Postmenopausal vaginal bleeding as initial presentation of gastric cancer: a case report with literature review of prognostic factors and treatment of krukenberg tumor
Introduction
Krukenberg tumor (KT) is a rare metastatic adenocarcinoma of the ovary, which constitutes 1–2% of all ovarian neoplasms and can be confused with adnexal masses such as teratomas, primary ovarian malignancies or complex cysts. According to the new diagnostic criteria, a mucin secreting signet ring cell cancer (SRCC) in the dense fibroblastic stroma of the ovary is referred as a KT. Rarely, metastatic ovarian tumors are found before the primary site is diagnosed—as in our case. Tumor (T) stage of the primary carcinoma is the most important predictor of KT.
Case presentation
A 68-year-old Haitian female with past medical history of diabetes mellitus, hypertension and coronary artery disease, who presented with complaints of intermittent postmenopausal vaginal bleeding and fatigue of 3–4 months duration. She has no history of abdominal pain, fever, chills, night sweats, nausea, vomiting, weight loss, change in appetite or bowel habits. She denied any history of smoking, alcohol or drug abuse and has no known family history of malignancy.
She had no ascites, hepatosplenomegaly, lymphadenopathy or palpable mass on abdominal examination. On bimanual pelvic examination, left sided adnexal mass was felt. The rest of the physical examination was within normal limits.
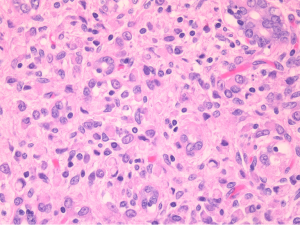
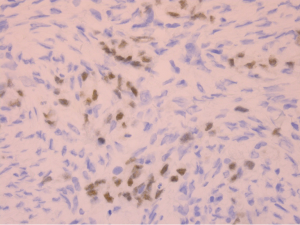
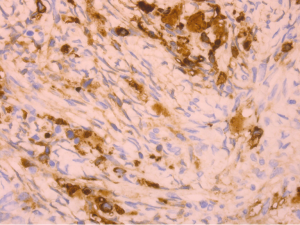
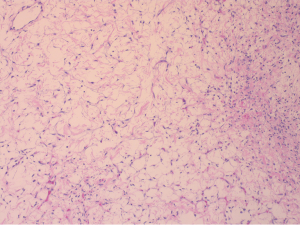
On laboratory results, hemoglobin was 12.5, hematocrit 40, CA-125 within normal limits. Ultrasound of abdomen and pelvis showed large left sided pelvic mass. She underwent TAH/BSO and was found to have significantly enlarged left ovary with large mass. Histopathology showed multiple uterine leiomyoma (largest of which was 1.0 cm), weakly proliferative endometrium, fibrothecoma of left ovary and a small focus of metastatic signet ring cell adenocarcinoma was seen in the left ovary (Figure 1). Immunohistochemistry (IHC) was positive for CK7 (Figure 2) and CDX2 (Figure 3).
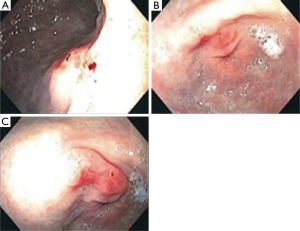
The morphology of tumor cells in conjunction with IHC staining pattern was consistent with metastatic signet ring cell adenocarcinoma of gastric origin. With the suspicious diagnosis of ovarian metastatic adenocarcinoma (KT) of gastric origin, upper gastrointestinal endoscopy was done, which showed moderate gastritis and small ulcer in the antrum (Figure 4). Multiple biopsies were taken and antral biopsy was suggestive of undifferentiated signet cell adenocarcinoma (Figure 5). Colonoscopy was normal. CT scan of chest, abdomen and pelvis with contrast did not show any evidence of metastatic disease. Patient underwent laparoscopic subtotal gastrectomy with Roux-en-Y gastrojejunostomy and partial omentectomy.
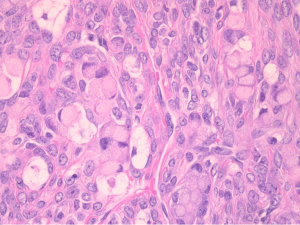
Pathology showed grade IV poorly differentiated signet ring cell adenocarcinoma (Figure 6) with a tumor size of 0.6 cm, only involving the mucosa. Proximal, radial and distal margins were negative. Lymphovascular and perineural invasion was not seen. Seven lymph nodes were negative for metastasis. The diagnosis was stage IV gastric adenocarcinoma (pT1a, pN0, pM1). PET/CT did not show any evidence of metastasis. The patient received 4 cycles of adjuvant chemotherapy (docetaxel, cisplatin and 5-fluorouracil). She is under surveillance now and doing well.
Discussion
KT is a rare metastatic adenocarcinoma of the ovary, which constitutes 1–2% of all ovarian neoplasms and can be confused with adnexal masses such as teratomas, primary ovarian malignancies or complex cysts (1). It is a late stage disease with very poor prognosis and median overall survival (mOS) of only 14 months (2).
Route of metastasis is still unproven; it could be lymphatic, hematogenous or peritoneal seeding. Most common primary site is stomach (70–80%), followed by colon (10–20%)—although occasionally breast, biliary tract, pancreas, appendix, kidneys or lungs are the primary sites. Patients often present with abdominal pain, bloating, ascites, nausea, vomiting, and poor appetite and weight loss. Patients with KT rarely present with vaginal bleeding (as in our case), hirsutism and virilization, which are caused by hormonal overproduction due to reaction of ovarian stroma caused by tumor cells (3,4).
Stromal involvement, mucin producing neoplastic signet ring cells and ovarian stromal sarcomatoid proliferation on histopathology is required for diagnosis of KT. Most KTs are diagnosed metachronously and few synchronously. Bilateral ovarian involvement is present in almost 80% of cases; if unilateral, it is more common on right side as compared to left. KT of colorectal origin has more frequent unilateral presentation. Metastatic ovarian tumor from colon is more difficult to differentiate than other primary sites. The median age of diagnosis is 45, almost 10 years younger than primary ovarian cancer.
Treatment guidelines are insufficient and the optimal treatment for KTs has not been established because of the rarity of this entity. Surgical resection of metastasis can possibly improve the outcome if primary lesion is amenable to surgical resection. Li and colleagues analyzed the prognostic factors and effects of metastasectomy in 133 patients with KTs of gastric origin (5). Gastrectomy and the absence of ascites were two independent risk factors associated with longer survival. mOS was 19 months compared to 9 months with and without gastrectomy and 13 vs. 21 months with and without ascites, respectively. Survival of patients who underwent both metastasectomy and gastrectomy was longer than the patients who underwent metastasectomy only (21 vs. 9 months). Survival is poor if original tumor cannot be resected. Patients without ascites and with resectable primary gastric lesion possibly can benefit from surgical resection of primary tumor and metastasectomy. This study also analyzed the association between cancer stem cells related protein expression of metastatic tumor and mOS. The positive expression of CD44, CD13, and SOX2 correlated with poor survival.
Another study by Cho and colleagues showed survival benefit of ovarian metastasectomy in synchronous or metachronous KT (6). They analysed 125 patients with stage IV gastric cancer with KT and 91 patients with recurrent KT after they underwent curative resection of gastric cancer. It showed that patients with KT of gastric origin who underwent chemotherapy plus metastasectomy had longer over survival than those who received chemotherapy alone, regardless of gastric cancer stage. R0 resection group had a significantly longer over all survival than R1/R2 resection (30 vs. 15 months).
Jeung and colleagues compared the median survival time of KTs of gastric versus colorectal origin (7). Median survival time was 22.7 months (19.2 vs. 27.3 months for KT of gastric and colorectal origin respectively). They also found significantly longer median survival time in metachronous cancer, post-menopausal women and with unilateral ovarian involvement compare to synchronous cancer, premenopausal women and bilateral ovarian involvement respectively.
KT is a rare entity with poor prognosis and treatment guidelines are insufficient. The best chance to increase patient survival is metastasectomy in surgical candidates followed by palliative chemotherapy in metachronous tumors and both resection of primary tumor and metastasectomy followed by palliative chemotherapy in synchronous tumors.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent has been obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Al-Agha OM, Nicastri AD. An in-depth look at Krukenberg tumor: an overview. Arch Pathol Lab Med 2006;130:1725-30. [PubMed]
- Young RH. From krukenberg to today: the ever present problems posed by metastatic tumors in the ovary: part I. Historical perspective, general principles, mucinous tumors including the krukenberg tumor. Adv Anat Pathol 2006;13:205-27. [PubMed]
- Kiyokawa T, Young RH, Scully RE. Krukenberg tumors of the ovary: a clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestations. Am J Surg Pathol 2006;30:277-99. [PubMed]
- Papakonstantinou E, Liapis A, Kairi-Vassilatou E, et al. Virilizing ovarian Krukenberg tumor in a 27-year-old pregnant woman. A case report and literature review. Eur J Gynaecol Oncol 2011;32:331-3. [PubMed]
- Li C, Kim S, Lai JF, et al. Advanced gastric carcinoma with signet ring cell histology. Oncology 2007;72:64-8. [PubMed]
- Cho JH, Lim JY, Choi AR, et al. Comparison of Surgery Plus Chemotherapy and Palliative Chemotherapy Alone for Advanced Gastric Cancer with Krukenberg Tumor. Cancer Res Treat 2015;47:697-705. [PubMed]
- Jeung YJ, Ok HJ, Kim WG, et al. Krukenberg tumors of gastric origin versus colorectal origin. Obstet Gynecol Sci 2015;58:32-9. [PubMed]