
The relationship between polycystic ovary syndrome and infertility: a bibliometric analysis
Introduction
Polycystic ovary syndrome (PCOS) is a common hormonal disorder with the main features of hyperandrogenism, anovulation, and polycystic ovaries (1,2). The specific clinical manifestations vary greatly between individuals (3,4). Patients with PCOS are prone to menstrual disorders, infertility, insulin resistance (IR), and metabolic disorders, and a propensity experience to varying degrees of psychological problems and decreased quality of life (5-8). Infertile patients with polycystic ovary syndrome are often characterized with ovulation disorders (9). Women with PCOS are at risk of maternal, fetal, and neonatal complications (10). At present, the cause of PCOS is not very clear (11,12). The prevalence of PCOS varies slightly among countries in the world (2). The results of epidemiological surveys in the United States and other countries have shown that according to the 1990 National Institutes of Health (NIH) standard, the prevalence of PCOS in women of childbearing age is 4.0–8%, and according to the 2003 Rotterdam standard, the true prevalence of PCOS might be even higher (13,14). The prevalence of PCOS among women of childbearing age in mainland China has been approximated at 5.61%, although there may be some differences in the results of local epidemiological surveys in various provinces and cities (15,16). There have been relatively few studies on the global prevalence of PCOS in adolescent women (17). According to the 1990 NIH standard, the prevalence of PCOS in adolescence outside of China was 1.14–3.00%; according to the Rotterdam standard, it was 8.3–9.13%. According to the Rotterdam standard, PCOS can be divided into 4 types: type A, oligo − and/or anovulation + hyperandrogenism + polycystic ovary; type B, oligo − and/or anovulation + polycystic ovary; type C, hyperandrogenism + polycystic ovary; type D, oligo − and/or anovulation + hyperandrogenism (18,19). Women’s fertility can be adversely affected by PCOS, as follows: infrequent ovulation or anovulation, increasing the risk of spontaneous abortion, reducing the quality of oocytes, insulin resistance leading to hyperinsulinemia and increasing the risk of miscarriage, and prolonged intimal hyperplasia, which is harmful for implantation (20). In their study, Zhao et al. found that among 1,208 infertile female patients, the incidence of PCOS was 7.9% (21). Bibliometrics analysis provides an overview on research status of specific topic and help investigators to better understand the current related problems. In order to further understand the current status of research on polycystic ovaries and infertility, this study applied the method of bibliometric (22) analysis to major international medical citation databases, discussed the problems existing in the research in this field, and provided references for future research.
Methods
Literature retrieval
This study referred to the general internationally accepted method of bibliometrics, and retrieved literature based on the Science Citation Index Expanded (SCI-E) database, since it was the most common database for bibliometrics analysis. The search time was from database inception to 21 September 2021. The retrieval method was subject term searching, with “polycystic ovary syndrome” and “infertility” as the search terms, and the operation method was “AND”.
Analysis method
After obtaining the search results, we exported all the records of the search results and the cited records in plain text format to generate source files for analysis, and then analyzed the source files with CiteSpace software (Chaomei Chen, 2004–2021; http://cluster.cis.drexel.edu/~cchen/citespace/). The content of the analysis included: annual changes in the number of publications, distribution of the countries and institutions of the authors of the literature, the distribution of the journals from which the articles were published, the distribution of authors, and the use of keywords.
Statistical analysis
This study was a descriptive study, using quantity and percentage to describe each indicator. Excel 2019 (Microsoft, USA) software was used to conduct data analysis and generate statistical figures.
Results
Search results
There were a total of 2,843 records in the search results, 127 of which were subsequently identified as duplicate records. After removal of the duplicates, the actual related research documents totaled 2,716 (Figure 1). Among them, 2,021 were original articles, 568 were reviews, 87 were proceeding papers, 68 were editorial materials, 27 were publications priority, 26 were conference abstracts, 22 were letters, 12 were book chapters, 6 were corrections, 2 were notes, 2 were reprints, 1 was a news item, and 1 was a retraction (note: some documents were classified twice, so the sum of these classified data was consistent with Figure 1). The number of these documents roughly showed an increasing annual trend (Figure 2, Table S1). The citation frequency of these documents totaled 86,817, with an average citation number of 31.97 per article, and an h-index of 126 (Figure 3).

Analysis of author country of origin
The analysis showed that the authors of these articles came from 105 countries, and the top 5 countries of origin of the authors were: the United States, China, the United Kingdom, Italy, and Australia (Figure 4). CiteSpace V software was used to analyze the source files and generate a country visualization map (Figure 5). There were 2 countries which appeared in a document 682 times concurrently, that is, both countries cooperated 682 times (Figure 5). The top 5 centrally ranked countries were the United States, the United Kingdom, France, Australia, and Canada (Table 1, Figure 5).
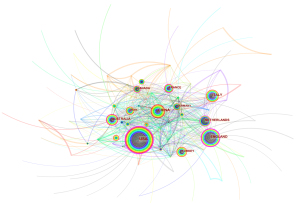
Table 1
| Rank | Countries | Centrality |
|---|---|---|
| 1 | USA | 0.36 |
| 2 | England | 0.30 |
| 3 | France | 0.18 |
| 4 | Australia | 0.15 |
| 5 | Canada | 0.12 |
| 6 | Netherlands | 0.11 |
| 7 | Sweden | 0.10 |
| 8 | Italy | 0.08 |
| 9 | China | 0.07 |
| 10 | Germany | 0.07 |
Institutional analysis of literature sources
We used CiteSpace V software to analyze the source files and generate a visualization map of the institutions (Figure 6). The analysis results showed that there were 502 institutions involved in these documents, and any 2 institutions had appeared in a document 1,068 times at the same time, that is, the cooperative relationship between the institutions has reached 1,068 times (Figure 6). The University of Adelaide from Australia had published the most literature on this topic. Ranked by centrality, the institution with the most cooperation was also the University of Adelaide. It can be seen from Tables 2,3 that the institutions with most publications and cooperation were mainly from the United States, Australia, and China.

Table 2
| Rank | Institutions | Publications |
|---|---|---|
| 1 | University of Adelaide | 62 |
| 2 | Monash University | 52 |
| 3 | University of Pennsylvania | 47 |
| 4 | Yale University | 42 |
| 5 | Pennsylvania State University | 42 |
| 6 | University of Michigan | 32 |
| 7 | Pennsylvania State College of Medicine | 30 |
| 8 | Shanghai Jiao Tong Univ | 30 |
| 9 | Heilongjiang University of Chinese Medicine | 24 |
| 10 | Virginia Commonwealth University | 24 |
Table 3
| Rank | Institutions | Centrality |
|---|---|---|
| 1 | University of Adelaide | 0.11 |
| 2 | Pennsylvania State University | 0.05 |
| 3 | University of Pennsylvania | 0.04 |
| 4 | Virginia Commonwealth University | 0.04 |
| 5 | Yale University | 0.03 |
| 6 | Pennsylvania State College of Medicine | 0.03 |
| 7 | Monash University | 0.02 |
| 8 | Heilongjiang University of Chinese Medicine | 0.02 |
Author analysis
We used CiteSpace V software to analyze the source files and generate the author visualization map (Figure 7). The results showed that some authors have published a large number of papers in this field (Table 4). Many authors have collaborated with researchers from other institutions many times while cooperating with researchers in their own institutions (Figure 7). From Table 4, Figure 7 and Table 5, we can see that Legro not only published the most documents, but also collaborated with other researchers the most frequently. Although the Chinese author Zhang has published a large number of documents, he did not have high centrality score, suggesting that Zhang had cooperated less with other authors.

Table 4
| Rank | Authors | Literatures |
|---|---|---|
| 1 | Legro RS | 69 |
| 2 | Zhang HP | 35 |
| 3 | Diamond MP | 28 |
| 4 | Fauser B | 26 |
| 5 | Coutifaris C | 22 |
| 6 | Santoro N | 21 |
| 7 | Franks S | 20 |
| 8 | Eisenberg E | 16 |
| 9 | Norman RJ | 14 |
| 10 | Homburg R | 14 |
Table 5
| Rank | Authors | Centrality |
|---|---|---|
| 1 | Legro RS | 0.09 |
| 2 | Wijeyeratne CN | 0.08 |
| 3 | Franks S | 0.04 |
| 4 | Norman RJ | 0.04 |
| 5 | Fauser BCJM | 0.03 |
| 6 | Balen A | 0.03 |
| 7 | Homburg R | 0.02 |
| 8 | Palomba S | 0.02 |
| 9 | Nestler JE | 0.02 |
Journal distribution
The papers included in this study were from 618 journals. The 2 journals with the most publications were Fertility and Sterility (284 papers) and Human Reproduction (209 papers), both of which are top journals in reproductive medicine. The top 10 journals according to the number of publications are shown in Table 6. However, the top comprehensive journals, Journal of the American Medical Association (JAMA) and Journal of Endocrinology, had the highest centrality scores, suggesting that more important related literature has been published in these journals (Table 7).
Table 6
| Journals | Records | % of 2,716 |
|---|---|---|
| Fertility and Sterility | 284 | 10.46 |
| Human Reproduction | 209 | 7.70 |
| Gynecological Endocrinology | 114 | 4.20 |
| Journal of Clinical Endocrinology Metabolism | 90 | 3.31 |
| Reproductive Biomedicine Online | 62 | 2.28 |
| Human Reproduction Update | 51 | 1.88 |
| European Journal of Obstetrics Gynecology and Reproductive Biology | 42 | 1.55 |
| Journal Of Assisted Reproduction and Genetics | 42 | 1.55 |
| Archives Of Gynecology and Obstetrics | 38 | 1.40 |
| Journal Of Reproductive Medicine | 34 | 1.25 |
Table 7
| Rank | Journals | Centrality |
|---|---|---|
| 1 | J Am Med Assoc | 0.07 |
| 2 | J Endocrinol | 0.06 |
| 3 | Horm Res | 0.06 |
| 4 | Nature | 0.05 |
| 5 | J Reprod Med | 0.05 |
| 6 | Int J Obesity | 0.05 |
| 7 | Am J Epidemiol | 0.05 |
| 8 | Am J Clin Nutr | 0.05 |
| 9 | Horm Metab Res | 0.05 |
| 10 | Ann Intern Med | 0.05 |
Keyword analysis
We used CiteSpace V software to analyze the source files and generate a keyword co-occurrence map (Figure 8). The results showed that a total of 511 keywords were used in the documents retrieved in this study. The number of occurrences of any 2 keywords in the same article at the same time was 2,117 times (Tables 8,9). In addition to keywords closely related to the subject of this research, keywords such as insulin resistance and metformin were also used more often. Burst detection was performed on keywords that were frequently used. The results revealed that the use of popular keywords has undergone obvious annual changes (Figure 9). In recent years, the more popular keywords included meta-analysis, follicular fluid, oxidative stress, and diagnostic criteria.
Table 8
| Rank | Keywords | Frequency |
|---|---|---|
| 1 | Polycystic ovary syndrome | 1503 |
| 2 | Infertility | 932 |
| 3 | Women | 890 |
| 4 | Insulin resistance | 563 |
| 5 | PCO | 472 |
| 6 | Prevalence | 316 |
| 7 | Obesity | 312 |
| 8 | Metformin | 296 |
| 9 | Ovulation induction | 288 |
| 10 | In vitro fertilization | 286 |
Table 9
| Rank | Keywords | Centrality |
|---|---|---|
| 1 | Follicle stimulating hormone | 0.11 |
| 2 | Gonadotropin | 0.10 |
| 3 | Hirsutism | 0.09 |
| 4 | Insulin resistance | 0.08 |
| 5 | Ovulation induction | 0.08 |
| 6 | Double blind | 0.08 |
| 7 | In vitro fertilization | 0.07 |
| 8 | Ovulation | 0.07 |
| 9 | Granulosa cell | 0.07 |
| 10 | Obese women | 0.07 |
Discussion
The results of this study showed that in the field where the subject involves both PCOS and infertility, the number of published documents and their citation frequency have shown an annually increasing trend. Researchers in the United States have published the most documents and conducted the most collaborations. However, among institutions, the University of Adelaide in Australia has published the most documents and cooperated most often. Among the authors, Legro from the University of Pennsylvania in the United States has published the most documents and participated most in cooperative efforts. In terms of journals, focused on top journals, comprehensive journals, and endocrinology journals in the field of reproduction. Keyword analysis showed that the focus of research in this field has changed in recent years, and insulin resistance and metformin have also been the focus of research.
The main clinical problem of PCOS is the imbalance of hormone levels, which leads to irregular menstrual cycle and anovulation, which affects fertility. It is the most common cause of anovulation in infertility. Progression of PCOS can be complicated by diabetes, obesity, and increased cholesterol, which will eventually lead to multi-system and multi-organ involvement. Some countries have issued relevant diagnosis and treatment guidelines regarding PCOS (23). There is also some expert consensus on the treatment of PCOS-related infertility. First of all, lifestyle adjustment has become a consensus in the treatment of PCOS and has been recommended by various guidelines. Studies have found that if overweight and obese PCOS patients lose 5–10% of their weight, their fertility would significantly improve, along with metabolic indicators and psychological status (24,25). In a recent meta-analysis, the author concluded that lifestyle intervention can improve free androgen index (FAI), weight, and body mass index (BMI) in women with PCOS, but the effect of lifestyle intervention on glucose tolerance remained unclear. We did not locate any high-quality in-depth studies on the impact of lifestyle interventions on live birth, miscarriage, or menstrual patterns (25). After active lifestyle adjustment, patients who have not resumed ovulation can be treated with ovulation-stimulating drugs. Commonly used drugs are letrozole (26), clomiphene (27), and metformin (28). Studies have shown that letrozole monotherapy may be better than clomiphene monotherapy (26); however, the combination of these drugs may be better than single-agent therapy (27). Gonadotropin (29) and laparoscopic ovarian drilling (LOD) are second-line treatments for PCOS (30,31) and used for patients with poor treatment effect of letrozole and clomiphene and other treatment difficulties. A recent meta-analysis found that compared with drugs alone to induce ovulation, laparoscopic ovarian drilling might reduce the rate of live births in women with anovulatory PCOS and clomiphene citrate (CC) resistance, regardless of whether they were combined with drugs to promote ovulation (31). Traditional Chinese medicine and acupuncture may also have certain therapeutic effects on PCOS, but more randomized controlled trials (RCTs) are needed for validation (32-35). When none of the above treatments can achieve satisfactory results, or the patient has other problems, assisted reproduction can be considered (36). There are 2 main types of assisted reproductive technology, intrauterine insemination (IUI) (37) and in vitro fertilization-embryo transfer (IVF-ET) (38,39). The clinical pregnancy rate and live birth rate of PCOS patients receiving IVF are similar to those of non-PCOS patients (40). However, metformin may not improve the clinical pregnancy rate and live birth rate after IVF-ET (41).
From our research results, we can deduce that the annual changes in commonly used keywords reflect changes in the focus of research in this field. Among them, medical treatment and IVF have received more attention. At the same time, rigorously designed double-blind clinical studies have also been the focus in recent years. In-depth analysis of the included literature shows that current clinical studies mainly focus on the comparison of the efficacy of first-line drugs, evaluation of the effects and safety of multi-drug combination therapy, and the application of artificial assisted reproductive technology in PCOS patients. When we analyzed the literature, we also noticed that the role of some auxiliary drugs has gradually come into focus, including drugs such as statins and resveratrol, which can improve patients' metabolic indicators and improve hormone levels (42).
Our analysis showed that in the research on PCOS-related infertility, the majority of key results come from the United States, United Kingdom, Australia, and other countries, and most of the institutions with more research results were from the United States. This suggested that the research has not been balanced between districts and countries, especially for developing countries and regions. In fact, PCOS is as common in developing countries, causing a series of psychological and social problems for affected patients (43,44). Therefore, we believe that in future there will be more international cooperation, especially multi-center clinical research and epidemiological research involving developing countries.
The limitations of this study were as follows: due to the diversity of keywords and subject terms used in the literature, it was difficult to accurately retrieve all the literature in this field. Part of the literature did not specify whether RCT is in the keywords or subject terms, which makes it impossible for us to accurately analyze the development of RCTs. To address this problem, future research should adopt the methods of systematic review and meta-analysis to conduct a comprehensive analysis of RCT research in this field.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-714/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Goodarzi MO, Dumesic DA, Chazenbalk G, et al. Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nat Rev Endocrinol 2011;7:219-31. [Crossref] [PubMed]
- Lizneva D, Suturina L, Walker W, et al. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril 2016;106:6-15. [Crossref] [PubMed]
- McCartney CR, Marshall JC. CLINICAL PRACTICE. Polycystic Ovary Syndrome. N Engl J Med 2016;375:54-64. [Crossref] [PubMed]
- Ortiz-Flores AE, Luque-Ramírez M, Escobar-Morreale HF. Polycystic ovary syndrome in adult women. Med Clin (Barc) 2019;152:450-7. [Crossref] [PubMed]
- Rosenfield RL. Current concepts of polycystic ovary syndrome pathogenesis. Curr Opin Pediatr 2020;32:698-706. [Crossref] [PubMed]
- Louwers YV, Laven JSE. Characteristics of polycystic ovary syndrome throughout life. Ther Adv Reprod Health 2020;14:2633494120911038. [Crossref] [PubMed]
- Pfieffer ML. Polycystic ovary syndrome: An update. Nursing 2019;49:34-40. [Crossref] [PubMed]
- Cooney LG, Dokras A. Depression and Anxiety in Polycystic Ovary Syndrome: Etiology and Treatment. Curr Psychiatry Rep 2017;19:83. [Crossref] [PubMed]
- Hanson B, Johnstone E, Dorais J, et al. Female infertility, infertility-associated diagnoses, and comorbidities: a review. J Assist Reprod Genet 2017;34:167-77. [Crossref] [PubMed]
- Bergh CM, Moore M, Gundell C. Evidence-Based Management of Infertility in Women With Polycystic Ovary Syndrome. J Obstet Gynecol Neonatal Nurs 2016;45:111-22. [Crossref] [PubMed]
- Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol 2018;14:270-84. [Crossref] [PubMed]
- Dasgupta S, Reddy BM. Present status of understanding on the genetic etiology of polycystic ovary syndrome. J Postgrad Med 2008;54:115-25. [Crossref] [PubMed]
- Dumesic DA, Oberfield SE, Stener-Victorin E, et al. Scientific Statement on the Diagnostic Criteria, Epidemiology, Pathophysiology, and Molecular Genetics of Polycystic Ovary Syndrome. Endocr Rev 2015;36:487-525. [Crossref] [PubMed]
- Belenkaia LV, Lazareva LM, Walker W, et al. Criteria, phenotypes and prevalence of polycystic ovary syndrome. Minerva Ginecol 2019;71:211-23. [Crossref] [PubMed]
- Wang T, Fu H, Chen L, et al. Pregnancy complications among women with polycystic ovary syndrome in China: a Meta-analysis. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2017;42:1300-10. [PubMed]
- Chen ZJ, Shi Y. Polycystic ovary syndrome. Front Med China 2010;4:280-4. [Crossref] [PubMed]
- Rothenberg SS, Beverley R, Barnard E, et al. Polycystic ovary syndrome in adolescents. Best Pract Res Clin Obstet Gynaecol 2018;48:103-14. [Crossref] [PubMed]
- Dabadghao P. Polycystic ovary syndrome in adolescents. Best Pract Res Clin Endocrinol Metab 2019;33:101272. [Crossref] [PubMed]
- Kostopoulou E, Anagnostis P, Bosdou JK, et al. Polycystic ovary Syndrome in Adolescents: Pitfalls in Diagnosis and Management. Curr Obes Rep 2020;9:193-203. [Crossref] [PubMed]
- Costello MF, Misso ML, Balen A, et al. A brief update on the evidence supporting the treatment of infertility in polycystic ovary syndrome. Aust N Z J Obstet Gynaecol 2019;59:867-73. [Crossref] [PubMed]
- Zhao J, Fan J, Wang X. Study on the prevalence and clinical characteristics of polycystic ovary syndrome in female infertile patients. J Prac Gyneco Endocrino 2019;6:137-8.
- Cooper ID. Bibliometrics basics. J Med Libr Assoc 2015;103:217-8. [Crossref] [PubMed]
- Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2013;98:4565-92. [Crossref] [PubMed]
- Faghfoori Z, Fazelian S, Shadnoush M, et al. Nutritional management in women with polycystic ovary syndrome: A review study. Diabetes Metab Syndr 2017;11:S429-32. [Crossref] [PubMed]
- Lim SS, Hutchison SK, Van Ryswyk E, et al. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev 2019;3:CD007506. [Crossref] [PubMed]
- Bansal S, Goyal M, Sharma C, et al. Letrozole versus clomiphene citrate for ovulation induction in anovulatory women with polycystic ovarian syndrome: A randomized controlled trial. Int J Gynaecol Obstet 2021;152:345-50. [Crossref] [PubMed]
- Mejia RB, Summers KM, Kresowik JD, et al. A randomized controlled trial of combination letrozole and clomiphene citrate or letrozole alone for ovulation induction in women with polycystic ovary syndrome. Fertil Steril 2019;111:571-578.e1. [Crossref] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline. Fertil Steril 2017;108:426-41. [Crossref]
- Morgante G, Massaro MG, Di Sabatino A, et al. Therapeutic approach for metabolic disorders and infertility in women with PCOS. Gynecol Endocrinol 2018;34:4-9. [Crossref] [PubMed]
- Senturk S, Celik O, Dalkilic S, et al. Laparoscopic Ovarian Drilling Improves Endometrial Homeobox Gene Expression in PCOS. Reprod Sci 2020;27:675-80. [Crossref] [PubMed]
- Bordewijk EM, Ng KYB, Rakic L, et al. Laparoscopic ovarian drilling for ovulation induction in women with anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev 2020;2:CD001122. [Crossref] [PubMed]
- Chen H, Lim CED. The efficacy of using acupuncture in managing polycystic ovarian syndrome. Curr Opin Obstet Gynecol 2019;31:428-32. [Crossref] [PubMed]
- Moini Jazani A, Nasimi Doost Azgomi H, Nasimi Doost Azgomi A, et al. A comprehensive review of clinical studies with herbal medicine on polycystic ovary syndrome (PCOS). Daru 2019;27:863-77. [Crossref] [PubMed]
- Ried K. Chinese herbal medicine for female infertility: an updated meta-analysis. Complement Ther Med 2015;23:116-28. [Crossref] [PubMed]
- Ma QW, Tan Y. Effectiveness of co-treatment with traditional Chinese medicine and letrozole for polycystic ovary syndrome: a meta-analysis. J Integr Med 2017;15:95-101. [Crossref] [PubMed]
- Kollmann M, Martins WP, Lima ML, et al. Strategies for improving outcome of assisted reproduction in women with polycystic ovary syndrome: systematic review and meta-analysis. Ultrasound Obstet Gynecol 2016;48:709-18. [Crossref] [PubMed]
- Huang S, Du X, Wang R, et al. Ovulation induction and intrauterine insemination in infertile women with polycystic ovary syndrome: A comparison of drugs. Eur J Obstet Gynecol Reprod Biol 2018;231:117-21. [Crossref] [PubMed]
- Tan X, Wen Y, Chen H, et al. Follicular output rate tends to improve clinical pregnancy outcomes in patients with polycystic ovary syndrome undergoing in vitro fertilization-embryo transfer treatment. J Int Med Res 2019;47:5146-54. [Crossref] [PubMed]
- Alcalay M, Bider D, Lipitz S, et al. Polycystic ovarian syndrome: pregnancy outcome following in vitro fertilization-embryo transfer. Gynecol Endocrinol 1995;9:119-23. [Crossref] [PubMed]
- Gadalla MA, Norman RJ, Tay CT, et al. Medical and Surgical Treatment of Reproductive Outcomes in Polycystic Ovary Syndrome: An Overview of Systematic Reviews. Int J Fertil Steril 2020;13:257-70. [PubMed]
- Wu Y, Tu M, Huang Y, et al. Association of Metformin With Pregnancy Outcomes in Women With Polycystic Ovarian Syndrome Undergoing In Vitro Fertilization: A Systematic Review and Meta-analysis. JAMA Netw Open 2020;3:e2011995. [Crossref] [PubMed]
- Banaszewska B, Pawelczyk L, Spaczynski R. Current and future aspects of several adjunctive treatment strategies in polycystic ovary syndrome. Reprod Biol 2019;19:309-15. [Crossref] [PubMed]
- Advani K, Batra M, Tajpuriya S, et al. Efficacy of combination therapy of inositols, antioxidants and vitamins in obese and non-obese women with polycystic ovary syndrome: an observational study. J Obstet Gynaecol 2020;40:96-101. [Crossref] [PubMed]
- Buddhavarapu S. Bearding, Balding and Infertile: Polycystic Ovary Syndrome (PCOS) and Nationalist Discourse in India. J Med Humanit 2020;41:411-27. [Crossref] [PubMed]







