 cm in maximal size.
In a survey amongst European Society of Thoracic Surgeons (ESTS) members, published this year (11) the current trends, rates of adoption and potential future expansion of NITS have been investigated. Out of 105 responders, 68 admitted to have already employed NITS. Thoracoscopic management of recurrent pleural effusion, pleural decortication for empyema thoracis and lung biopsy for interstitial lung disease were indicated as the more frequently performed procedures. Poor-risk patients due to co-morbidity and elderly patients were considered as the ideal candidates for NITS whereas a faster, recovery, reduced morbidity and shorter hospital stay with decreased costs were indicated as the main potential advantages. As the main technical disadvantages, responders indicated coughing and poor maneuverability due to diaphragmatic and lung movements. Sixty-eight percent of responders believed that NITS procedures will be likely to increase in the near future.
Robotic thoracic surgery
Adoption of robot technology in thoracic surgery has been introduced to overcome some limitations of VATS like use of rigid instruments and suboptimal vision, while keeping the advantages of a low invasiveness. More intuitive maneuverability, greater flexibility and high definition three-dimensional vision are deemed other advantages of the robotic approach.
As far as surgical treatment of lung cancer is concerned, preliminary reports have suggested that robotic lobectomy and segmentectomy are feasible and safe with long term outcome similar to that of VATS approaches although no randomised comparison with standard VATS has been yet accomplished.
In a recent review article by Veronesi (12), it is emphasizes that according to recently published findings, the robotic approach proved a good and safe alternative to VATS and might be considered an easier and more intuitive procedure to afford difficult cases or anatomical segmentectomy. However, so far there is no data on long term results following robotic resection for lung cancer.
The main limitation of robotic procedures is still represented by higher costs of the technique compared to sole VATS. In a recent multicenter analysis among 15,502 lung surgery cases, costs related to robotic assistance, which was employed in 4% of instances proved significantly greater (25,040 vs. 20,476 USD for standard VATS) (13).
Other current limitations include the need of multiportal approaches and the excessive encumbrance of the robotic arms and of the overall apparatus. It seems reasonable to assume that currently, robotized VATS cannot probably add major advantages over standard VATS. However, robotic technology is rapidly evolving and it is likely that evolutionary robotized systems will probably overcome most of the limitations that we address today to this technology. For this reason, continuing active research in this exciting field is warranted and hopefully specific training with robot-assisted procedures will be increasingly included in future postgraduate thoracic surgery training programs.
VATS lobectomy in Italy
Finally, I would like to present some data retrieved from the Italian experience on VATS lobectomy that has been collected by the Italian VATS group registry. Up to September 2015 the registry had collected an overall number of 1,668 thoracoscopic lobectomies performed in over 70 Italian Institutions. Overall, it is worth of noting that although only 23 institutions have performed more than 25 procedures, adoption of VATS lobectomy is rapidly increasing in Italy and quite many thoracic surgeons are currently involved in active VATS lobectomy programs entailing use of either multiport or uniportal approaches. On the other hand, adoption of anatomical VATS segmentectomy in Italy is still not as common as in China and in other Asian countries although I cannot show precise figures on this regard. Nonetheless, the wider diffusion of screening programs and detection of early stage lung cancer patients will reasonably lead to an increasing adoption of these options also in Italy.
Conclusions
According to a PubMed search on studies published within the last 3 years by Italian surgeons on minimally invasive thoracic surgery, uniportal, nonintubated, and robotic VATS approaches as well as VATS lobectomy, represented the most frequently investigated issues. Several Italian thoracic surgeons are actively involved in clinical investigations on minimally invasive thoracic surgery and have provided noteworthy results, new ideas and promising technical refinements.
Continuing investigation in each of the sub-topics identified by this web search is contributing to define more precisely indications advantages and disadvantages of each approach and it is likely that combination strategies including adoption of uniportal and nonintubated approaches will help define novel ultra-minimally invasive thoracic surgery strategies.
Acknowledgements
I thank Prof. Roberto Crisci from the University of Aquila who kindly provided me the data of the Italian VATS group. I also apologize to the many Italian authors who have published valuable papers on minimally invasive thoracic surgery but have not been mentioned extensively. The reason is to be mainly attributed to the time limitation of my presentation. I also would like to clarify that the selection of papers presented more in detail within each main topic discussion has been liberally made by myself and thus represents an arbitrary choice.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Pompeo E. Professor Eugenio Pompeo’s live presentation on “Minimally Invasive Thoracic Surgery: New Trends in Italy” in the Eagle Forum. Asvide 2015;2:124. Available online: http://www.asvide.com/articles/700
- Cova F. Atlas thoracoscopicon. Milano: Sperling & Kupfer Eds., 1928.
- Torre M, Belloni P. Nd:YAG laser pleurodesis through thoracoscopy: new curative therapy in spontaneous pneumothorax. Ann Thorac Surg 1989;47:887-9. [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Peracchia A, Ancona E, Ruol A, et al. Use of mini-invasive procedures in esophageal surgery. Chirurgie 1992;118:305-8. [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [PubMed]
- Ibrahim M, Menna C, Andreetti C, et al. Flexible videoscope for thoracoscopic lobectomy: evolution of uniportal technique. Surg Endosc 2015;29:2056-9. [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [PubMed]
- Pompeo E, Rogliani P, Palombi L, et al. The complex care of severe emphysema: role of awake lung volume reduction surgery. Ann Transl Med 2015;3:108. [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery-A survey from the European Society of Thoracic Surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Pompeo E, Rogliani P, Cristino B, et al. Awake thoracoscopic biopsy of interstitial lung disease. Ann Thorac Surg 2013;95:445-52. [PubMed]
- Veronesi G. Robotic lobectomy and segmentectomy for lung cancer: results and operating technique. J Thorac Dis 2015;7:S122-30. [PubMed]
- Swanson SJ, Miller DL, McKenna RJ Jr, et al. Comparing robot-assisted thoracic surgical lobectomy with conventional video-assisted thoracic surgical lobectomy and wedge resection: results from a multihospital database (Premier). J Thorac Cardiovasc Surg 2014;147:929-37. [PubMed]



