Prognostic factors in patients with thoracic esophageal carcinoma staged pT1-4aN0M0 undergone esophagectomy with three-field lymphadenectomy
Introduction
Esophageal cancer is one of the most common malignancies in china, accounting for around 50% of incidence world-wide (1). Surgery is still one of the principal treatment methods for patients with esophageal cancer. Patients with thoracic esophageal cancer were found to have relatively high cervical lymph node metastasis rate, ranging from 17.2% to 49.5% (2-4). The number of metastatic lymph nodes is a principal prognostic factor predicting the outcome of surgery (5,6). While report based on mass cases had never been found on prognostic factors in patients neither with lymph node metastasis nor distant metastasis (pT1-4aN0M0). Compared with traditional 2-field lymphadenectomy, esophagectomy plus lower cervical, mediastinal and upper abdominal lymph node resection, i.e., 3-field lymphadenectomy exhibits better surgical exposure, and is also considered to play a pivotal role in understanding the nodal metastatic pattern, and determining postoperative staging as well (2-4).
Materials and methods
Patient population
Seven hundred and seventy patients, diagnosed of thoracic esophageal squamous cell carcinomas only, had undergone subtotal esophagectomy plus 3-field lymphadenectomy, and pathologically staged of pT1-4aN0M0 were entered into the study to find out the possible prognostic factors and the value of prophylactic postoperative radiotherapy. The study was performed in accordance with the Declaration of Helsinki and was approved by the ethics committee of Fujian Provincial Cancer Hospital. All patients provided written consent for storage of their information in the hospital database and for use of this information in our research.
Patients were involved in this study if they: (I) had received radical esophagectomy and 3-field nodal dissection in the first treatment; (II) had no evidence of distal hematogenous metastasis found in preoperative chest CT scanning, abdominal CT scanning and systematic ECT bone scanning; (III) with a strictly pathological diagnosis of squamous cell carcinoma only and no evidence of nodal metastasis; (IV) had not received radiotherapy or chemotherapy before surgery or chemotherapy after surgery; and (V) had untaken more than 15 lymph nodes removed in surgery. From January 1993 to March 2007, 2,665 patients with thoracic esophageal squamous cell carcinoma were treated with surgery at Fujian Province Cancer Hospital, Fuzhou, Fujian, China. A total of 1,090 cases of pathological diagnosis of lymph node metastasis, only 770 cases met with our criteria, 320 were excluded from this analysis for having received preoperative chemotherapy or radiation (156 cases), postoperative chemotherapy or postoperative concurrent chemoradiation (30 cases), surgical procedures other than an extended esophagectomy with 3-field lymphadenectomy that included removal of at least 15 nodes (126 cases), having had other malignancies before the diagnosis of esophageal cancer, or having had disease of mixed histology (4 cases), R2 resection (4 cases). Of those 770 patients, 687 had received surgery only (aged 28-84 years, median 57 years), and 83 patients had undergone surgery followed by postoperative radiation therapy (aged 32-78 years, median 53 years). Altogether, 18,893 nodes had been removed, with a mean of 24.5 nodes per patient (range, 15-68).
Surgical procedure
The surgery included a subtotal esophagectomy, together with cervico-thoraco-celiac (3-field) lymphadenectomy. It started with a right posterolateral thoracotomy through the 5th intercostal space. When the thoracic maneuver was completed, the patient was repositioned for median laparotomy and cervical lymph node resection by means of a collar incision. Lymph node stations dissected in the superior mediastinum included the right and left pararecurrent laryngeal nerve nodes, the paratracheal nodes, and the paraesophageal nodes, in the mid-mediastinum included the subcarinal nodes and the paraesophageal nodes, and in the inferior mediastinum included the paraesophageal nodes and the diaphragm nodes. Lymph node stations dissected in the abdomen included the paracardiac nodes, the lesser curvature nodes, and the left gastric artery nodes. Lymph node stations dissected in the neck included the right and left supraclavicular nodes and cervical paraesophageal nodes (the deep cervical nodes) (2).
Radiotherapy methods
Radiotherapy was started 3-4 weeks postoperatively. The median radiation dose to the tumor bed was 50 Gy in 25 fractions at 2 Gy per fraction, 5 days a week.
Statistical analysis
The various clinical features of patients with esophageal cancer were input into the computer. Overall survival was calculated from the day of surgery to day of death or day of loss of follow-up or final day of follow-up. Follow-up and Survival condition Statistical analysis was performed using SPSS 15.0 (SPSS, Inc., Chicago, IL). Kaplan-Meier analysis was performed to estimate the survival rate, and the log-rank test was performed to calculate significance. Cox proportional hazards analysis was performed to calculate the hazard ratio (HR) and CI. The χ2 test was used to compare the reasons of treatment failure between two groups.
Results
Follow-up and survival condition
All patients took clinic visit every 3-6 months for 1-2 years, every 6-12 months for 3-5 years. They regularly received chest CT scanning, abdominal CT scanning and systematic ECT bone scanning every 3-6 months and had esophagogastroscopy every year. Until the final day of follow-up on March 1, 2009, the number of cases of 1, 3, 5, 10 years follow-up was 633, 444, 258 and 75, respectively. Lymph node metastasis, local recurrence and hematogenous metastasis were judged according to clinical signs and various kinds of imaging examinations. For the entire study patients, the overall survival rates at 1, 3, 5, and 10 years were 92.9%, 80.8%, 71.7%, and 57.4%.
Prognostic analysis
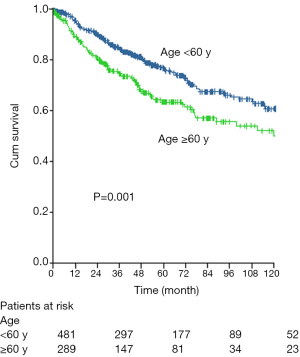
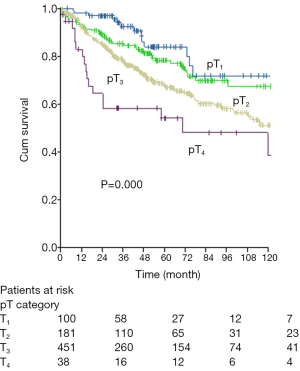
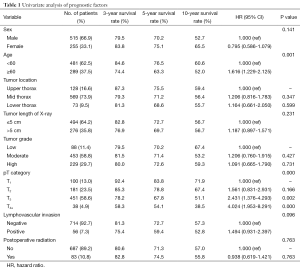
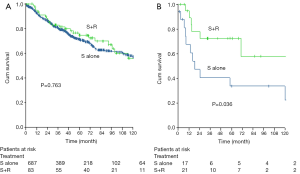
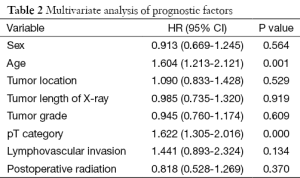
Age and pT staging were found closely correlated to prognosis by means of univariate analysis (Table 1). Five-year survival in cases younger and older than 60 were 76.5% vs. 63.3% (P=0.001, Figure 1), while those of pT1, pT2, pT3 and pT4a were 83.8%, 78.8%, 67.8% and 54.1% respectively (P=0.000, Figure 2). Five-year survival of groups of simple surgery and surgery plus postoperative radiotherapy were 71.3% and 74.5% respectively (P=0.763, Figure 3A), while further analysis indicated that postoperative radiotherapy was able to boost the survival of patient in pT4a which were 72.4% vs. 33.8% (P=0.036, Figure 3B). Multivariate analyses also proved that age and T staging were two independent factors on prognoses (Table 2).
Full table
Full table
Analyses of complications
The incidence of operative complication was 14.3% (98/687), including pneumonia 5.7% (39/687), trachyphonia 2.5% (17/687), anastomotic leakage 2.2% (15/687), severe cardiac complication (such as, acute heart attacks and serious heart rhythm disorders) 1.7% (12/687), incision infection 1.3% (9/687), hemorrhage of digestive tract 0.3% (2/687) and others 2.2% (15/687). Around 2% (14/687) died of operative complications, and 1.2% of them died within 30 postoperative days. Toxicities related to receipt of postoperative radiation, scored according to the RTOG/EORTC (1992) criteria (7,8). In our study, the incidence of acute complication was hematologic toxicity, neutropenia grade 2, 14.5% (12/83) and grade 3, 1.2% (1/83); grade 1-2 mucosal toxicity of esophagus 12.0% (10/83), grade 1-2 pulmonary toxicity 19.2% (16/83). And the incidence of late complication was: grade 5 pulmonary toxicity 1.2% (1/83), grade 5 cardiac toxicity (non-cancerous hydropericardium) 1.2% (1/83) and grade 5 upper digestive tract toxicity (thoracic stomach hemorrhage) 1.2% (1/83).
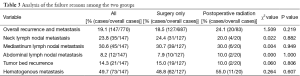
Analysis of the reasons for failure
Of the entire study patients, a total of 208 patients died: 180 in the surgery-only group and 28 in the postoperative radiation group. Among the surgery-only group, the cause of death in 49 cases was unknown, 106 died from cancer, and 25 died from other diseases. Among the postoperative radiation group, the cause of death in 9 cases was unknown, 16 died from cancer, and 3 died from other diseases. Five cases in the surgery-only group and three cases in the postoperative radiation group had a second primary tumor. The overall recurrence rate in our study was 19.1% (147/770). Among the cases with known cause of treatment failure, only one patient in the surgery-only group had lower mediastinal lymph node metastasis, and no lower mediastinal lymph node metastasis was found in the postoperative radiation group. Postoperative radiation did not affect local control rate or hematogenous metastasis rate. The specific failure reasons in the two groups are shown in Table 3. Further analysis showed that when compared to surgery alone, postoperative radiotherapy reduced the tumor bed recurrence rate of pT4a patients; in the surgery-only group, eight patients exhibited recurrence at the tumor bed, while there was only one such case in the postoperative radiotherapy group (P=0.005, Fisher’s exact test).
Full table
Discussion
It’s indicated in our study that both age and pT staging were significant and independent factors influencing the prognosis of patients at a stage of pT1-4aN0M0. Those with an advanced staging of pT and with an age more than 60 turned out with an unsatisfactory prognosis. Although it’s reported that postoperative radiotherapy made no significance in the survival rate, some further studies concluded that it could not only reduce the incidence of relapse in tumor bed but also boost the survival of those with a lesion longer than 5 cm and at a stage of T4a.
For pT1-4aN0M0 esophageal carcinoma patients after RO radical surgery, the number of negative lymph node was an import predictor. Bollschweiler et al. (9) reported that after RO radical surgery for esophageal carcinoma, the long-term survival rate in patients with >15 negative lymph nodes was significantly superior to that in patients with <15 negative lymph nodes (P<0.01). Greenstein et al. (10) reported that in postoperative esophageal carcinoma patients with negative metastatic lymph nodes, the age, pT stage, and the number of negative lymph node are independent predictors, while sex and postoperative radiotherapy showed no apparent association to prognosis (P>0.05). In this study, each patient has at least 15 negative lymph nodes (mean, 24.5; range, 15-68). Univariate and multivariate analysis showed that the age and pT staging are independent predictors. It’s also reported that cancer embolus was one of the most important factors influencing the prognosis. Lymphovascular invasion often result in lymph node metastases and distant metastasis after surgery (11-13), so patients with positive lymphovascular invasion often turn out a poor prognosis. Data from the present study indicate that 5-year survival of patients with or without cancer emboli were 59.4% or 72.7%, respectively (P=0.096). The statistical insignificance was considered due to the small number of samples.
The most important reason for postoperative failure with esophageal cancer is recurrence and metastasis. Patients with squamous cell carcinoma of the thoracic esophagus who had no lymph node metastasis and had undergone 3-field lymphadenectomy, the local-regional recurrence rate was 16.1-29% (11,12,14). Theoretically, prophylactic radiotherapy after resection of esophageal carcinoma could kill residual tumor cells, eradicate micro-metastases, decrease local recurrence, and increase survival. Several RCTs on the effect of postoperative radiotherapy on lymph node negative patients with esophageal cancer turned out with a negative result (15-17). And it’s the same with our study. The overall recurrence rate of patients in this study was 19.1% (147/770), which was consistent with previous reports (11,12,14). The 5-year survival rates in the surgery-only group and in the postoperative radiation group were 71.3% and 74.5%, respectively (P=0.763), suggesting that postoperative radiotherapy has no effect on survival rate. With further analysis showed that postoperative radiotherapy did somehow boost the survival of pT4a cases, with a 5-year survival of 72.4% vs. that of simple surgery 33.8% (P=0.036), Postoperative radiation also reduced the tumor bed recurrence of patients with pT4a tumors. the reason was thought to be that, with an obvious limitation that surgery could not remove all the infiltrating malignancy in paraesophageal loose connective tissue postoperative radiotherapy might probably become an indispensable redeem for surgery, eliminating the residual tumor cells and eradicating micro-metastases, so as to lower the incidence of local relapse and improve its postoperative survival. Fok et al. (18) reported that late complications of esophageal carcinoma in patients with postoperative radiation included radiation-induced pulmonary fibrosis, non-cancerous pericardial and pleural effusion and alimentary tract hemorrhage. While there were 3.6% (3/83) cases who died of late radiotherapeutic complications, which was considered as a result that the heart, lungs and thoracic-stomach all received some dosage of radiation. Due to small number size of samples and relevant statistical bias, the value of postoperative radiotherapy need to be further studied in other randomized clinical studies.
In conclusion, age and T staging were independent prognostic factors for patients with thoracic esophageal carcinoma staged pT1-4aN0M0 undergone esophagectomy with 3-field lymphadenectomy. Patients with high T staging and at an age more than 60 turned out bad prognoses, neither could postoperative radiotherapy improve their survival.
Acknowledgements
We are deeply indebted to Professor Guoliang Jiang, Department of Radiation Oncology, Fudan University Cancer Hospital, and Professor Xianglin Yuan from the Department of Cancer Medicine, Tongji Hospital, Tongji Medical School, Huazhong University of Technology for their guidance and suggestions in study design, data analyses, and manuscript preparation.
This research was supported in part by Fujian Provincial Foundation for Medical Innovation (2009-CXA-13) to K Zhu and X Chen.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Guo M, Zhao YD, Yang HJ, et al. Analysis of clinicopathological characteristics for 5406 cases of esophageal neoplasm. Chin J Cancer Prev Treat 2008;15:54-6.
- Chen J, Liu S, Pan J, et al. The pattern and prevalence of lymphatic spread in thoracic oesophageal squamous cell carcinoma. Eur J Cardiothorac Surg 2009;36:480-6. [PubMed]
- Ando N, Ozawa S, Kitagawa Y, et al. Improvement in the results of surgical treatment of advanced squamous esophageal carcinoma during 15 consecutive years. Ann Surg 2000;232:225-32. [PubMed]
- Akiyama H, Tsurumaru M, Udagawa H, et al. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 1994;220:364-72; discussion 372-3. [PubMed]
- Chen J, Pan J, Zheng X, et al. Number and location of positive nodes, postoperative radiotherapy, and survival after esophagectomy with three-field lymph node dissection for thoracic esophageal squamous cell carcinoma. Int J Radiat Oncol Biol Phys 2012;82:475-82. [PubMed]
- Shimada H, Okazumi S, Matsubara H, et al. Impact of the number and extent of positive lymph nodes in 200 patients with thoracic esophageal squamous cell carcinoma after three-field lymph node dissection. World J Surg 2006;30:1441-9. [PubMed]
- Chen J, Zhu J, Pan J, et al. Postoperative radiotherapy improved survival of poor prognostic squamous cell carcinoma esophagus. Ann Thorac Surg 2010;90:435-42. [PubMed]
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341-6. [PubMed]
- Bollschweiler E, Baldus SE, Schröder W, et al. Staging of esophageal carcinoma: length of tumor and number of involved regional lymph nodes. Are these independent prognostic factors? J Surg Oncol 2006;94:355-63. [PubMed]
- Greenstein AJ, Litle VR, Swanson SJ, et al. Effect of the number of lymph nodes sampled on postoperative survival of lymph node-negative esophageal cancer. Cancer 2008;112:1239-46. [PubMed]
- Bhansali MS, Fujita H, Kakegawa T, et al. Pattern of recurrence after extended radical esophagectomy with three-field lymph node dissection for squamous cell carcinoma in the thoracic esophagus. World J Surg 1997;21:275-81. [PubMed]
- Nakagawa S, Kanda T, Kosugi S, et al. Recurrence pattern of squamous cell carcinoma of the thoracic esophagus after extended radical esophagectomy with three-field lymphadenectomy. J Am Coll Surg 2004;198:205-11. [PubMed]
- Igaki H, Kato H, Tachimori Y, et al. Prognostic evaluation for squamous cell carcinomas of the lower thoracic esophagus treated with three-field lymph node dissection. Eur J Cardiothorac Surg 2001;19:887-93. [PubMed]
- Baba M, Aikou T, Yoshinaka H, et al. Long-term results of subtotal esophagectomy with three-field lymphadenectomy for carcinoma of the thoracic esophagus. Ann Surg 1994;219:310-6. [PubMed]
- Lu JC, Qian PD, Zha WW, et al. The meta-analysis of randomized controlled trial of prophylactic radiotherapy for esophageal carcinoma after curative resection. Journal of Evidence-Based Medicine 2005;5:167-71.
- Xiao ZF, Yang ZY, Liang J, et al. Value of radiotherapy after radical surgery for esophageal carcinoma: a report of 495 patients. Ann Thorac Surg 2003;75:331-6. [PubMed]
- Xiao ZF, Yang ZY, Miao YJ, et al. Influence of number of metastatic lymph nodes on survival of curative resected thoracic esophageal cancer patients and value of radiotherapy: report of 549 cases. Int J Radiat Oncol Biol Phys 2005;62:82-90. [PubMed]
- Fok M, Sham JS, Choy D, et al. Postoperative radiotherapy for carcinoma of the esophagus: a prospective, randomized controlled study. Surgery 1993;113:138-47. [PubMed]