
Efficacy of extracorporeal shock waves in the treatment of myofascial pain syndrome: a systematic review and meta-analysis of controlled clinical studies
Introduction
Myofascial pain syndrome (MPS), a musculoskeletal system disease, is a recurrent local myofascial pain characterized by the appearance of myofascial trigger points (MTrPs) (1). MTrPs are palpable nodules in the fibrous bands of skeletal muscle and are characterized by painful irritability, and direct or indirect stimulation of MTrPs causes intense referred pain, neuroelectrical activity, and convulsive responses, which can even lead to joint limitation and loss of mobility (2). Although myofascial pain can involve a wide range of pain points up and down the body; neck, shoulder, and back pain is the most common in clinical practice, and the degree of pain is the most significant (3). A study (4) has shown that sedentary, excessive mental stress and long-term poor posture can all cause muscle strain, resulting in the formation of neck, shoulder, and back myofascial lesions, directly affecting the nerve endings and producing pain. The treatment modalities for MPS include trigger point injection (TPI), transcutaneous electrical nerve stimulation (TENS), ultrasound (US), and other modalities. In recent years, extracorporeal shock wave therapy (ESWT) as a type of physical therapy has been applied in the treatment of MPS. Shock waves are high-energy mechanical waves. ESWT uses the principle of shock wave to transmit energy to the deep tissue of musculoskeletal tissue, so as to carry out pathological reversal of human muscle, bone, internal organs and other tissue lesions, and achieve the purpose of treatment. In the practice of rehabilitation medicine, ESWT is mainly used in ischemic femoral head necrosis, delayed fracture healing and various chronic pain (5). At present, many controlled clinical studies have shown the effectiveness of ESWT therapy for the treatment of MPS, but there are very few systematic reviews on this aspect. The study by Yoo et al. (6) included five controlled clinical studies for meta-analysis. However, this study was limited to patients with pain sites in the trapezius muscle, and the number of included studies was too small. The study by Jun et al. (7) included 11 articles but included observational studies, so the level of evidence of the results was not high. This study included more high-quality controlled clinical studies and analyzed whether ESWT is more effective than other treatment modalities.
We present the following article in accordance with the PRISMA reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-295/rc).
Methods
Literature search strategy
The following databases were searched by computer: PubMed, Embase, Cochrane Central Register of Controlled Trials, and Web of Science for clinical studies from database establishment to October 2021, and we limited the English literature. The keyword phrases used in the search were “ESWT”, “extracorporeal shock wave”, “MPS”, and “myofascial pain syndrome”.
Inclusion of studies
We developed inclusion criteria according to the PICOS (Patients, Intervention, Control, Outcome, Study type) principle, which aims to solve this problem: “Is the treatment of ESWT more advantageous than other intervention methods?”: (I) study subjects: all study subjects were patients with MPS, we do not limit gender, we do not limit the site of pain onset, neck, shoulder, lower back, and femoral pain patients were included in the study; (II) intervention group method: the study included a group treated with ESWT, and the ESWT adopted in each study may be different, in respect of energy density and total treatment time. Simple limb movements can be used during ESWT treatment, but the movement is only to be used with ESWT, not a stand-alone treatment; we exclude combined treatment; (III) control group method: a control group must be included in the study, and its intervention method is Sham ESWT, or one or more of nerve electrical stimulation therapy, drug injection therapy, ultrasonic therapy; (IV) efficacy determination: we take the degree of pain after treatment, pain threshold when pressed, disability index as the main efficacy indicators. To avoid severe heterogeneity, the Visual Analog Scale (VAS) method was used to determine the degree of pain after treatment, excluding the degree of pain assessed by other methods, such as Rating Scales and Verbal Scales (8). We selected the data after the end of treatment or 1 week after the end of treatment as the analysis, and the data during treatment will not be included in the analysis. (V) Study types: we only included controlled trials, and we preferred to include randomized controlled trials but also included controlled clinical trials or quasi-randomized studies. We did not include controlled studies at different periods, and we did not limit the randomization method, allocation concealment, or blinding method adopted by the study, but we would assess the quality of the study before analysis.
Literature selection and data extraction
All the retrieved literature in the database was stored in files with the suffix name “enw” or “txt” and managed uniformly by the import function of Endnote X9 software. After the repeated studies were automatically removed by the software, we read the titles and abstracts of the articles for screening. After the unqualified literature was removed, the remaining literature was obtained in full text and screened continuously until qualified literature was obtained. This work was independently completed by two researchers. To solve differences between the two reviewers, a third reviewer was introduced to participate in the discussion.
Data extraction was independently performed by the two researchers using Excel sheets, which were cross-checked after completion. The extracted contents included: (I) basic data of the literature: name of the first author, publication time and publication; (II) characteristics of the study subjects: sample size, gender ratio, average age, location of pain, diagnosis of the disease, and duration (course of the disease); (III) literature intervention methods: specific measures for the intervention group and the control group; (IV) outcome data: drop-out cases, outcome data. In the process of data extraction, if no specific data were provided in the literature, the data were obtained according to the address specified in the literature. If the data could not be obtained, the original author of the literature was contacted to obtain the data; if the data could not be obtained, the literature was excluded.
Literature quality
We used the PEDro scale (9) to evaluate the included randomized control trial (RCT) studies, which contained 11 evaluation criteria, with 1 point for each item and a total score of 11 points.
Risk of bias, heterogeneity survey, and sensitivity analysis
The risk of bias assessment tool provided in RevMan 5.4 was used for analysis. The risk assessment was performed for each study from six aspects: randomization, allocation concealment, quality of blinding, outcome assessment, incomplete data, selective reporting, and other bias. The source of heterogeneity was judged by subgroup analysis and exclusion, and if the source could not be identified, general descriptive analysis was used. Sensitivity analysis was performed by comparing the results of the fixed-effect model with those of the random-effect model.
Statistical methods
Heterogeneity analysis: the heterogeneity among different studies was analyzed using the I2 test and Q test. The heterogeneity was not statistically significant, as indicated by I2<50% or P≥0.1, which means there was no (or acceptable) heterogeneity among the studies. Effect size: MD (mean difference) effect size was used for continuous variables. The 95% CI was used as the confidence interval, and P<0.05 was considered statistically significant. Effect model selection: if heterogeneity analysis showed no heterogeneity between literatures, a fixed effect model was used; if heterogeneity existed, a random effect model was used; analysis tools and result presentation: Revman 5.4 software provided by Cochrane was used as analysis tool in this study, and the analysis results were presented in the form of forest plot; publication bias analysis: publication bias was reported in funnel plot.
Results
Literature screening results
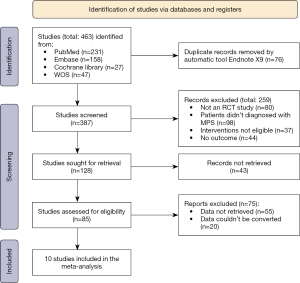
In this study, 463 literatures were initially identified, 76 repeated literatures were automatically removed using Endnote X9 tool, 259 literatures that did not meet the criteria were screened and excluded, 43 literatures that could not obtain the full text were excluded, 75 literatures that did not meet the requirements were excluded after reading the full text, and 10 literatures (10-19) were finally included. The selection flow chart is shown in Figure 1. Study (20) used a combination modality and was excluded; study (21) included cases with non-MPS and was excluded (others had much excluded literature data and we do not list all of them here).
Basic characteristics of literatures
A total of 571 patients were included in this study, of which 541 patients had MPS pain at the neck and upper back, and only 30 patients had pain at the waist, as shown in Table 1.
Table 1
| Author | Year of publication | Pain site | Mean age (years) | Population (E/C) | Experimental group | Control group | Follow-up time | Outcome indicators | PEDro Score |
|---|---|---|---|---|---|---|---|---|---|
| Jeon et al. (10) | 2012 | Neck and upper back | 45.00±15.46 | 15/15 | ESWT | TPI + TENS | 4 weeks | PPT/VAS/PRS/MPQ | 8 |
| Hong et al. (11) | 2017 | Lumborum | 55.46±15.09 | 15/15 | ESWT | TPI | 4 weeks | PPT/ODI/RM/QBS | 7 |
| Aktürk et al. (12) | 2018 | Neck and upper back | 33.45±8.02 | 20/20 | ESWT | US | 6 weeks | PPT/VAS/SF-36 | 9 |
| Luan et al. (13) | 2019 | Neck and upper back | 32.47±10.58 | 30/32 | ESWT | DN | 4 weeks | PPT/VAS/NDI | 10 |
| Gezgİnaslan et al. (14) | 2019 | Neck and upper back | 44.2±11.94 | 49/45 | H-ESWT | TENS + US | 4 weeks | VAS/SF-36/PSQI/NDI/BDI | 10 |
| Kamel et al. (15) | 2020 | Neck and upper back | 48.8±7.5 | 22/21 | ESWT | US | 4 weeks | VAS/ROM | 10 |
| Toghtamesh et al. (16) | 2020 | Neck and upper back | 28.13±3.98 | 16/16 | ESWT | DN | 4 weeks | VAS/ROM | 10 |
| Rahbar et al. (17) | 2021 | Neck and upper back | 38.09±9.67 | 22/23 | ESWT | US + HP | 4 weeks | VAS/PPT/NDI | 9 |
| Taheri et al. (18) | 2021 | Neck and upper back | 46.6±12.6 | 19/18 | ESWT | US | 4 weeks | VAS/NDI | 8 |
| Yalçın (19) | 2021 | Neck and upper back | 40.4±12.8 | 75/82 | ESWT | KT | 4 weeks | VAS/PPT/NDI | 7 |
E, experimental; C, control; PPT, pressure pain threshold; VAS, Visual Analog Scale; MPQ, McGrill pain questionnaire; PRS, Pain Rating Scale; ESWT, extracorporeal shock wave therapy; TPI, trigger point injection; TENS, transcutaneous electrical nerve stimulation; ODI, Oswestry Disability Index; RM, Roles and Maudsley; QBS, Quebec Back Pain Disability Scale scores; SF-36, Short Form-36 for quality of life; US, ultrasound; HP, hot pack; DN, dry needling; NDI, Neck Disability Index; H-ESWT, high-energy flux density ESWT; PSQI, Pittsburgh Sleep Quality Index; BDI, Beck Depression Inventory; ROM, range of motion; KT, kinesiological taping.
Risk assessment of bias of included literatures
RevMan 5.4 was used for the risk assessment of the included literature. The literature (12,18) described the allocation concealment and blindness method. The literature (11,19) did not use the random allocation method nor used the allocation concealment and blindness method. There were great implementation risks. The literature (10) did not describe the random allocation method, allocation concealment, or blindness method. All literatures described the dropout cases. There was no selective reporting bias risk or other risks, as shown in Figures 2,3.
Meta-analysis results
Pain after treatment (VAS)
All studies (10,12-19) reported the comparison of pain after treatment between the experimental group and the control group using ESWT. There was statistical heterogeneity between the studies (I2=85%, P<0.00001). Therefore, using random effects mode analysis, the pain level after treatment was lower with the ESWT method than with other treatment methods (MD =−1.34, 95% CI: −1.87 to −0.81, P<0.00001), as shown in Figure 4.
Post-treatment press pain threshold (PPT)
Six articles (10-13,17,19) reported the PPT after treatment, and the number of patients in the experimental and control groups was 177 and 187, respectively. There was statistical heterogeneity between the studies (I2=98%, P<0.00001), so the random-effects model combined analysis was used. The pain threshold after ESWT was higher than that after other treatment methods (MD =0.90, 95% CI: 0.73 to 1.07, P<0.00001), as shown in Figure 5.
Post-treatment Neck Disability Index (NDI)
Three studies (13,17,19) reported the neck disability index after treatment. Because there was statistical heterogeneity between the studies (I2=92%, P<0.00001), a random effects mode combined analysis was used. The neck disability index was lower after ESWT (MD =−1.79, 95% CI: −2.48 to −1.10, P<0.00001), as shown in Figure 6.
Heterogeneity investigation and sensitivity analysis
In the analysis of 3 main outcome indicators, there was statistically significant heterogeneity among the studies. The source of heterogeneity may be from the different sites of MPS pain. We grouped patients according to the site of pain (neck and upper back and lumborum). The results showed that there was still significant heterogeneity within the two subgroups. We excluded each other one by one and could not determine the source of heterogeneity. Therefore, the source of heterogeneity in our analysis may be a mixture of multiple factors, such as patient age, pain site, treatment time and follow-up time, and different treatment methods in the experimental group and control group.
In the analysis of posttreatment pain, if the effect mode was changed to the fixed effect mode, the effect size was obtained (MD =−1.20, 95% CI: −1.39 to −1.01, P<0.00001), which was not significantly different from the results of the random effect mode, indicating that the results of the meta-analysis were stable.
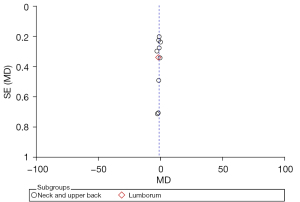
Analysis of publication bias
In the analysis of pain after treatment, the funnel plot showed that both sides were evenly distributed, suggesting that there was a small possibility of publication bias, as shown in Figure 7.
Discussion
ESWT therapy was initially applied in the lithotripsy of renal calculi and later in the treatment of long-term nonunion of fractures, gradually moving toward the field of treatment of chronic pain. ESWT is a noninvasive physical therapy method that is simple to perform, noninvasive, and has no adverse effects (22). In this study, 10 controlled clinical studies were included. Meta-analysis was performed to determine the therapeutic effect of ESWT on MPS. The results showed that compared with other treatment methods, ESWT can reduce pain, increase the pain threshold, and reduce the shoulder and neck disability index, providing an evidence-based basis for the application of ESWT in the treatment of MPS.
In the control groups in the literature (10,11), the TPI treatment method was adopted, and the principle was to inject analgesic drugs (glucocorticoids and local anesthetics) into the trigger points to eliminate inflammation, block pain, and reduce edema. However, this treatment method lacks long-term effects, and the direct injection of drugs may bring allergic reactions and other adverse reactions (23). Extracorporeal shock waves do not require invasive procedures and directly conduct energy through the skin into muscle tissue to improve microcirculation and promote the separation of adherent soft tissues, which can have a long-acting analgesic effect (14).
In the literature (13,16), the control group adopted the dry needling method, and the effect size result of pain VAS showed that the pain relief rate of ESWT was superior to that of acupuncture. It is noteworthy that in the literature (13), the improvement rate for PPT was better with dry needling therapy than with ESWT therapy. Acupuncture therapy from different angles to continuously stimulate and destroy the trigger pain points to achieve the purpose of treatment, this approach has a good effect, but the patient’s tolerance and compliance are poor, and it still belongs to the category of invasive procedures.
Ultrasound-guided pulsed radiofrequency is a noninvasive procedure similar to ESWT that can emit high-frequency pulse current, promote local separation of adherent tissue, and effectively avoid nerve injury. However, this method has a poor energy transfer effect and a low pain relief rate. The control group in previous studies (12,14,15,18) was treated with ultrasound-guided pulsed radiofrequency, but the rate of pain relief was worse than that of ESWT.
It should be noted that in the study by Király et al. (20), the innovative combination of ESWT and laser was applied in the treatment of MPS, and the results showed that the effect was better than ESWT alone, which suggested that in the clinical treatment, the physician could reasonably combine ESWT with different treatment methods. This could not only improve the therapeutic effect and shorten the treatment course but also increase the patient’s tolerance and reduce adverse reactions.
In the study by Park et al. (24), high-energy density (0.210 mJ/mm) was compared with the low-energy density (0.068 mJ/mm) ESWT method, and the results showed that high-energy density ESWT was superior to low-energy density treatment in improving symptoms and relieving pain, but its safety and efficacy still require more research support.
This study found that there was great heterogeneity among the 10 studies, and the heterogeneity was derived from the confounding of multiple factors. The funnel plot of this study showed that both sides were evenly distributed, without significant publication bias. The sensitivity analysis showed that the results were stable. However, in this study, some studies did not use the random allocation method, which may cause implementation bias. More controlled clinical studies with the same assessment method with the same case characteristics should be explored in depth in the future.
Conclusions
In conclusion, ESWT can avoid the adverse effects of invasive procedures on patient tolerance and compliance; compared with TPI, dry needling and US, ESWT can more effectively relieve the pain of MPS patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-295/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-295/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Borg-Stein J, Iaccarino MA. Myofascial pain syndrome treatments. Phys Med Rehabil Clin N Am 2014;25:357-74. [Crossref] [PubMed]
- Money S. Pathophysiology of Trigger Points in Myofascial Pain Syndrome. J Pain Palliat Care Pharmacother 2017;31:158-9. [Crossref] [PubMed]
- Urits I, Charipova K, Gress K, et al. Treatment and management of myofascial pain syndrome. Best Pract Res Clin Anaesthesiol 2020;34:427-48. [Crossref] [PubMed]
- Sugawara AT, Lima MDC, Dias CB. Predictive factors of response in radial Extracorporeal Shock-waves Therapy for Myofascial and Articular Pain: A retrospective cohort study. J Back Musculoskelet Rehabil 2021;34:485-90. [Crossref] [PubMed]
- Galasso A, Urits I, An D, et al. A Comprehensive Review of the Treatment and Management of Myofascial Pain Syndrome. Curr Pain Headache Rep 2020;24:43. [Crossref] [PubMed]
- Yoo JI, Oh MK, Chun SW, et al. The effect of focused extracorporeal shock wave therapy on myofascial pain syndrome of trapezius: A systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e19085. [Crossref] [PubMed]
- Jun JH, Park GY, Chae CS, et al. The Effect of Extracorporeal Shock Wave Therapy on Pain Intensity and Neck Disability for Patients With Myofascial Pain Syndrome in the Neck and Shoulder: A Meta-Analysis of Randomized Controlled Trials. Am J Phys Med Rehabil 2021;100:120-9. [Crossref] [PubMed]
- Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage 2011;41:1073-93. [Crossref] [PubMed]
- Cashin AG, McAuley JH. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother 2020;66:59. [Crossref] [PubMed]
- Jeon JH, Jung YJ, Lee JY, et al. The effect of extracorporeal shock wave therapy on myofascial pain syndrome. Ann Rehabil Med 2012;36:665-74. [Crossref] [PubMed]
- Hong JO, Park JS, Jeon DG, et al. Extracorporeal Shock Wave Therapy Versus Trigger Point Injection in the Treatment of Myofascial Pain Syndrome in the Quadratus Lumborum. Ann Rehabil Med 2017;41:582-8. [Crossref] [PubMed]
- Aktürk S, Kaya A, Çetintaş D, et al. Comparision of the effectiveness of ESWT and ultrasound treatments in myofascial pain syndrome: randomized, sham-controlled study. J Phys Ther Sci 2018;30:448-53. [Crossref] [PubMed]
- Luan S, Zhu ZM, Ruan JL, et al. Randomized Trial on Comparison of the Efficacy of Extracorporeal Shock Wave Therapy and Dry Needling in Myofascial Trigger Points. Am J Phys Med Rehabil 2019;98:677-84. [Crossref] [PubMed]
- Gezgİnaslan Ö. GÜmÜŞ Atalay S. High-Energy Flux Density Extracorporeal Shock Wave Therapy Versus Traditional Physical Therapy Modalities in Myofascial Pain Syndrome: A Randomized-controlled, Single-Blind Trial. Arch Rheumatol 2019;35:78-89. [PubMed]
- Kamel FH, Basha M, Alsharidah A, et al. Efficacy of Extracorporeal Shockwave Therapy on Cervical Myofascial Pain Following Neck Dissection Surgery: A Randomized Controlled Trial. Ann Rehabil Med 2020;44:393-401. [Crossref] [PubMed]
- Toghtamesh M, Tajali SB, Jalaei S. Comparing between the effects of dry needling and shock wave in the treatment of trapezius myofascial pain. Journal of Modern Rehabilitation 2020;14:225-32.
- Rahbar M, Samandarian M, Salekzamani Y, et al. Effectiveness of extracorporeal shock wave therapy versus standard care in the treatment of neck and upper back myofascial pain: a single blinded randomised clinical trial. Clin Rehabil 2021;35:102-13. [Crossref] [PubMed]
- Taheri P, Naderi M, Khosravi S. Extracorporeal Shock Wave Therapy Versus Phonophoresis Therapy for Neck Myofascial Pain Syndrome: A Randomized Clinical Trial. Anesth Pain Med 2021;11:e112592. [PubMed]
- Yalçın Ü. Comparison of the effects of extracorporeal shockwave treatment with kinesiological taping treatments added to exercise treatment in myofascial pain syndrome. J Back Musculoskelet Rehabil 2021;34:623-30. [Crossref] [PubMed]
- Király M, Bender T, Hodosi K. Comparative study of shockwave therapy and low-level laser therapy effects in patients with myofascial pain syndrome of the trapezius. Rheumatol Int 2018;38:2045-52. [Crossref] [PubMed]
- Ramon S, Gleitz M, Hernandez L, et al. Update on the efficacy of extracorporeal shockwave treatment for myofascial pain syndrome and fibromyalgia. Int J Surg 2015;24:201-6. [Crossref] [PubMed]
- Wang HJ, Cheng JH, Chuang YC. Potential applications of low-energy shock waves in functional urology. Int J Urol 2017;24:573-81. [Crossref] [PubMed]
- Okada-Ogawa A, Sekine N, Watanabe K, et al. Change in muscle hardness after trigger point injection and physiotherapy for myofascial pain syndrome. J Oral Sci 2019;61:36-44. [Crossref] [PubMed]
- Park KD, Lee WY, Park MH, et al. High- versus low-energy extracorporeal shock-wave therapy for myofascial pain syndrome of upper trapezius: A prospective randomized single blinded pilot study. Medicine (Baltimore) 2018;97:e11432. [Crossref] [PubMed]







