Peripherally located endobronchial hamartoma mimicking aspergilloma: a case report
Introduction
Hamartomas, one of the commonest benign pulmonary tumors, are categorized as centrally-located endobronchial and peripherally located pulmonary types. We herein report a case of a hamartoma originating from a peripheral bronchus that resembled an aspergilloma on a computed tomography (CT) scan.
Case presentation
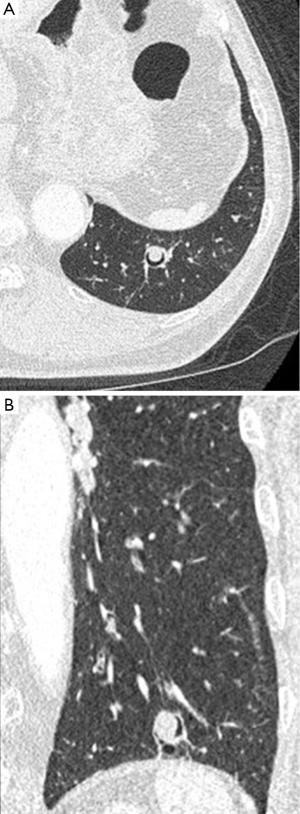
An asymptomatic 75-year-old man was referred to our hospital for assessment of an abnormal shadow detected by screening chest radiography. A chest CT scan revealed a 13-mm diameter nodule with an air crescent sign in the posterior basal segment of the left lung (Figure 1). [18F]-2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET)-CT revealed no significant uptake within the nodule. The serum concentration of β-D glucan was within normal limits; however, the serum concentration of aspergillus antigen was 0.5 (cut off index; reference value 0.5). Trans-bronchial biopsy and brushing cytology showed no malignant cells. Cultures for acid-fast bacilli and fungi were negative. The patient underwent antifungal treatment with itraconazole for 1 year, during which the CT appearance of the nodule did not change. Therefore video-assisted radical left lower lobectomy was performed and was successful.
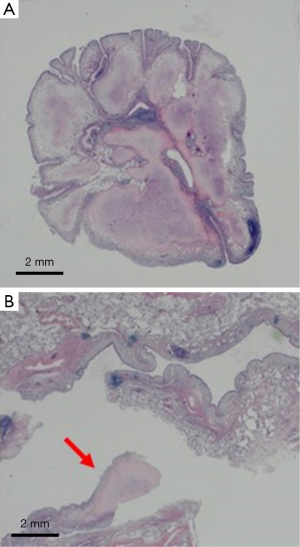
Macroscopically, the target lesion was a well-defined 13-mm diameter white mass within the fifth branch of the dilated posterior basal segmental bronchus of the left lung. A pedicle of the lesion was identified in the dilated bronchial wall (Figure 2). Microscopically, the lesion consisted of chondroid tissue covered with bronchial-type epithelium and was diagnosed as a chondromatous hamartoma (Figure 3). The dilated bronchi were rich in goblet and smooth muscle cells. No fungal elements were detected within the lesion.

The patient was doing well without any complications 3 years after surgery.
Discussion
Pulmonary hamartomas are the most common benign tumors of the lung, comprising 41.9% of reported lung tumors (1). Pulmonary hamartomas are classified as peripherally located pulmonary and centrally located endobronchial types. Endobronchial hamartomas occur less frequently, accounting for 2.5–19.5% of hamartomas (2). Peripheral endobronchial hamartomas are very rare. A search of PubMed using the key words of pulmonary hamartoma and/or endobronchial hamartoma identified a few reports (3-5). One of these articles reported a 35-mm diameter endobronchial tumor that had developed in the anterior superior segment of the right lung adjacent to pleura (3) and another a 20-mm diameter endobronchial tumor in the posterior basal segment of the right lung (4). In the latter case, a radical right upper lobectomy was performed because of a misdiagnosis of lung cancer that was based on enlargement of the hilar lymph nodes.
On CT imaging, pulmonary hamartomas typically appear as well-defined solitary pulmonary nodules in a peripheral location; 34–50% of them contain fat and 15–30% calcification. In our case, a chest CT scan showed an air crescent sign without any of the above features.
An air crescent sign on a radiologic image is the result of collection of air around a pulmonary nodule. Well-demarcated pulmonary tumors such as sclerosing hemangiomas and solitary fibrous tumors can show the air crescent sign, which indicates that air has been trapped around the tumor (6,7). The air crescent sign is typically caused by an aspergilloma located within a preexisting thin-walled cavity with a smooth inner margin, most often formed by a previous tuberculous infection in the upper lobe. Lung cancer, tuberculosis, hydatid cyst, cystic bronchiectasis filled with mucus plugs, and bacterial lung abscess may also cause air crescent signs with or without aspergillus infection (8,9). Pulmonary aspergillomas are typically positive on PET-CT, but may be negative (10). In our case, the lesion was misdiagnosed as an aspergilloma based on these clinical features, leading eventually to radical lobectomy. Such lesions should be excised by radical surgery to obtain a definite diagnosis.
In conclusion, physicians should note that peripherally located hamartomas can develop within the peripheral bronchi resulting in an air crescent appearance on radiological images.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shiozawa M. Hamartoma of the lung. Nihon Kyobu Geka Gakkai Zasshi 1973;21:87-100. In Japanese.
- Bateson EM. So-called hamartoma of the lung--a true neoplasm of fibrous connective tissue of the bronchi. Cancer 1973;31:1458-67. [PubMed]
- Kanauchi T, Hoshi T, Sugiura T, et al. Three cases of pulmonary hamartoma originating from bronchus and bronchiole. Japan Society for Bronchology 2006;51:178-82. Available online: www.jsre.org. In Japanese.
- Mega S, Oguri M, Okubo T, et al. A case of peripheral Endobronchial hamartoma with Sarcoid Reaction in Regional Lymph Nodes. The Journal of the Japan Society for Respiratory Endoscopy 2008;30:124-8. In Japanese.
- Tomashefski JF Jr. Benign endobronchial mesenchymal tumors: their relationship to parenchymal pulmonary hamartomas. Am J Surg Pathol 1982;6:531-40. [PubMed]
- Wang QB, Chen YQ, Shen JJ, et al. Sixteen cases of pulmonary sclerosing haemangioma: CT findings are not definitive for preoperative diagnosis. Clin Radiol 2011;66:708-14. [PubMed]
- Kanai Y, Endo S, Tetsuka K, Nokubi M. Pleural solitary fibrous tumor with bullae: is it a microinvasive tumor? Gen Thorac Cardiovasc Surg 2012;60:122-4. [PubMed]
- Bandoh S, Fujita J, Fukunaga Y, et al. Cavitary lung cancer with an aspergilloma-like shadow. Lung Cancer 1999;26:195-8. [PubMed]
- Santos JW, Machado FP, Schaichet F, et al. Unusual cavity lung lesion in an asymptomatic patient—Case report and differential diagnosis. Respiratory Medicine Extra 2007;3:186-8.
- Cucchetto G, Cazzadori A, Conti M, et al. Treatment of chronic pulmonary aspergillosis with voriconazole: review of a case series. Infection 2015;43:277-86. [PubMed]


