Thoracoscopic left mediastinal lymph node dissection
Introduction
In Japan, the use of thoracic surgery for lung cancer is constantly increasing. Moreover, the frequency of video-assisted thoracoscopic surgery (VATS) for lung cancer is also increasing. A nationwide survey in 2012 revealed that about 65% of the operations for lung cancer were performed using VATS, and among them, 50% were performed using only thoracoscopic vision (1,2). However, it is controversial whether mediastinal lymph node dissection can be performed as effectively using VATS as using the open thoracotomy approach (3,4). Herein, I report some techniques for subcarinal lymph node dissection from the left thoracic cavity and left upper mediastinal lymph node dissection using VATS.
Operative techniques
At our institution, VATS is usually performed with one utility incision and three ports. The surgeon is positioned on the right side of the patient. The scopist and assistant are positioned on the opposite side. The surgeon uses a 7-mm port at the level of the 4th intercostal space and an approximately 3-cm utility incision at the level of the 6th intercostal space. The camera scope, which is a 30° endoscope, is inserted from the port positioned at the 5th intercostal space, and an assistant provides help using one or two devices from the port positioned at the level of the 7th intercostal space. Two monitors are used. On the operator’s monitor, the cranial side is on the left. On the assistant’s monitor, the image is rotated upside down, so that the cranial side is on the right.
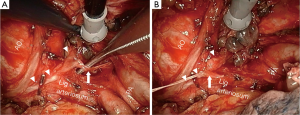
Knacks for subcarinal lymph node dissection from left thoracic cavity (Figure 1)
When approaching the subcarinal lymph nodes from the left thoracic cavity, it is difficult to secure the view of the right lower portion. To address this problem, the lower lobe bronchus is encircled with cotton tapes for the assistant doctors to pull it to the ventral and cranial sides before the division of the inferior pulmonary vein. This results in not only the bronchus but also the inferior pulmonary vein and pericardium being simultaneously retracted towards the front. As a result, this technique provides a better view of the right lower portion of the subcarinal lymph node.
Moreover, the order of dissection is also important. If the lymph node is separated from the left main bronchus first, it will fall down and interrupt the right-side view. Therefore, it is imperative to start the separation from the right main bronchus, and then proceed to the left.
Knack for left upper mediastinal lymph node dissection (Figure 2)

It is difficult to dissect lymph nodes at level 4L from the recurrent laryngeal nerve without incurring the risk of paralysis. To address this problem, I ligate and transect the thoracic cardiac branch from the recurrent laryngeal nerve, and retract it by using a suture (Figure 3). I pull the thread out through the port on my left, grasp it using a mosquito pean, and drop it naturally. Then, tension is applied to the recurrent laryngeal nerve to visualize the bottom of the lymph nodes at level 4L, and make it easy to dissect the periphery of the nerve safely.
In anatomy, the recurrent nerve has a few branches. If these are found, it is more effective to retract a deeper branch.
From about 30 cases in my experience, I have not observed any incidence of recurrent nerve paralysis using this procedure.
Comments
VATS was started about 20 years ago, and since then, it has undergone improvements by many surgeons. Yamashita et al. showed that VATS lobectomy by an experienced surgeon is associated with minimal invasiveness and an outcome equivalent to that of open lobectomy (7). On the other hand, Subroto et al. showed that robotic surgery is associated with a higher rate of intraoperative injury and bleeding than thoracoscopic surgery (8). Therefore, it is currently believed that thoracoscopic surgery is a well-balanced procedure because of its quality, minimal invasiveness, and safety. However, in order to achieve surgical outcomes by VATS that are comparable to those of open surgery in terms of quality and safety, by not only specialists but also any general thoracic surgeon, development of better surgical methods is warranted.
Acknowledgements
This manuscript was presented at the 5th Xizi Annual Forum of Thoracic Oncology.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery, Masuda M, et al. Thoracic and cardiovascular surgery in Japan during 2012: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2014;62:734-64. [PubMed]
- Kitano M, Yamashita Y, Shiraishi N, et al. 12th Nationwide Survey of Endoscopic Surgery in Japan. J Jpn Soc Endosc Surg 2014;19:495-640.
- Palade E, Passlick B, Osei-Agyemang T, et al. Video-assisted vs open mediastinal lymphadenectomy for Stage I non-small-cell lung cancer: results of a prospective randomized trial. Eur J Cardiothorac Surg 2013;44:244-9. [PubMed]
- Merritt RE, Hoang CD, Shrager JB. Lymph node evaluation achieved by open lobectomy compared with thoracoscopic lobectomy for N0 lung cancer. Ann Thorac Surg 2013;96:1171-7. [PubMed]
- Nagashima T. Knacks for subcarinal lymph node dissection from left thoracic cavity. Asvide 2016;3:011. Available online: http://www.asvide.com/articles/762
- Nagashima T. Knacks for left upper mediastinal lymph node dissection. Asvide 2016;3:012. Available online: http://www.asvide.com/articles/763
- Yamashita S, Goto T, Mori T, et al. Video-assisted thoracic surgery for lung cancer: republication of a systematic review and a proposal by the guidelines committee of the Japanese Association for Chest Surgery 2014. Gen Thorac Cardiovasc Surg 2014;62:701-5. [PubMed]
- Paul S, Jalbert J, Isaacs AJ, et al. Comparative effectiveness of robotic-assisted vs thoracoscopic lobectomy. Chest 2014;146:1505-12. [PubMed]


