Blocking the rectus sheath guided by ultrasound in an 8-year-old patient with cystic fibrosis: reporting a case
Introduction
Cystic fibrosis (CF) is a serious disease that is transmitted with an autosomal recessive inheritance pattern, and is the commonest disease among Caucasian populations (1/2,500) (1). There are many clinical manifestations that derive from its multiorgan dysfunctions, mainly in the respiratory and digestive tract. In addition, lung disease is principally responsible for morbidity and mortality in CF patients.
Blocking the rectus sheath, first described by Schleich in 1899 (2), is a loco-regional technique that provides adequate analgesia in those surgical procedures with midline or umbilical incisions (3-7). Nevertheless it has been scarcely used, mainly because of the precision required for needle placements, especially as far as the underlying peritoneal structures are concerned (3). The use of ultrasound scans to guide the anaesthetic technique has proven very useful to block the rectus sheath because rectus sheath layers are easily identified (4,5,7).
This article presents the case of an 8-year-old CF patient on the waiting list for a lung transplant (functional classification stage), who was scheduled for port-a-cath placement, and gastrostomy revision-cerclage.
Clinical case
An 8-year-old female patient, weighing 25 kg, 120 cm in height, with CF, was on the waiting list for a lung transplant and a percutaneous endoscopic gastrostomy for hyperprotein nutrition purposes, which required a port-a-cath being placed in the left vena femoralis, as well as gastrostomy revision-cerclage.
Three weeks before surgery, the patient’s respiratory failure became exacerbated, secondary to superinfection, so she had to be admitted to the paediatric intensive care unit (PICU) for 1 week with non-invasive bilevel positive airway pressure (BiPAP) ventilation.
One week before surgery, sedation was performed for central venous catheter placement on the right vena femoralis. During sedation, the patient manifested symptoms of desaturation, with a considerable number of secretions, which required instruments being placed in airways with a laryngeal mask airway (LMA) and positive pressure ventilation (PPV). She subsequently recovered spontaneous ventilation, but had to remain in the PICU for respiratory control purposes.
The patient was in a ward on the day of surgery, but was unable to remain in the dorsal decubitus position and needed to sit up, and a 40% fraction of inspired oxygen (FiO2) was administered via a face mask to maintain appropriate oxygen saturation (SaO2) levels.
Given the patient’s background, we decided to combine sedation, in order to maintain her spontaneous ventilation and to avoid handling airways, with a blocked rectus sheath as this would provide us with anaesthesia for the gastrostomy zone without deteriorating ventilation mechanics.
Anaesthetic management
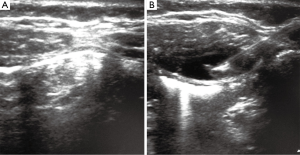
With the patient in a sitting position and with standard monitoring after premedication with 0.3 mg of atropine (0.01 mg·kg−1), the patient was sedated with midazolam intravenously (iv) in split doses to reach a total 3 mg dose. By maintaining the patient in a sitting position with an inclination of some 45º, bilateral blocking of the rectum sheath, guided by a gastrostomy ultrasound scan (T5-T6) (Figure 1), was carried out with a 22G Tuohy needle and by administering 10 mL of a mixture containing 2% Mepivacaine (20 mg·dL−1) and 0.25% Levobupivacaine (2.5 mg·dL−1). Anaesthesia was reinforced using an impeller beneath the skin around the gastrostomy with 4 mL of the same mixture.
At this time, sedation was supplemented with 1% Propofol perfusion at 10 mL/h and then surgery began. The patient remained calm at all times, her limbs did not move, and spontaneous ventilation was maintained with 40% FiO2 through a face mask, with SaO2 kept above 97% at all times. After 100 min of surgery, Propofol perfusion was withdrawn and the patient was fully conscious, collaborative, and was transferred back to the ward.
Discussion
The lung disease behind CF is responsible for more than 90% of morbidity and mortality in CF patients. The gradual affected state of the respiratory system determines respiratory failure, pulmonary hypertension, cor pulmonale and death. Pulmonary hypertension increases risk of death among CF patients who are on waiting lists for lung transplants, while clinically significant cor pulmonale occurs in end stages of CF with a mean survival rate of 8 months (1).
One common objective of anaesthesia in these patients is to cause as little ventilator depression as possible, and attempts are made to minimise airway handling so as to not increase pulmonary morbidity, and possible mortality. Therefore, anaesthetic treatment for these patients must be planned on an individual basis, and acquiring early tracheal extubation and avoiding both prolonged intubation and mechanical ventilation are of vital importance.
With this objective in mind, neuraxial or regional anaesthesia techniques can be beneficial in CF patients as they offer not only surgical anaesthesia, but also postoperative analgesia (1). In our case, the patient presented a poor functional class, was on a waiting list for a lung transplant, and was scheduled for a port-a-cath to be placed on the left vena femoralis and gastrostomy revision-cerclage. Given her clinical status and the type of surgery to be done, we considered performing regional anaesthesia and blocking the rectus sheath, guided by an ultrasound scan, to provide an excellent anaesthesia for surgery, a suitable postsurgical analgesia, and to maintain the patient’s spontaneous ventilation by avoiding handling of airways.
Blocking the rectus sheath has been demonstrated to be useful to provide analgesia while repairing umbilical and epigastric hernias, and for laparoscope-related surgery, pylorotomy and other minor midline incisions (3,4,6,7). It has also been reported to be a useful technique to treat chronic abdominal wall pain in paediatric patients (8). Although such blocking is relatively easy to carry out, performing the technique “blindly” by sensorial perceptions has always been a cause for concern about exact needle placement (3,4).
One of the most interesting technological advances recently made in regional anaesthesia in paediatric patients has been to introduce an anatomical ultrasound image to help locate the nerve. This is because regional anaesthesia techniques in children have always been considered a challenge due to the neural structures that pass close to critical structures (5,7,9).
While blocking the rectus sheath, proximity to the posterior sheath of the peritoneal cavity can easily lead to mislaying the needle inside the peritoneal cavity, which entails a risk of intraperitoneal injection and blocking failure, perforating the intestine (stomach or colon) or puncturing a mesenteric vessel (3,4,7). Furthermore, another author has described a retroperitoneal hematoma after blocking the rectus sheath (9).
Using ultrasound scans permits real-time non-invasive images of relevant anatomical structures and allows the needle to be placed at the same time thanks to direct viewing guidance. Thus a misplaced needle can be recognised and corrected immediately, which reduces the risk of failure and potential complications. Exact real-time image-guided needle placement means using smaller volumes of local anaesthetic without compromising the efficacy or success of the blocking technique. The advantages of performing blocking by an ultrasound guided technique, as opposed to blind techniques based on subtle sensations, which can go unnoticed even by experienced people, has also been demonstrated in the past. Therefore, ultrasound techniques offer considerable advantages over conventional techniques, based on reference points, for regional anaesthesia use in children (3-5,7,10).
Conclusions
Blocking rectus sheaths guided by ultrasound imaging has been demonstrated to be sufficiently effective for revision-cerclage gastrostomy surgery as it avoids the typical complications related to blocking and avoids the risks associated with general anaesthesia in CF patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors declare no conflicts of interest.
References
- Huffmyer JL, Littlewood KE, Nemergut EC. Perioperative management of the adult with cystic fibrosis. Anesth Analg 2009;109:1949-61. [PubMed]
- Schleich CL. Schmerzlose Operationen. Berlin: J Springer; 1899.
- Willschke H, Bösenberg A, Marhofer P, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia--a new approach to an old technique. Br J Anaesth 2006;97:244-9. [PubMed]
- Dolan J, Lucie P, Geary T, et al. The rectus sheath block: accuracy of local anesthetic placement by trainee anesthesiologists using loss of resistance or ultrasound guidance. Reg Anesth Pain Med 2009;34:247-50. [PubMed]
- Tsui B, Suresh S. Ultrasound imaging for regional anesthesia in infants, children, and adolescents: a review of current literature and its application in the practice of extremity and trunk blocks. Anesthesiology 2010;112:473-92. [PubMed]
- Isaac LA, McEwen J, Hayes JA, et al. A pilot study of the rectus sheath block for pain control after umbilical hernia repair. Paediatr Anaesth 2006;16:406-9. [PubMed]
- Willschke H, Marhofer P, Machata AM, et al. Current trends in paediatric regional anaesthesia. Anaesthesia 2010;65 Suppl 1:97-104. [PubMed]
- Skinner AV, Lauder GR. Rectus sheath block: successful use in the chronic pain management of pediatric abdominal wall pain. Paediatr Anaesth 2007;17:1203-11. [PubMed]
- Yuen PM, Ng PS. Retroperitoneal hematoma after a rectus sheath block. J Am Assoc Gynecol Laparosc 2004;11:448. [PubMed]
- Chin KJ, Chan V. Ultrasound-guided peripheral nerve blockade. Curr Opin Anaesthesiol 2008;21:624-31. [PubMed]


