Pharmacist-led standardization of total parenteral nutrition improves postoperative nutritional status in colorectal cancer patients
Introduction
The surgical stress response can induce catabolism, which often leads to postoperative malnutrition (1,2). The effect is even more pronounced in patients with cancer, since preoperative malnutrition is more prevalent among such patients (3,4). Perioperative patients are usually required to fast. Due to the special surgical site, the recovery time of gastrointestinal function is longer in patients who undergo gastrointestinal surgery compared to patients receiving other surgeries (5). In addition, the delayed intestinal peristalsis caused by intraoperative anesthetics, postoperative analgesia, and perioperative antiemetics also prolongs the time of fasting. Therefore, although the enhanced recovery after surgery (ERAS) program advocates early oral feeding as the preferred mode of nutrition for surgical patients (6), in many cases, parenteral nutrition (PN), usually total parenteral nutrition (TPN), remains indispensable in perioperative patients with colorectal cancer (CRC).
Preoperative malnutrition tends to be more common in CRC compared to some other malignancies (7,8). Surgical stress induces nutritional consumption, which further aggravates postoperative malnutrition. Nutritional status is related to the incidence of postoperative complications in the short term (9), and may affect the prognosis of patients in the long-term (10). Results of a retrospective multicenter study based on the ACS-NSQIP database showed that perioperative nutrition was significantly associated with postoperative mortality in patients with CRC (7). Therefore, the appropriate use of PN is essential for perioperative patients with CRC.
PN treatment is usually administered in the form of total nutrient admixture (TNA), which is composed of different nutrients, including glucose, amino acids, intravenous fat emulsions (IVFE), vitamins, electrolytes, and trace elements all in one bag. Thus, there are many factors to consider in TPN prescription, such as stability of the TNA, as well as individual nutritional needs of the patient. For example, the concentration of divalent ions affects the stability of the emulsion and the safety of the PN infusion (11). Moreover, non-protein energy (NPE), amino acid supply, the proportion of energy from fat, and individual characteristics of the patients, are all parameters that play a role in the computational complexity of PN prescription (12). In clinics, perioperative PN is usually prescribed by surgeons. Our previous investigations (data not shown) showed that, due to workload and specialty limitation, the PN prescriptions issued by surgeons are often unsatisfactory. Lack of individualization and incompatibility are common problems of TNA. Sub-optimal TPN prescriptions may not only affect the efficacy of the TNA, but may also affect the safety and clinical outcomes of the patient. Hence, a pharmacist-led TPN standardization program was introduced. With the development of clinical pharmacy and the refinement of specialty division of clinical pharmacists, the nutritionist-pharmacists are usually received systematic training in the use of TPN. The intervention of nutritional pharmacists is expected to improve the administration and standardization of TPN prescriptions. Participation of pharmacists in multidisciplinary teams (MDT) has been shown in many studies to improve treatment standardization and patient outcomes, including improved PN compatibility and stability (13,14). To evaluate the role of pharmacists in the postoperative complications and nutritional status of perioperative patients with CRC, a retrospective study was conducted examining patients’ outcomes before and after the introduction of pharmacist-led TPN intervention. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1172/rc).
Methods
The standardization of the pharmacist-led parenteral nutrition program
A pharmacist-led standardization program for PN administration was introduced in the Zhejiang Cancer Hospital (Hangzhou, China). An evaluation standard of perioperative PN was established by pharmacists based on the guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN), the American Society for Parenteral and Enteral Nutrition (ASPEN), and the Chinese Medical Association for Parenteral and Enteral Nutrition (CSPEN). The evaluation standard was then published in the hospital for multidisciplinary advice and final revision. Subsequently, a computerized TPN management system was developed and applied, including a prescription management system and evaluation software, to identify and reduce unsuitable prescriptions. The prescription rationality control system was embedded in the electronic prescription platform to intercept extraordinary PN prescriptions, especially those with incompatibility issues and inappropriate formulation. The prescription rationality evaluation software was used regularly to evaluate the individualization of PN prescription for different patients. For continuous improvement, the inappropriate prescriptions were sorted out and feedback was provided to the doctors for confirmation. Any concerns were identified and improved after discussed with doctors. Different templates of TPN prescription suitable for patients with different weight ranges are also set in the electronic medical record for reference.
Setting and participants
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by institutional ethics committee of Zhejiang Cancer Hospital (No. IBR-2022-53). Individual patient consent for this study was waived due to the retrospective nature of this investigation.
This retrospective observational before-and-after cohort study was performed in the Zhejiang Cancer Hospital. All patients admitted to the CRC oncology surgery ward in June 2019 and June 2020 were retrospectively analyzed. The following inclusion criteria were applied: (I) patients were pathologically diagnosed with colon or rectal cancer; and (II) the patient underwent surgery during this period. The following exclusion criteria were applied: (I) the primary lesions was not in the colorectal site, such as ovarian cancer, cervical malignancy, small intestinal malignancy, etc.; (II) pathological diagnosis was not colorectal adenocarcinoma, such as benign tumor, polyp, neuroendocrine tumor, stromal tumor, lymphoma, etc.; (III) the patient did not receive surgical treatment; and (IV) instead of traditional/customized TPN, commercially available premade (“premixed”) multichambered PN was administered.
Source of data
The clinical information of the patients and the TPN-related information were retrieved from electronic databases using medical record archives as follows: (I) patient information including age, gender, weight, tumor type, operation type, hematological examination, hospital stay time, etc.; and (II) TPN prescriptions.
Data evaluation
As described above, the TPN rationality was evaluated by the standard established and calculated by the self-developed evaluation software. TPN prescription with 20–35 kcal/kg/d NPE, ≤50% energy supplied from fat of NPE, ≥1.0 g/kg/d amino acid supply, and 100–200:1 of the ratio of NPE/nitrogen was assessed as appropriate. Postoperative nutritional status was evaluated using the levels of postoperative serum albumin, prealbumin, total protein, and extent of decrease in these indicators after surgery. Clinical outcomes were collated, including surgical complications such as postoperative infection, TPN-related complications such as hypoglycemia, and length of hospital stay post-surgery. To evaluate the grade of hypoalbuminemia, the standard of Common Terminology Criteria Adverse Events (CTCAE) 5.0 was applied.
Bias
To address potential sources of bias, the same month of the year (June) was selected for comparison. Data for the whole month were analyzed, rather than a fixed total sample size, to avoid bias caused by sampling. However, as a retrospective study, a degree of bias was inevitable.
Missing data
If the proportion of missing data was greater than 40%, the variable would be discarded and not analyzed. If the missing proportion of the variable was less than 10%, the missing values would be ignored, otherwise, the median value would be used to populate the missing value.
Statistical analyses
The GraphPad Prism software (version 5.0, GraphPad Software, La Jolla California, USA) was used for statistical analyses. Continuous variables are expressed as mean ± SEM and categorical variables are expressed as counts and percentages. Student’s t-tests were performed to analyze the continuous data of two groups. Chi-squared (χ2) and Fisher’s exact tests were used to evaluate the differences between groups of categorical variables. For all tests, a two-sided P value <0.05 was considered statistically significant.
Results
Basic clinical information of the patients
A total of 167 patients from June 2019 and 157 patients from June 2020 were initially enrolled in this retrospective study. After application of the inclusion and exclusion criteria, a total of 137 patients from June 2019 and 147 from June 2020 were selected for further analysis. The details of the study flow chart are showed in Figure 1. The basic clinical information of the patients is shown in Table 1. There were no significant differences in gender, age, cancer type, nor surgical type between the two groups (P>0.05).

Table 1
| Variables | June 2019 (n=137) | June 2020 (n=147) | P value | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender | 0.899 | |||||
| Male | 93 | 67.9 | 98 | 66.7 | ||
| Female | 44 | 32.1 | 49 | 33.3 | ||
| Age (y) | 0.629 | |||||
| ≥65 | 53 | 38.7 | 62 | 42.2 | ||
| <65 | 84 | 61.3 | 85 | 57.8 | ||
| Cancer type | 0.856 | |||||
| Colon cancer | 50 | 36.5 | 55 | 37.4 | ||
| Rectal cancer | 86 | 62.8 | 90 | 61.2 | ||
| Colorectal cancer | 1 | 0.7 | 2 | 1.4 | ||
| Surgical type | 0.771 | |||||
| Tumor radical or partial resection | 123 | 89.8 | 128 | 87.1 | ||
| Enterostomy or Stoma closure | 12 | 8.8 | 16 | 10.9 | ||
| Othersa | 2 | 1.5 | 3 | 2.0 | ||
a, others include exploratory laparotomy, laparoscopic enterolysis, etc.
Missing data
Among the variables collected in this study, no missing value were detected in the TPN prescription information, postoperative infection, nor hospital-stay time. There were 4 cases from June 2019 and 0 cases from June 2020 with missing albumin and total protein values. A total of 9 cases from June 2019 and 4 cases from June 2020 had missing prealbumin data. Since there were few missing values, the missing data were ignored without special consideration.
Pharmacist-led standardization improved the rationality of TPN
The TPN rationality was evaluated. As seen in Table 2, pharmacist-led standardization improved the proportion of TPN with appropriate NPE, energy composition, and ratio of NPE to nitrogen (NPE/N). The proportion of TPN with NPE at 20–35 kcal/kg/d increased (60.6% for 2019 vs. 70.7% for 2020, P=0.004), as recommended. It was also recommended to increase the ratio of energy from fat to energy from carbohydrates, up to 50%. In June 2019, 96.4% of TPNs met this recommendation, while in June 2020, the proportion raised to 100% (P>0.05). The ratio of NPE/N was recommended as 100–200 kcal/g nitrogen. The proportion of TPN with appropriate NPE/N was 88.3% in 2019 and 95.9% in 2020 (P=0.049). A minimum dose of 1.0 g/kg/d amino acid supply was considered necessary according to the guideline. However, there was no significant difference in the amino acid supply between the two groups (P=0.511).
Table 2
| TPN ingredient | Year 2019 (n=137) | Year 2020 (n=147) | P | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Non-protein energy (NPE) | 0.004 | |||||
| <20 kcal/kg/d | 45 | 32.8 | 43 | 29.3 | ||
| 20–35 kca/kg/d (R) | 83 | 60.6 | 104 | 70.7 | ||
| >35 kcal/kg/d | 9 | 6.6 | 0 | 0.0 | ||
| Fat energy/NPE | 0.997 | |||||
| ≤50% (R) | 132 | 96.4 | 147 | 100.0 | ||
| 50% | 5 | 3.6 | 0 | 0.0 | ||
| Amino acid | 0.511 | |||||
| <1.0 g/kg/d | 42 | 30.7 | 39 | 26.5 | ||
| ≥.5 g/kg/d (R) | 95 | 69.3 | 108 | 73.5 | ||
| NPE/nitrogen | 0.049 | |||||
| <100:1 | 15 | 10.9 | 6 | 4.1 | ||
| 100–200:1 (R) | 121 | 88.3 | 141 | 95.9 | ||
| >200:1 | 1 | 0.7 | 0 | 0 | ||
R: the indicator is preferentially recommended.
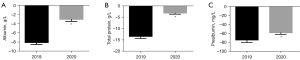
Pharmacist-led intervention improved postoperative nutritional status
To evaluate the impact of pharmacist-led TPN standardization on clinical outcomes, the postoperative nutritional status of patients was examined. As shown in Table 3 and Figure 2, compared with preoperative level, postoperative decline of serum albumin, total protein, and prealbumin occurred in both 2019 and 2020. However, the proportion of decrease and the levels were significantly reduced in 2020. In June 2019, 76.7% of patients with CRC had postoperative albumin reduction, while the proportion was decreased to 25.2% in June 2020. The mean difference in decreased value of albumin also reduced from −8.11±0.43 to −3.08±0.44 g/L (P<0.0001). Similar, in June 2019, the proportion of postoperative total protein decrease was 72.2%, with an average decrease of −13.48±0.90 g/L. By June 2020, the proportion of postoperative total protein decrease had improved to 25.2%, with an average decrease of −3.24±0.45 g/L (P<0.0001). The decrease in postoperative prealbumin was also improved (−74.84±5.76 mg/L for 2019 vs. −58.69±3.65 mg/L for 2020, P=0.019).
Table 3
| Variables | June 2019 | June 2020 | P |
|---|---|---|---|
| Albumin decrease (n) | 133 | 147 | |
| Rate (%) | 76.7 | 25.2 | |
| Decrease average (g/L) | −8.11±0.43 | −3.08±0.44 | <0.0001 |
| Total protein decrease (n) | 133 | 147 | |
| Rate (%) | 72.2 | 25.2 | |
| Decrease average (g/L) | −13.48±0.90 | −3.24±0.45 | <0.0001 |
| Prealbumin decrease (n) | 128 | 143 | |
| Rate (%) | 78.9 | 71.5 | |
| Decrease average (mg/L) | −74.84±5.76 | −58.69±3.65 | 0.019 |
The value of postoperative serum albumin, total protein, and prealbumin were missing in several patients as no tests were performed.
Furthermore, the absolute values of postoperative serum albumin, total protein, and prealbumin were analyzed (Figure 3). Compared with June 2019, the level of postoperative serum prealbumin in June 2020 increased significantly (192.3±5.5 mg/L for 2019 and 229.5±4.8 mg/L for 2020, P<0.001). However, there was no significant change in the absolute values of postoperative total serum protein. The postoperative serum albumin was divided into four grades according to the standard of the Common Terminology Criteria Adverse Events (CTCAE) Version 5.0. As shown in Table 4, after the intervention of pharmacists, the proportion of grade 2 (postoperative serum albumin ≥20 and <30 g/L) decreased significantly, from 21.1% in 2019 to 6.1% in 2020 (P=0.001).

Table 4
| Grades of postoperative hypoproteinemia | Year 2019 | Year 2020 | P | |||
|---|---|---|---|---|---|---|
| na | % | na | % | |||
| Total | 133 | 147 | 0.001 | |||
| Grade 0: ≥40 (g/L) | 18 | 13.5 | 25 | 17.0 | ||
| Grade 1: ≥30 and <40 (g/L) | 87 | 65.4 | 113 | 76.9 | ||
| Grade 2: ≥20 and <30 (g/L) | 28 | 21.1 | 9 | 6.1 | ||
| Grade 3: <20 (g/L) | 0 | 0.00 | 0 | 0.00 | ||
a, the number of cases. There were 4 cases data of serum albumin censored in Year 2019. The level of postoperative serum albumin was divided into four grades according to the standard of Common Terminology Criteria Adverse Events (CTCAE) Version 5.0.
Pharmacist-led intervention reduced postoperative complications
Data regarding postoperative infection, time to discharge after surgery, and TPN-related hypoglycemia were collated to evaluate the effect of pharmacist intervention on postoperative complications and recovery. The results demonstrated that postoperative infection rates decreased from 18.2% (25/137) in June 2019 to 11.6% (17/147) in June 2020. The infection time was also reduced from 9.4±1.4 to 7.7±1.0 days (P=0.368). By controlling the range of insulin dosage in the TPN, the pharmacist-led intervention decreased the incidence of TPN related hypoglycemia from 15.3% in June 2019 to 5.4% in June 2020. However, there was no difference in discharge time after surgery between the two groups (10.3 days in 2019 vs. 11.0 days in 2020, P=0.110).
Discussion
This current study demonstrated that pharmacist-led TPN standardization improved the postoperative clinical outcomes in patients with CRC. Compared to 2019, the average postoperative prealbumin and albumin levels were increased in 2020, with a smaller decrease in postoperative albumin, prealbumin, and total protein. In addition, lower postoperative infection rates, shorter infection times, and lower incidence of TPN-related hypoglycemia were observed in 2020.
The “systemic inflammatory response syndrome” is characterized by a series of inflammatory reactions that are activated to achieve injury healing and functional recovery after surgery. Metabolic responses are necessary for this process. In particular, nutrients such as glycogen, fat, and protein will be catabolized during this response (15-17). Thus, perioperative nutritional support is vital for postoperative recovery. Indeed, impaired nutritional status is one of the risk factors of postoperative complications and can lead to malnourishment and long-term stress/inflammation. Therefore, perioperative management, including nutrition, is essential for long-term outcome, especially in patients with cancer (17-19).
CRC is the third common cancer globally and the second leading cause of cancer-related deaths, with 1.93 million new cases and 0.9 million deaths worldwide in 2020 (20). Bowel obstruction and malabsorption are common complications of CRC, leading to patient malnutrition (7). A 1-day prevalence survey that investigated 154 French hospitals showed that 39.3% of the 1,903 CRC patients were malnourished (8). Moreover, in CRC, malnutrition was found to be significantly related to prolonged total hospital stay and 30-day mortality after surgery (7). Thus, appropriate and adequate perioperative nutritional therapy is undoubtedly crucial for patients with CRC.
Participation of pharmacists in multidisciplinary teams (MDT) has been shown in many studies to improve treatment standardization and patient outcomes, including improved PN compatibility and stability (13,14), increased adherence to guideline-based management in warfarin use (21), as well as improved venous thromboembolism (VTE) prophylaxis (22). In the present study, we evaluated the impact of pharmacist-led standardization of TPN on postoperative nutritional status and complications in patients with CRC. The results demonstrated that pharmacist intervention improved the adherence to guideline-based TPN standardization.
The recommended resting energy expenditure (REE) for cancer patients is 25–30 kcal/kg (23). Only NPE is calculated for PN, thus the minimum recommended REE is reduced to 20 kcal/kg/d for NPE. Also, considering the energy expenditure of physical activities and stress response, the upper limit of total energy expenditure (TEE) of 35 kcal/kg/d is recommended in our study. A range of 20–35 kcal/kg/d of TEE was evaluated as rational. Pharmacist intervention increased the proportion of TPN with rational NPE. It has been recommended by ESPEN that the ratio of energy from fat in NPE for cancer patients should be increased up to 50% (24). The mean ratio of NPE to nitrogen was found to be 130 kcal/g nitrogen (23). Thus, a range of 100–200 kcal/g NPE/nitrogen was recommended. Pharmacist participation improved the above-mentioned indicators of TPN. The optimal nitrogen supply for cancer patients has not been determined. At present, a minimum protein supply of 1 g/kg/day is recommended according to the ESPEN guideline (23). The proportion of TPN with amino acid supply ≥1 g/kg increased slightly after the pharmacist intervention, however, there was no significant difference between the groups.
Serum albumin is a recognized factor that reflects the nutritional status of patients (25) and has been widely used as a predictor of outcome (26,27), including postoperative outcome of cancer patients (3,28,29). Prealbumin is another commonly used indicator of nutritional status. Low prealbumin levels indicate malnutrition (30), and are associated with sarcopenia (31) and adverse prognosis (32). Due to its short half-life, prealbumin is more sensitive than albumin in reflecting the changes in nutritional status in the short-term. In some cases, prealbumin levels have been found to be the best independent nutritional predictor (33). Our results showed that the average postoperative prealbumin levels were higher in 2020 (after intervention) compared to 2019 (before intervention). The decline of postoperative serum albumin, total protein, and prealbumin were all improved in the invention group, suggesting that the pharmacist-led standardization protocol improved the postoperative nutritional status of patients with CRC.
The nutritional status of patients is associated with the incidence of postoperative complications, including infections (34). Our results revealed that postoperative infection rates were decreased after pharmacist-led TPN standardization. In addition, the rate of TPN-related hypoglycemia was also reduced. Most TPN infusions end in the early morning, which corresponds with the time of low physiological blood glucose levels. Together with the adsorption and sudden release of insulin by the TPN container, hypoglycemia often occurs at the end of TPN infusions, often in the early morning. To date, there has been no universally acknowledged recommendation for the dosing regimen of insulin in TNA. The dose of insulin must be tailored individually to avoid hypoglycemia. In this study, the pharmacist suggested different empirical ranges of insulin for patients with or without diabetes, reduced the initial dose of insulin, and increased the frequency of insulin adjustment individually for each patient. This specialized intervention resulted in a reduced incidence of TPN-related hypoglycemia.
There were some limitations to this study. First, this report is a retrospective study rather than a prospective, randomized, controlled study. Therefore, several interfering factors may exist which may affect the results. Second, several indicators of postoperative outcome may be affected by medical policy or clinical practice. For example, the discharge time of patients may be affected by the lack of beds and policies related to the rate of bed turnover. Finally, the current management by pharmacists is not optimal due to the shortage of manpower. A refined management system for the administration of PN for individual patients should be designed, and a prospective study should be conducted in the future.
Acknowledgments
Funding: This work was supported by the Medical Science Research Foundation of Zhejiang Province (Grant No. 2020KY459 to Yinghui Tong), the Hospital Pharmaceutical Research Funding of Zhejiang Pharmaceutical Association (Grant No. 2018ZYY26 to Yinghui Tong), and the Research Project on Tumor Pharmaceutical Affair Quality Control Standard of Professional Committee of Tumor Clinical Pharmacy of China Anti-Cancer Association (Grant No. Z19ZJZL103 to Yinghui Tong).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1172/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1172/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1172/coif). YT reports that this work was supported by the Medical Science Research Foundation of Zhejiang Province (Grant No. 2020KY459), the Hospital Pharmaceutical Research Funding of Zhejiang Pharmaceutical Association (Grant No. 2018ZYY26), and the Research Project on Tumor Pharmaceutical Affair Quality Control Standard of Professional Committee of Tumor Clinical Pharmacy of China Anti-Cancer Association (Grant No. Z19ZJZL103). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by institutional ethics committee of Zhejiang Cancer Hospital (No. IBR-2022-53). Individual patient consent for this study was waived due to the retrospective nature of this investigation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Phillips BE, Smith K, Liptrot S, et al. Effect of colon cancer and surgical resection on skeletal muscle mitochondrial enzyme activity in colon cancer patients: a pilot study. J Cachexia Sarcopenia Muscle 2013;4:71-7. [Crossref] [PubMed]
- Yeung SE, Hilkewich L, Gillis C, et al. Protein intakes are associated with reduced length of stay: a comparison between Enhanced Recovery After Surgery (ERAS) and conventional care after elective colorectal surgery. Am J Clin Nutr 2017;106:44-51. [PubMed]
- Gupta A, Gupta E, Hilsden R, et al. Preoperative malnutrition in patients with colorectal cancer. Can J Surg 2021;64:E621-9. [Crossref] [PubMed]
- Matthews LS, Wootton SA, Davies SJ, et al. Screening, assessment and management of perioperative malnutrition: a survey of UK practice. Perioper Med (Lond) 2021;10:30. [Crossref] [PubMed]
- Piric M, Pasic F, Rifatbegovic Z, et al. The Effects of Drinking Coffee While Recovering from Colon and Rectal Resection Surgery. Med Arch 2015;69:357-61. [Crossref] [PubMed]
- Weimann A, Braga M, Carli F, et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin Nutr 2021;40:4745-61. [Crossref] [PubMed]
- Hu WH, Cajas-Monson LC, Eisenstein S, et al. Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 2015;14:91. [Crossref] [PubMed]
- Hébuterne X, Lemarié E, Michallet M, et al. Prevalence of malnutrition and current use of nutrition support in patients with cancer. JPEN J Parenter Enteral Nutr 2014;38:196-204. [Crossref] [PubMed]
- Qi Q, Song Q, Cheng Y, et al. Prognostic Significance of Preoperative Prognostic Nutritional Index for Overall Survival and Postoperative Complications in Esophageal Cancer Patients. Cancer Manag Res 2021;13:8585-97. [Crossref] [PubMed]
- Wiseman MJ. Nutrition and cancer: prevention and survival. Br J Nutr 2019;122:481-7. [Crossref] [PubMed]
- Gervasio J. Total nutrient admixtures (3-in-1): pros vs cons for adults. Nutr Clin Pract 2015;30:331-5. [Crossref] [PubMed]
- Boullata JI, Gilbert K, Sacks G, et al. A.S.P.E.N. clinical guidelines: parenteral nutrition ordering, order review, compounding, labeling, and dispensing. JPEN J Parenter Enteral Nutr 2014;38:334-77. [Crossref] [PubMed]
- Boullata JI, Mirtallo JM, Sacks GS, et al. Parenteral nutrition compatibility and stability: A comprehensive review. JPEN J Parenter Enteral Nutr 2022;46:273-99. [Crossref] [PubMed]
- Kraft MD, Tucker AM, Durfee SM, et al. Parenteral Nutrition Prescribing and Order Review Safety Study: The Need for Pharmacist Intervention. Nutr Clin Pract 2021;36:480-8. [Crossref] [PubMed]
- Alazawi W, Pirmadjid N, Lahiri R, et al. Inflammatory and Immune Responses to Surgery and Their Clinical Impact. Ann Surg 2016;264:73-80. [Crossref] [PubMed]
- Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology 2015;123:1455-72. [Crossref] [PubMed]
- Weimann A, Braga M, Carli F, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr 2017;36:623-50. [Crossref] [PubMed]
- Horowitz M, Neeman E, Sharon E, et al. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol 2015;12:213-26. [Crossref] [PubMed]
- Gustafsson UO, Oppelstrup H, Thorell A, et al. Adherence to the ERAS protocol is Associated with 5-Year Survival After Colorectal Cancer Surgery: A Retrospective Cohort Study. World J Surg 2016;40:1741-7. [Crossref] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Varnes BE, Singh V, May CC. Management of warfarin-associated intracerebral hemorrhage before and after implementation of an order set and prospective pharmacist order verification. J Thromb Thrombolysis 2021;52:239-47. [Crossref] [PubMed]
- da Silva LM, Lima HO, Ferrer R, et al. Comparison of strategies for adherence to venous thromboembolism prophylaxis in high-risk surgical patients: a before and after intervention study. BMJ Open Qual 2021;10:e001583. [Crossref] [PubMed]
- Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr 2017;36:11-48. [Crossref] [PubMed]
- August DA, Huhmann MBAmerican Society for Parenteral and Enteral Nutrition. (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr 2009;33:472-500. [Crossref] [PubMed]
- Kondrup J, Rasmussen HH, Hamberg O, et al. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003;22:321-36. [Crossref] [PubMed]
- Bekhit OE, Yousef RM, Abdelrasol HA, et al. Serum Albumin Level as a Predictor of Outcome in Patients Admitted to Pediatric Intensive Care Units. Pediatr Emerg Care 2021;37:e855-60. [Crossref] [PubMed]
- Yu KH, Ozer M, Cockrum P, et al. Real-world prognostic factors for survival among treated patients with metastatic pancreatic ductal adenocarcinoma. Cancer Med 2021;10:8934-43. [Crossref] [PubMed]
- Zengin A, Bag YM, Aydin MC, et al. Is Prognostic Nutritional Index an Indicator for Postoperative 90-Day Mortality in Laparoscopic Gastric Cancer Surgery? Nutr Cancer 2021; [Epub ahead of print]. [Crossref] [PubMed]
- Kinoshita F, Tagawa T, Yamashita T, et al. Prognostic value of postoperative decrease in serum albumin on surgically resected early-stage non-small cell lung carcinoma: A multicenter retrospective study. PLoS One 2021;16:e0256894. [Crossref] [PubMed]
- Wang P, Chen X, Liu Q, et al. Good performance of the Global Leadership Initiative on Malnutrition criteria for diagnosing and classifying malnutrition in people with esophageal cancer undergoing esophagectomy. Nutrition 2021;91-92:111420. [Crossref] [PubMed]
- Xiu S, Sun L, Mu Z, et al. Low prealbumin levels are associated with sarcopenia in older men with type 2 diabetes mellitus: A cross-sectional study. Nutrition 2021;91-92:111415. [Crossref] [PubMed]
- Fan Y, Sun Y, Man C, et al. Preoperative Serum Prealbumin Level and Adverse Prognosis in Patients With Hepatocellular Carcinoma After Hepatectomy: A Meta-Analysis. Front Oncol 2021;11:775425. [Crossref] [PubMed]
- Hemdan A, Abo-Samra M, Moneir W, et al. Nutritional predictors of pharyngocutaneous fistula after total laryngectomy: A multivariate analytic study in a single institution. Auris Nasus Larynx 2021; [Epub ahead of print]. [Crossref] [PubMed]
- Zhu M, Wei J, Chen W, et al. Nutritional Risk and Nutritional Status at Admission and Discharge among Chinese Hospitalized Patients: A Prospective, Nationwide, Multicenter Study. J Am Coll Nutr 2017;36:357-63. [Crossref] [PubMed]
(English Language Editor: J. Teoh)