Double segmentectomy for T4 lung cancer in a pulmonary-compromised patient
Introduction
Surgical treatment for lung cancer started in 1933 with the first successful pneumonectomy by Dr. Graham and continued to develop to the present day (1). In 1973, Dr. Jensik suggested that segmentectomy may be an adequate resection method for early-stage lung cancer in patients incapable of tolerating a standard lung resection (2). This suggestion has been widely debated for years and remains controversial.
Recently, more reports on the outcomes of patients who underwent anatomic segmentectomy for lung cancer, have been published. Segmentectomy is considered an alternative to lobectomy for tumors <2 cm in size (3). The method is a proven oncologic procedure for patients with significant morbidities and reduced cardiopulmonary reserve particularly. However, questions remain regarding safety, morbidity, mortality, and recurrence rate. We have performed anatomical segmentectomy with systematic nodal dissection as part of our commitment to provide surgical options to patients unfit for traditional lobectomy. In the present study, we report a case of a patient with limited respiratory reserve, who underwent double segmentectomy.
Case presentation
A 69-year-old man was referred to our pulmonology clinic with symptoms of dyspnea and chronic cough. He had a history of smoking approximately 50 pack/years. Clinical examination including osculation revealed decreased sounds on the left hemithorax. Blood test results were all in normal ranges. Chest X-ray demonstrated two distinct opacities in the left lung. Thorax computed tomography revealed a 2 cm × 2 cm lesion located in the apicoposterior segment of the left upper lobe and another 3 cm × 3 cm lesion in the superior segment of the left lower lobe (Figure 1). Preoperative bronchoscopic examination however did not yield a definitive diagnosis. Transthoracic fine needle aspiration biopsy of the lesion located in the left lower lobe indicated squamous cell carcinoma.
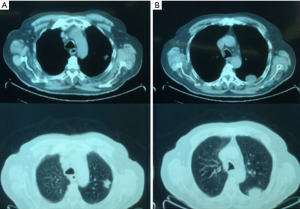
Positron emission tomography revealed two areas with 18F-fludeoxyglucose (18F-FDG) hyperintensity: one being 22 mm × 18 mm in size in the apicoposterior segment of left upper lobe [maximum standardized uptake value (SUVmax =13.6)] and the other being 36 mm × 21 mm in size in the superior segment of the left lower lobe (SUVmax =11.9) (Figure 1A,B). There was no observation of other high uptake areas suspicious for metastasis. Skeletal system and intracranial structures did not show any elevated FDG uptake either. Respiration function test results were as follows: forced vital capacity (FVC), 70%; and forced expiratory volume in 1 second (FEV1), 44%. Arterial blood gas analysis showed partial pressure of oxygen as 76 mmHg, partial pressure of carbon dioxide as 37.6 mmHg, and oxygen saturation as %95. Preoperative cardiopulmonary exercise testing for evaluation purposes was also performed in order to estimate operative risk. Maximum oxygen consumption during exercise (VO2max) value was 12.3 mL/kg/min; oxygen desaturation was not observed in 6-minute walk test with 420 m walked.
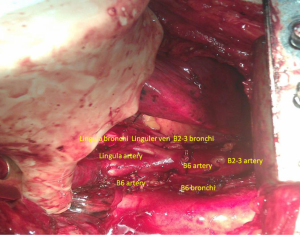
A left muscle-sparing thoracotomy was performed. On exploration, a 2 cm × 3 cm lesion in the left upper lobe and another 3 cm × 3 cm lesion in the lower lobe were detected. Histological analysis of frozen sections from a wedge resection of the preoperatively undiagnosed tumor revealed squamous cell carcinoma. Preresectional mediastinal lymph node dissection was performed. Histological analysis of the sampled mediastinal lymph nodes revealed no evidence of tumor. Poly-segmentectomy from different lobes was planned. The fissure was dissected, and anatomical segmentectomy of the left upper division and superior segment of the lower lob (B6 segment) was performed (Figure 2). The patient’s postoperative course was uneventful, and he was discharged on the fifth day after surgery. Definitive pathology result showed squamous cell carcinoma with no nodal involvement, and the tumor was classified as stage IIIB (T4N0M0) according to the seventh revision of the International Association for the Study of Lung Cancer Tumor-Node-Metastasis staging system for lung cancer.
Discussion
Our study suggested that preoperative pulmonary evaluation should be performed according to each patient’s specific characteristics and the type of surgery planned. All available guidelines recommend that when spirometry results predict postoperative FEV1 and diffusing capacity of the lung for carbon monoxide values are less than 40%, an exercise test should be performed to measure VO2max (4).
A VO2max between 10 to 15 mL/kg/min or a predicted postoperative VO2max of <10 mL/kg/min is usually considered contraindicative for surgery. Nevertheless, no single criterion should be used to exclude a patient from a curative surgery. Instead, the use of multiple preoperative studies is needed to select patients who are capable of tolerating and will benefit from pulmonary resection. Surgical intervention other than standard lobectomies or pneumonectomies can therefore be offered to selected high-risk patients. Experience from lung volume-reduction surgery has shown that some patients who would have been considered inoperable can safely undergo resection of lung cancer (5).
Harada et al. compared the outcomes of postoperative pulmonary function between segmentectomy and lobectomy in patients with stage I non-small cell lung cancer (NSCLC) and similar preoperative pulmonary function. Postoperative reductions of FVC and FEV1 were significantly lower in the segmentectomy group compared to those in the lobectomy group (6).
Anatomic segmentectomy can be an alternative to lobectomy for the protection of lung functions. Anatomically complete maximal parenchyma-saving resection can be performed in patients with limited respiration capacity. Removing a relatively large volume of healthy lung tissue could result in a poorer quality of postoperative life and a higher frequency of operative morbidity despite a reduced likelihood of having a second lung tumor resected.
The discussion on such a topic has been controversial with conflicting results in studies comparing lobectomy and sublobar resections. Many of those have included segmentectomy and wedge resection in the same group. Sublobar resection is usually performed for most patients with insufficient postoperative pulmonary reserve because they cannot tolerate a lobectomy. According to reports in recent years, segmentectomy in selected patients showed similar results to those of lobectomy (4-6). The selection criteria were tumor <2 cm in size, peripheral lesion location, and a 1 cm parenchymal surgical margin. However, questions remain regarding safety, morbidity, mortality, and recurrence rate with this method.
Kilic et al. compared the outcomes of 78 elderly patients (aged >75 years) with stage I NSCLC who underwent segmentectomy and lobectomy (7). The mortality rates were 1.3% for segmentectomy and 4.7% for lobectomy. Postoperative major complication rates were 11.5% for segmentectomy and 25.5% for lobectomy. These parenchyma-sparing methods also help increase the success of oncological treatment. The most undesirable and worst outcome of limited but adequate resection of lung cancer is local recurrence.
Multivariate analysis confirmed that recurrence rate and prognosis associated with sub-lobar resection were not inferior to those achieved with lobar resection, and overall survivals were similar in both groups. Local recurrence does not result in cancer-related death if it can be treated sufficiently (3).
Cancer and Leukemia Group B (CALGB 140503) has activated a phase III randomized trial investigating lobectomy versus sub-lobar resection for <2 cm, peripheral, node-negative, non-small cell lung cancer. A multi-institutional trial was also in the planning phase by the Japan Clinical Oncology Group (JCOG0802). The trial will similarly randomize patients with <2 cm peripheral NSCLC to the lobectomy or segmentectomy group. Future results from the randomized phase III limited resection trials CALGB and JCOG0802 for peripheral <2 cm NSCLC will hopefully clarify the role of sub-lobar resection as an alternative to lobectomy (8). Standard surgical resection for lung cancer is constantly evolving. Segmentectomy could be a reasonable treatment option in selected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Graham EA, Singer JJ. Successful removal of the entire lung for carcinoma of the bronchus. JAMA 1933;101:1371. [PubMed]
- Jensik RJ, Faber LP, Milloy FJ, et al. Segmental resection for lung cancer a fifteen year experience. J Thorac Cardiovasc Surg 1973;66:563-72. [PubMed]
- Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [PubMed]
- Colice GL, Shafazand S, Griffin JP, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest 2007;132:161-77.
- Zahid I, Sharif S, Routledge T, et al. Is lung volume reduction surgery effective in the treatment of advanced emphysema? Interact Cardiovasc Thorac Surg 2011;12:480-6. [PubMed]
- Harada H, Okada M, Sakamoto T, et al. Functional advantage after radical segmentectomy versus lobectomy for lung cancer. Ann Thorac Surg 2005;80:2041-5. [PubMed]
- Kilic A, Schuchert MJ, Pettiford BL, et al. Anatomic segmentectomy for stage I non-small cell lung cancer in the elderly. Ann Thorac Surg 2009;87:1662-6; discussion 1667-8.
- Stiles BM, Altorki NK. Segmentectomy Versus Lobectomy for Stage I Lung Cancer in Patients with Good Pulmonary Function. In: Ferguson MK, editor. Difficult Decisions in Thoracic Surgery. New York, NY: Springer, 2007:125-33.


