Evolution of trochlear compartment geometry in total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is a successful procedure, with over 560,000 operations performed annually in Europe (1) and over 600,000 in the United States (2). Due to the ageing population, the number of TKA procedures is expected to rise almost four times by 2030 (3). Despite its success, a large proportion of patients experience pain and dissatisfaction after TKA, where patellofemoral pain and instability remain among the most common reasons for revision (4).
Anterior knee pain following TKA is observed equally in knees with resurfaced and non-resurfaced patellae (5-7), thus it is unlikely that pain is caused by arthritis of the patellar cartilage. Although the exact mechanism remains unclear, abnormal patellofemoral joint loads or kinematics caused by patellar malalignment, and over- and under-stuffing appear to play important roles in the development of anterior knee pain (8-10). Patellar instability is a frequent complication after TKA that could lead to dislocation (5.8 per 100,000), which is of particular concern in young females (33 per 100,000) (11). It is caused by a variety of genetic, congenital, or sport-related factors (4,12): anatomic deformities, ligament malalignment, and neuromuscular activation.
Patellofemoral complications are usually caused by multiple factors related to surgical technique (e.g., implant positioning and sizing, soft-tissue balancing, patellar resurfacing, etc.) and implant design (e.g., trochlear depth, sagittal curvature, patellar component shape) (13-15). Numerous biomechanical studies suggest that even if the surgical technique is optimized, patellofemoral tracking is not always restored to physiological values, because the prosthetic trochlea may differ from the native trochlea, implying that complications may be due to implant design (14-17).
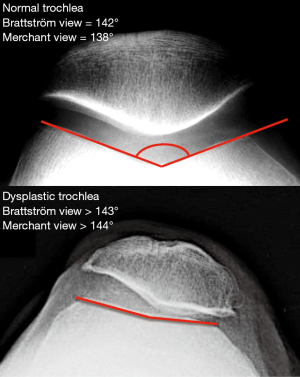
In 2010, the authors compared trochlear geometry in 14 TKA designs and found that most models exhibit characteristics of trochlear dysplasia (18). In a later study the authors found similar anomalies in patellofemoral arthroplasty (PFA) components (19). The principal parameter compared was the sulcus angle, a non-dimensional indicator often used to quantify the extent of trochlea dysplasia on skyline radiographs (Figure 1). The mean sulcus angle in normal knees is 138° in the ‘Merchant view’ at 45° of flexion (20,21), and 142° in the ‘Brattström view’ at 30° of flexion (22). The sulcus angle in knees with trochlear dysplasia is generally above 144° in the ‘Merchant view’ (23) or above 143° in the ‘Brattström view’ (24). In cases with severe patellofemoral disorders, such anatomic deformities can be addressed surgically by extensor mechanism realignment, trochleoplasty or tibial tuberosity osteotomy; and in the presence of arthritis, by partial or total arthroplasty (25-29).
The aim of the present study was to provide an updated analysis of trochlear geometry in more recent TKA models available globally, and to determine whether they feature improvements compared to their predecessors. The hypothesis was that recent TKA models have more anatomic trochlear compartments and would display no signs of trochlear dysplasia. Because patellofemoral complications are usually caused by multiple factors related to surgical technique and implant design, the authors did not attempt to correlate the findings with clinical results of the studied implants.
Material and methods
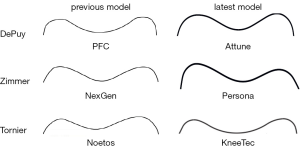
This is a descriptive study of the 6 following TKA femoral components: PFC and Attune (DePuy Orthopaedics Inc., Warsaw, IN, USA), NexGen and Persona (Zimmer Inc., Warsaw, IN, USA), HLS Noetos and KneeTec (Tornier SA, Montbonnot, France). Specimens were chosen from the middle of the available size range.
The specimens were each scanned using a three-dimensional (3D) optical scanning machine (ATOS II, GOM mbH, Braunschweig, Germany) and its photogrammetric analysis software (TRITOP, GOM mbH, Braunschweig, Germany). The system has measurement resolution of 0.05 mm and overall accuracy of ±0.01 mm. The coordinates of points scanned on each specimen were rendered into smooth surfaces using 3D model reconstruction software (Rapid Form, 3D Systems Corp., SC, USA), which enabled full manipulation and measurement using computer aided design software (Pro/Engineer, Parametric Technology Corporation, MA, USA).
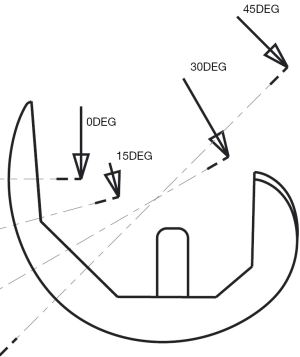
The specimens were each oriented in a consistent coordinate system, with the origin defined as the intersection between the flexion-extension axis (centre of the cylinder that best fits the distal condyles) and the midpoint of the intercondylar notch. The authors plotted the trochlear profiles of the specimens at different flexion angles following a previously published protocol (18). Each specimen was virtually rotated about its flexion-extension axis using Pro/Engineer by the following angles: 0°, 15°, 30° and 45°. At each flexion angle, the most anterior point on the trochlea was marked and the mediolateral trochlear profile at that level was digitized (Figure 2).
All recorded coordinates were exported to spreadsheets using Microsoft® Excel (Microsoft Corp, Redmond, WA). To enable consistent geometric comparisons between all specimens, the coordinates of right-sided implants were mirrored to become super-imposable with those of left-sided implants. The two-dimensional ML profiles of each prosthetic trochlea could therefore be superposed and compared with its origin at the intersection of (I) the midpoint between the medial and lateral margin of each specimen and (II) the trochlear groove, or deepest point on the sulcus, of each profile. The ‘sulcus angle’ of each profile was calculated from the coordinates of the trochlear groove and those of the highest points of the medial and lateral facets.
As this study did not involve human nor animal data, institutional review board (IRB) was not required, and statistical analysis was not performed.
Results
The sulcus angles of all implants were compared (Table 1) and the trochlear profiles at 30° of flexion were presented visually in a non-dimensional coordinate system (Figure 3). Analysis of sulcus angles reveals general convergence of designs to anatomic values.
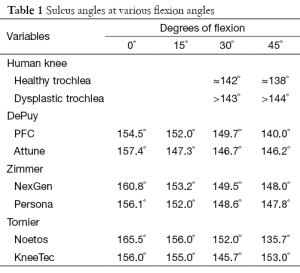
Full table
At 0° of flexion, sulcus angles of recent implant models lie within the narrow range of 156.0° to 157.4°, while those of previous generation models are spread across a wide range of 154.5° to 165.5°. Comparison of DePuy implants revealed that the more recent Attune model has a trochlea 3° shallower than that of the earlier PFC model. By contrast, the Zimmer and Tornier implants revealed that the more recent Persona and KneeTec respectively have trochlea 4.7° and 9.5° deeper than those of the earlier NexGen and Noetos models.
At 30° of flexion, sulcus angles of recent implant models also lie within a limited range of 145.7° to 148.6°, but those of previous generation models are within a similar range of 149.5° to 152.0°. All three manufacturers have deepened their trochlea at 30° of flexion in the more recent models compared to earlier designs. While the sulcus angles converge towards anatomic values, they remain 3° to 6° shallower than average values reported for healthy knees.
At 45° of flexion, the sulcus angles of recent models vary within the range of 146.2° to 153.0°, and those of previous generation models are equally spread from 135.7° to 148.0°. Both DePuy and Tornier have reduced the depth of the trochlea in their recent models compared to previous models, whereas the trochlea of Zimmer implants remained unchanged at that level. It is worth noting that sulcus angle measurements at 45° of flexion in TKA models are inconsistent due to the presence of an intercondylar notch or a post-cam mechanism.
Discussion
The principal finding of this study was that recent TKA designs have more anatomic trochlear geometries than earlier TKA models by the same manufacturers. The sulcus angles remain 3° to 6° greater (shallower) in prosthetic trochlear compartments than in healthy knees, and they exceed radiologic signs of trochlear dysplasia by 2° to 5°. The hypothesis that recent TKA models display no signs of trochlear dysplasia is therefore refuted.
In a previous study of 14 TKA designs, the authors reported that 11 models had sulcus angles that exceeded radiographic indicators of trochlear dysplasia, and that in most models the discrepancy was over 10°. The sulcus angle is inversely proportional to the depth of the trochlear groove, which is important to engage the patella in the trochlea, especially in early flexion (0° to 30°) (29-31). The average sulcus angle for healthy knees is 138° in the ‘Merchant view’ (20,21,32), and 142° in the ‘Brattström view’ (22). A high sulcus angle indicates a shallow or dysplastic trochleae, observed in the majority of patients suffering from patellofemoral disorders (33). On the other hand, a normal sulcus angle does not exclude the presence of trochlear dysplasia, since sulcus angle may be high proximally and decrease distally to normal values (34-36).
The design of the femoral component is of great importance to grant normal kinematics and inappropriate trochlear groove geometry could induce patellofemoral complications following TKA (37). In the past, the inability of implant manufacturers to replicate normal trochlear anatomy was attributed to lack of anatomic data from healthy trochlear grooves (15,30,31), but numerous morphometric studies were published in recent years to help prevent such discrepancies between normal and prosthetic anatomy (16,18,19,31,38-48).
Trochlear components with high sulcus angles require a specific and adapted surgical technique including ligament balancing and extensor mechanism realignment according to the TT-TG value to prevent any further patellar maltracking in early flexion. If the patella is resurfaced, the shape of the patellar button could influence patellofemoral tracking and stability, but this aspect was not considered in the present analysis as all models included can be implanted without patellar resurfacing.
The authors recently studied how the in-vivo position of the patella in mid-flexion can be influenced by design enhancements to the trochlear compartment and patellar button in the HLS KneeTec compared to its predecessor the HLS Noetos (38). While the tibiofemoral kinematics were nearly identical for both implant studied, the patellar flexion angle was significantly using the KneeTec component (23.5°±8.7°) than using the Noetos component (6.3°±7.3°). Since the same surgical technique and implant alignment were used for both implant models, it is likely that the differences in post-operative patellar position are related to the differences in trochlear geometry and patellar design between the two implant models. The authors noted that the ‘cone-shaped’ button of the Noetos tilts until equilibrium is reached, whereas the ‘dome-shaped’ button of the KneeTec resists tilt by virtue of its large-radius spherical surface (49).
The strengths of this study were the ability to directly compare current and preceding TKA models by the same manufacturers to assess the evolution of trochlear geometry in the light of published morphometric studies and kinematic investigations on the patellofemoral joint. The measurement techniques were consistent and reproducible. In addition, the ‘scale factor’ was minimized by studying specimens from the middle of the size range and by referring to a non-dimensional variable of sulcus angle. The main weaknesses of the study were the consideration of the trochlear component and not the patellar component, and the focus on static design features rather than dynamic implant performance.
Conclusions
The present study reveals that recent TKA designs have more anatomic trochlear geometries than earlier TKA models by the same manufacturers, but the trochlear compartments still exceed radiologic signs of trochlear dysplasia by 2° to 5°. The clinical relevance of this descriptive study is that surgeons should be aware of such design limitations in order to improve their choice of implants for specific patients, and to improve diagnosis and treatment of post-operative patellofemoral complications. The authors stress the importance of assessing patellar tracking intra-operatively to ensure that the extensor mechanisms is optimally adjusted and that the implant configuration grants adequate patellar stability particularly in early flexion.
Acknowledgements
The authors are grateful to Eric Faure and Eric Renault (Tornier SA, Montbonnot, France) for their support in scanning and modelling the specimens studied.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Eucomed Orthopaedic Committee. Implant Data Collection Report. 2012. Available online: http://archive.eucomed.org/newsroom/101/104/Orthopaedic-devices-increase-quality-of-life-at-good-value-for-money
- Losina E, Thornhill TS, Rome BN, et al. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 2012;94:201-7. [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA 2013.
- Lygre SH, Espehaug B, Havelin LI, et al. Does patella resurfacing really matter? Pain and function in 972 patients after primary total knee arthroplasty. Acta Orthop 2010;81:99-107. [PubMed]
- Nizard RS, Biau D, Porcher R, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res 2005.196-203. [PubMed]
- Pilling RW, Moulder E, Allgar V, et al. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am 2012;94:2270-8. [PubMed]
- Brown EC 3rd, Clarke HD, Scuderi GR. The painful total knee arthroplasty: diagnosis and management. Orthopedics 2006;29:129-36. [PubMed]
- Petersen W, Rembitzki IV, Brüggemann GP, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 2014;38:319-28. [PubMed]
- van Jonbergen HP, Reuver JM, Mutsaerts EL, et al. Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc 2014;22:478-99. [PubMed]
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [PubMed]
- Ntagiopoulos PG, Bonin N, Sonnery-Cottet B, et al. The incidence of trochlear dysplasia in anterior cruciate ligament tears. Int Orthop 2014;38:1269-75. [PubMed]
- Healy WL, Wasilewski SA, Takei R, et al. Patellofemoral complications following total knee arthroplasty. Correlation with implant design and patient risk factors. J Arthroplasty 1995;10:197-201. [PubMed]
- Ostermeier S, Buhrmester O, Hurschler C, et al. Dynamic in vitro measurement of patellar movement after total knee arthroplasty: an in vitro study. BMC Musculoskelet Disord 2005;6:30. [PubMed]
- Varadarajan KM, Rubash HE, Li G. Are current total knee arthroplasty implants designed to restore normal trochlear groove anatomy? J Arthroplasty 2011;26:274-81. [PubMed]
- Varadarajan KM, Freiberg AA, Gill TJ, et al. Relationship between three-dimensional geometry of the trochlear groove and in vivo patellar tracking during weight-bearing knee flexion. J Biomech Eng 2010;132:061008. [PubMed]
- Anouchi YS, Whiteside LA, Kaiser AD, et al. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 1993.170-7. [PubMed]
- Dejour D, Ntagiopoulos PG, Saffarini M. Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2599-607. [PubMed]
- Saffarini M, Ntagiopoulos PG, Demey G, et al. Evidence of trochlear dysplasia in patellofemoral arthroplasty designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2574-81. [PubMed]
- Merchant AC. Femoral sulcus angle measurements. Am J Orthop (Belle Mead NJ) 1997;26:820, 822.
- Mulligan ME, Jones ED Jr. Femoral sulcus angle measurements. Am J Orthop (Belle Mead NJ) 1997;26:541-3. [PubMed]
- Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella. a clinical and x-ray-anatomical investigation. Acta Orthop Scand Suppl 1964;68 SUPPL 68:1-148. [PubMed]
- Tecklenburg K, Dejour D, Hoser C, et al. Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 2006;14:235-40. [PubMed]
- Davies AP, Costa ML, Shepstone L, et al. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br 2000;82:1162-6. [PubMed]
- Patel J, Ries MD, Bozic KJ. Extensor mechanism complications after total knee arthroplasty. Instr Course Lect 2008;57:283-94. [PubMed]
- Grelsamer RP. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br 2001;83:772-3. [PubMed]
- Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop 2010;34:311-6. [PubMed]
- Arendt E. Anatomy and malalignment of the patellofemoral joint: its relation to patellofemoral arthrosis. Clin Orthop Relat Res 2005.71-5. [PubMed]
- Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med 2007;35:484-92. [PubMed]
- Barink M, Meijerink H, Verdonschot N, et al. Asymmetrical total knee arthroplasty does not improve patella tracking: a study without patella resurfacing. Knee Surg Sports Traumatol Arthrosc 2007;15:184-91. [PubMed]
- Meijerink HJ, Barink M, van Loon CJ, et al. The trochlea is medialized by total knee arthroplasty: an intraoperative assessment in 61 patients. Acta Orthop 2007;78:123-7. [PubMed]
- Merchant AC, Mercer RL, Jacobsen RH, et al. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 1974;56:1391-6. [PubMed]
- Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [PubMed]
- Fucentese SF, Schöttle PB, Pfirrmann CW, et al. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 2007;15:168-74. [PubMed]
- Martinez S, Korobkin M, Fondren FB, et al. Computed tomography of the normal patellofemoral joint. Invest Radiol 1983;18:249-53. [PubMed]
- Shih YF, Bull AM, Amis AA. The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc 2004;12:300-6. [PubMed]
- Kulkarni SK, Freeman MA, Poal-Manresa JC, et al. The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? J Arthroplasty 2000;15:424-9. [PubMed]
- Saffarini M, Zaffagnini S, Bignozzi S, et al. Does patellofemoral geometry in TKA affect patellar position in mid-flexion? Knee Surg Sports Traumatol Arthrosc 2015;23:1799-807. [PubMed]
- Ntagiopoulos PG, Dejour D. Current concepts on trochleoplasty procedures for the surgical treatment of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 2014;22:2531-9. [PubMed]
- Zaffagnini S, Dejour D, Grassi A, et al. Patellofemoral anatomy and biomechanics: current concepts. Joints 2013;1:15-20. [PubMed]
- Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575-81. [PubMed]
- Kamath AF, Slattery TR, Levack AE, et al. Trochlear inclination angles in normal and dysplastic knees. J Arthroplasty 2013;28:214-9. [PubMed]
- Guilbert S, Chassaing V, Radier C, et al. Axial MRI index of patellar engagement: a new method to assess patellar instability. Orthop Traumatol Surg Res 2013;99:S399-405. [PubMed]
- Dejour D, Ferrua P, Ntagiopoulos PG, et al. The introduction of a new MRI index to evaluate sagittal patellofemoral engagement. Orthop Traumatol Surg Res 2013;99:S391-8. [PubMed]
- Panni AS, Cerciello S, Maffulli N, et al. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 2011;19:663-70. [PubMed]
- Iranpour F, Merican AM, Dandachli W, et al. The geometry of the trochlear groove. Clin Orthop Relat Res 2010;468:782-8. [PubMed]
- Varadarajan KM, Gill TJ, Freiberg AA, et al. Gender differences in trochlear groove orientation and rotational kinematics of human knees. J Orthop Res 2009;27:871-8. [PubMed]
- Ma HM, Lu YC, Kwok TG, et al. The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Joint Surg Br 2007;89:408-12. [PubMed]
- Becker R, Karlsson J. The importance of the third knee compartment on outcome following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:475-7. [PubMed]