Diagnosis, disease stage, and distress of Chinese cancer patients
Introduction
As is known to all, cancer is a severe disease that does great harm to patients’ life. It can affect cancer patients not only physically, but also psychologically (1). Depress, anxiety and pessimism caused by cancer diagnosis might affect the quality of life in cancer patients (1-5). Therefore, some doctors and nurses might choose not to tell the truth to patients at the time of the diagnosis (6-15).
Many studies have focused on information needs of cancer patients with different cultural backgrounds (16-23). Cancer patients believed that doctor-in-charge was the appropriate person to inform the diagnosis. They also wanted to know the truth immediately after the diagnosis (18-20). Cancer patients also wanted to know a great deal of specific information concerning their illness. And today, more and more patients are being informed of their diagnosis and prognosis (21,22). These previous studies revealed the attitude of cancer patient toward truth telling, and many studies revealed the attitudes of doctors and migrant cancer patients toward disclosure (24-28). However, it is not clear how patient knows about the cancer diagnosis and whether patient knows enough information about the diagnosis (such as the disease stage). This issue needs to be investigated further more.
Psychosocial distress is common among cancer patients. Many surveys suggest that nearly half of adults with cancer experienced clinically significant levels of distress (29-31). To the best of our knowledge, little literature focused on distress of cancer patients who did not know enough information (such as the stage of illness) about their disease.
The present study focuses on this issue as followings: (I) how did patients know about their cancer diagnosis? (II) Was the cancer stage, which patient believed, true? (III) Distress of cancer patients who did not know enough information (such as the stage of illness) about their disease.
Methods
Participants
This study was processed in a university hospital with more than 4,200 patient beds (474 beds in cancer center). All the participants were in-patients of oncology department, and knew their cancer diagnosis. To be eligible for the study, subjects needed to be 18 years or older, agree to participate in this study by signing on the informed consent document, well enough to fill out a questionnaire themselves or communicate with the interviewer. Participants who did not complete their questionnaire for any reason were excluded.
Definition
For participants, according to the National Cancer Institute (NCI) dictionary of cancer terms (http://www.cancer.gov/dictionary), ‘advanced cancer’ is a term describing cancer that has spread to other places in the body and that usually cannot be cured or controlled with treatment. When data of the real disease stage was analyzed, we identified stage IV disease as ‘advanced cancer’, stage I–III disease as ‘non-advanced cancer’. Distress is a multi-factorial unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms and its treatment. Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis (http://www.nccn.org).
Methods and procedures
Questionnaires including single-item visual scale of Distress Thermometer (DT, http://www.nccn.org) were delivered to eligible inpatients. All participants were given necessary information about the details of how to fill out the questionnaire and asked not to share their information with others. During the investigation, participants would answer some questions about when and how they knew the cancer diagnosis and questions about their cancer stage. We provided answers for all questions in this questionnaire and participants could choose the ‘best one’ for each question. All answers and related information were inputted into computer. Then data were analyzed by an independent investigator. This study passed ethics review and was approved by Cancer Center of Sichuan University, China.
Materials
We constructed a questionnaire including information that was divided into three groups. The following demographic information was gathered by the questionnaires: gender, age, marriage, income, religion, occupation, and level of education. The following clinical information was also gathered: time since diagnosis, type of primary cancer, real disease stage, and Eastern Cooperative Oncology Group performance status (ECOG PS). Among them, information about type of primary cancer and real disease stage were filled out by the interviewer. In addition, the third group of information was obtained: (I) when did you know the cancer diagnosis? (II) How did you know the diagnosis? (III) Who knew the diagnosis first? (IV) Who did you hope to know the diagnosis first? (V) Did you suspect that your diagnosis was cancer before being informed? (VI) What was the cancer stage that you believed? We also added DT to the questionnaire to investigate distress of participants. Previous studies revealed that a DT cutoff score of 4 had optimal sensitivity and specificity (30,32), so our study also set the DT cutoff score at 4. All of these questions were closed and the whole questionnaire took about 15 minutes to complete.
Before administration, the questionnaire was pilot tested with 20 cancer patients, revising it for clarity and ease of comprehension.
Statistical analysis
Descriptive statistical analysis was used to summarize the participant’s demographic characteristics. Chi-square test was used to determine the significant difference in the answers between participants with non-advanced and advanced cancer. Univariate logistic regression analysis was used to measure the association between demographic/clinical information and the third group of information. For variables with significant association in univariate analysis, multivariate logistic regression analysis was used to estimate odds ratios (OR) and 95% confidence intervals (CI). All tests of statistical significance were two-tailed tests. We set the significance level at P<0.05. SPSS statistic software (Version 17.0) was used for data analysis.
Results
Sample characteristics
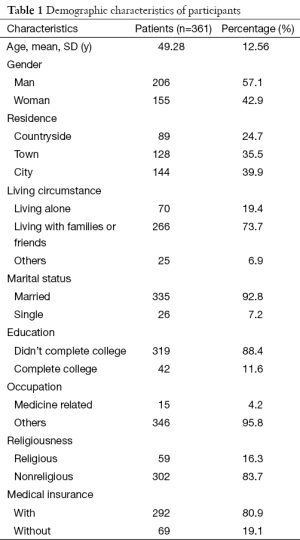
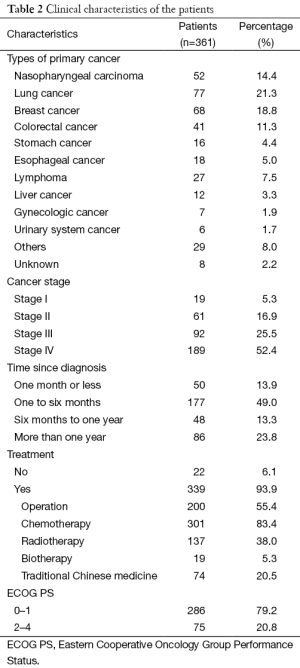
Four hundreds and twenty-two cancer patients were contacted, and 361 completed the questionnaire (effective responses rate, 85.5%). The most common reason given for nonparticipation was lack of time. The demographic information of participants is summarized in Table 1. The clinical information of patients is summarized in Table 2.
Full table
Full table
Details regarding how to learn the diagnosis
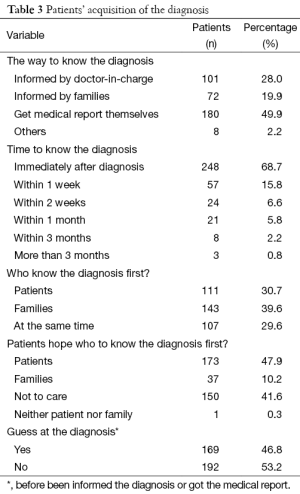
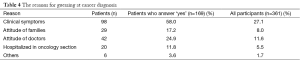
Nearly half of patients (180/361, 49.9%) reported that they got their medical reports themselves and knew the diagnosis. Most patients (68.7%) reported that they knew their cancer diagnosis immediately after the diagnosis. Only 30.7% cancer patients knew the diagnosis earlier than their family members. Nearly half of patients (47.9%) believed that they themselves should be informed of cancer diagnosis before their families. In addition, nearly half of participants (46.8%) had guessed at their cancer diagnosis before they were informed of the diagnosis or got the medical reports. Table 3 shows the details. The reasons for guessing at cancer diagnosis are summarized in Table 4.
Full table
Full table
Disease stage
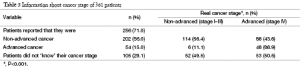
More than 70% patients reported that they knew their cancer stages (Table 5). However, the disease stage, which they believed, differed significantly from the real cancer stage (κ=0.291, P<0.001). Actually, only 44.9% of patients (162/361) knew their real disease stages.
Full table
Multivariate logistic regression analysis
Younger patients were more likely to know the diagnosis immediately after the diagnosis (OR, 0.972; 95% CI, 0.954–0.991, P=0.003). Patients living alone (OR, 0.543; 95% CI, 0.310–0.950; P=0.032) and with colorectal cancer (OR, 0.431; 95% CI, 0.216–0.858; P=0.017) were less likely to know the diagnosis immediately after the diagnosis.
Patients with ‘advanced cancer’ were also more likely to guess at their cancer diagnosis before being informed than patients with ‘non-advanced cancer’ (OR, 0.449; 95% CI, 0.244–0.861; P=0.015).
Patients with breast cancer (OR, 2.215; 95% CI, 1.279–3.836; P=0.005) and living in the countryside (OR, 1.915; 95% CI, 1.078–3.402; P=0.027) were more likely to know the diagnosis before their families. In addition, younger patients were more likely to wish to know the diagnosis before their families (OR, 0.977; 95% CI, 0.960–0.994; P=0.008).
Patients with stage I–III cancer were more likely to know their real disease stage than patients with stage IV cancer (OR, 6.628; 95% CI, 4.066–10.804; P<0.001). Patients living in city (OR, 2.920; 95% CI, 1.560–5.465; P=0.001) and woman patients (OR, 1.892; 95% CI, 1.072–3.338; P=0.028) were more likely to know the real cancer stage.
Relationship between cancer stage and distress of patients
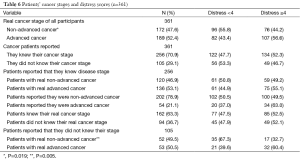
The details of the relationship between cancer stage and distress score were presented in Table 6. Distress scores of patients reporting that they knew their cancer stage was not significantly different from that of patients reporting that they knew nothing about their stage (OR 0.797; 95% CI, 0.505–1.256; P=0.328).
Full table
Among all participants involved in this study, patients with real advanced cancer were more likely to get higher distress score (≥4) than patients with real non-advanced cancer both in univariate logistic regression analysis (OR 1.648; 95% CI, 1.087–2.499; P=0.019) and in multivariate logistic regression analysis (OR 1.716; 95% CI 1.126–2.616; P=0.012).
Univariate logistic regression analysis revealed that, among participants who reported they knew nothing about their disease stage, real cancer stage was the only factor related to patient’s distress score. Those patients with real advanced cancer were more likely to get higher distress score (≥4) than patients with real non-advanced cancer (OR 3.137; 95% CI, 1.411-6.976; P=0.005).
Among patients who reported that they knew their disease stages, distress score of patient was not significantly related to patient’s real cancer stage (OR, 1.271; 95% CI, 0.777–2.080; P=0.339), the stage which patient reported (OR, 1.734; 95% CI, 0.935–3.215; P=0.081), and the fact whether they actually knew their real cancer stage (OR 0.986; 95% CI, 0.593–1.641; P=0.958).
Discussion
Recent studies suggest that patients with terminal illness must be told the truth—even in the most difficult situations in order to fully participate in their medical care (33). Our previous study, which focused on patients’ attitude toward disclosure, revealed that nearly 90% cancer patients wished to be informed of diagnosis immediately (20). This study observed that 68.7% cancer patients knew the diagnosis immediately after the diagnosis. In addition, 15.8% of the participants knew the truth within one week. Therefore, nearly 85% of participants knew their cancer diagnosis immediately/within one week (Table 3). This rate (85%) was very close to patients’ wish (90%) and obviously higher than data from a previous article published in 2002 (19). In that study, authors reported that 73% patients wished to be informed of diagnosis immediately/within one week, while only 50% patients had their wish fulfilled. This difference reflects in some degree that the situation of truth telling in China has changed remarkably during last ten years.
In this study, the median age of participants is nearly 49 years old (Table 1). It was observed that younger patients were more likely to know cancer diagnosis immediately (P=0.003). A Hispanic study also revealed that the vast majority preferred a shared or active decision-making process and wanted information about their diagnosis and prognosis. Older patients and those who wanted to know their diagnosis seemed to be more satisfied with the way treatment decisions were made (29). A similar phenomenon was also observed by an Italian study, which reported that the probability to be informed was higher for young patients (34). Physicians had reported that ‘poor understanding of the patient’ (13/27, 48%) and ‘family’s wish’ (8/27, 30%) were the major reasons for non-disclosure to elder patients (35). In China, elder patients went to hospital usually with the company of their children. And it was the duty of these ‘young’ family members to communicate with doctors. The role of the family in liaising between doctor and the patient was also emphasized by Chinese-Australians (28) and patients of other Asian culture, such as Japanese (28,34,36). We reported that only 78.0–92.2% Chinese family members believed that patients should be informed of cancer diagnosis immediately (20). Apart from that, we also observed that younger patients were more likely to wish to know the diagnosis before their families (P=0.008). Therefore, younger patients might be more ‘active’ during the process of diagnosis. Because of these factors, younger patients might be easier than their elder counterparts to know the facts immediately after diagnosis.
Our previous studies revealed that doctor-in-charge was the appropriate person to inform the diagnosis (20,24). However, this study observed that only 28.0% of the patients (101/361) were informed by doctors directly. Nearly half of the participants (180/361, 49.9%) got their medical reports themselves and knew the diagnosis. The remaining 72 (19.9%) patients were informed by their families (Table 3). A previous study, starting in another Chinese city, also revealed that 44.37% of cancer patients knew the diagnosis through medical records/reports (19). An American research of cancer patients revealed that most patients (96%) received their cancer diagnoses from physicians (37). Only less than 4% of patients were told by relatives. These results illuminated that different countries had significant difference in the way that cancer patients got the true diagnosis: almost all cancer patients from western countries were informed by health professionals, while most Chinese patients got the bad news from indirect approach. However, a Turkey research revealed that the understanding of the diagnosis indirectly may be stressful to the patient because it arouses suspicion about the cancer and treatment, and consequently can lead to psychiatric disturbance (3).
A previous study revealed that a majority of American patients, but only a minority of Japanese patients, agreed that a patient should be informed of cancer diagnosis before their family, from which we can observe that cultural varieties play a vital role in the need of disclosure among cancer patients (26). The present study observed that only 10.2% of the Chinese patients wished their family members to know the diagnosis before themselves. However, there was still 39.5% of the patients reported that their families knew the diagnosis first (Table 3). This result reflected the current situation of truth telling in China. Even today, it is still a problem for Chinese doctors to disclose cancer diagnosis to patient directly as a result of “family wish”. However, a Latin American research indicated that most cancer patients did not wish themselves to be prevented from knowing the truth by their families, and wanted to participate in the whole process of treatment decision (38).
Nearly half of the patients (169/361, 46.8%) became aware that they got cancer before disclosure. They were aware of cancer diagnosis because of ‘the clinical symptoms (98/169, 58.0%)’, and ‘the attitude of doctors/families (71/169, 42.1%) (Table 4). The patients with ‘advanced cancer’ were more likely to be aware of the diagnosis before disclosure (P=0.015). A previous study revealed that 48% of patients with gastrointestinal cancer speculated that they had cancer (1). Although non-informed, nearly 30% of the Italian participants were aware of cancer diagnosis (34). Another study also reported that a majority of patients (58.0%) were aware of their terminal status, and approximately 28% of patients guessed it from their worsening condition (39). Studies above revealed that cancer patients might be aware of their true diagnosis. This conjecture and scare of uncertain diagnosis may even have more negative affection to patients’ psychological state (40). Actually, patients who knew of their diagnosis had a lower rate of emotional distress and a higher quality of life (39). A study among elderly cancer patients also illustrated that informed patients refer better expectation than those not informed (17).
The participants included in our research were in-patients who already knew their cancer diagnosis. However, nearly one third of them (29.1%) knew nothing about their disease stage (Table 5). Among them, 50.5% (53/105) were stage IV cancer patients. Other participants (71.0%) believed that they knew the disease stages. However, the disease stage, which they believed, differed significantly from the real cancer stage (κ=0.291, P<0.001). Many patients with stage IV disease (88/136, 64.7%) didn’t consider themselves as ‘advanced cancer patients’ (Table 5). Actually, only 162 participants (44.9%) really knew their true disease stage in present study (Table 5). Patient with stage I–III cancer (P<0.001), patients living in city (P=0.001), and woman patients (P=0.028) was more likely to know the real disease stage.
A Latin American study revealed that distress scores are higher in patients with advanced cancer than those in patients with the disease under control (41). A similar phenomenon was also observed in this study (Table 6). Among all participants and participants who reported they knew nothing about their disease stage, patients with real advanced cancer were more likely to get higher distress score (≥4) than patients with real non-advanced cancer. However, distress scores of patients, who reported that they knew their disease stages, were not significantly related to the stages which patients reported, or the fact whether they actually knew their real cancer stage. Briefly, distress scores of cancer patients were determined by the real cancer stage, not the stage that patients believed. The most potential reason is that patients with advanced cancer usually suffer from more severe physical symptoms (42). As a result of high distress score in patients with advanced cancer, health professionals should pay more attention to these patients’ psychological status. Psychological support should be given to patients with advanced cancer, no matter whether they knew it or not.
Conclusions
In conclusion, our findings suggest that most of patients (68.7%) knew the bad news immediately after diagnosis of cancer. Half of patients knew their diagnosis directly from medical report. However, only 63.3% patients among them knew their real stages. Patients with advanced cancer were more likely to get a higher distress score. Distress scores of cancer patients were determined by the real cancer stage, not the stage that patients believed.
The limitations of this study were as follows: (I) the single institutional nature of this study is a limitation. However, this hospital, where we started our study, is one of the largest-scale hospitals in China. Patients of this hospital come from nearly all over the country; (II) nearly half of patients reported that they got their medical reports themselves and knew the diagnosis. However, this study did not distinguish how patients got their medical reports.
Acknowledgements
We thank all participants for their help. We also thank all the other doctors and nurses who helped us in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Montazeri A, Tavoli A, Mohagheghi MA, et al. Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer 2009;9:39. [PubMed]
- Lheureux M, Raherison C, Vernejoux JM, et al. Quality of life in lung cancer: does disclosure of the diagnosis have an impact? Lung Cancer 2004;43:175-82. [PubMed]
- Atesci FC, Baltalarli B, Oguzhanoglu NK, et al. Psychiatric morbidity among cancer patients and awareness of illness. Support Care Cancer 2004;12:161-7. [PubMed]
- Alexander PJ, Dinesh N, Vidyasagar MS. Psychiatric morbidity among cancer patients and its relationship with awareness of illness and expectations about treatment outcome. Acta Oncol 1993;32:623-6. [PubMed]
- Hyodo I, Eguchi K, Takigawa N, et al. Psychological impact of informed consent in hospitalized cancer patients. A sequential study of anxiety and depression using the hospital anxiety and depression scale. Support Care Cancer 1999;7:396-9. [PubMed]
- Fallowfield LJ, Jenkins VA, Beveridge HA. Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med 2002;16:297-303. [PubMed]
- Bradley EH, Hallemeier AG, Fried TR, et al. Documentation of discussions about prognosis with terminally ill patients. Am J Med 2001;111:218-23. [PubMed]
- Bruera E, Neumann CM, Mazzocato C, et al. Attitudes and beliefs of palliative care physicians regarding communication with terminally ill cancer patients. Palliat Med 2000;14:287-98. [PubMed]
- Georgaki S, Kalaidopoulou O, Liarmakopoulos I, et al. Nurses' attitudes toward truthful communication with patients with cancer. A Greek study. Cancer Nurs 2002;25:436-41. [PubMed]
- Annunziata MA, Talamini R, Tumolo S, et al. Physicians and death: comments and behaviour of 605 doctors in the north-east of Italy. Support Care Cancer 1996;4:334-40. [PubMed]
- Grassi L, Giraldi T, Messina EG, et al. Physicians' attitudes to and problems with truth-telling to cancer patients. Support Care Cancer 2000;8:40-5. [PubMed]
- Gordon DR, Paci E. Disclosure practices and cultural narratives: understanding concealment and silence around cancer in Tuscany, Italy. Soc Sci Med 1997;44:1433-52. [PubMed]
- Tan TK, Teo FC, Wong K, et al. Cancer: To tell or not to tell? Singapore Med J 1993;34:202-3. [PubMed]
- Harris JJ, Shao J, Sugarman J. Disclosure of cancer diagnosis and prognosis in Northern Tanzania. Soc Sci Med 2003;56:905-13. [PubMed]
- Mystakidou K, Parpa E, Tsilila E, et al. Cancer information disclosure in different cultural contexts. Support Care Cancer 2004;12:147-54. [PubMed]
- Al-Amri AM. Cancer patients' desire for information: a study in a teaching hospital in Saudi Arabia. East Mediterr Health J 2009;15:19-24. [PubMed]
- Repetto L, Piselli P, Raffaele M, et al. Communicating cancer diagnosis and prognosis: when the target is the elderly patient-a GIOGer study. Eur J Cancer 2009;45:374-83. [PubMed]
- Yun YH, Lee CG, Kim SY, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol 2004;22:307-14. [PubMed]
- Wang XL, Hang XW, Zhang Y, et al. Information needs of cancer patients about diagnosis. Journal of Henan University 2002;21:5-10. (Medical Science).
- Jiang Y, Liu C, Li JY, et al. Different attitudes of Chinese patients and their families toward truth telling of different stages of cancer. Psychooncology 2007;16:928-36. [PubMed]
- Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer 2001;84:48-51. [PubMed]
- Horikawa N, Yamazaki T, Sagawa M, et al. Changes in disclosure of information to cancer patients in a general hospital in Japan. Gen Hosp Psychiatry 2000;22:37-42. [PubMed]
- Liao CL, Xu YM. A Survey on the Situation of Tumor Patient's Demand for the Right of Being Informed. Journal Of Nursing Science 2006;21:37-9. (in Chinese).
- Jiang Y, Li JY, Liu C, et al. Different attitudes of oncology clinicians toward truth telling of different stages of cancer. Support Care Cancer 2006;14:1119-25. [PubMed]
- Fielding R, Wong L, Ko L. Strategies of information disclosure to Chinese cancer patients in an Asian community. Psychooncology 1998;7:240-51. [PubMed]
- Ruhnke GW, Wilson SR, Akamatsu T, et al. Ethical decision making and patient autonomy: a comparison of physicians and patients in Japan and the United States. Chest 2000;118:1172-82. [PubMed]
- Sullivan RJ, Menapace LW, White RM. Truth-telling and patient diagnoses. J Med Ethics 2001;27:192-7. [PubMed]
- Huang X, Butow P, Meiser B, et al. Attitudes and information needs of Chinese migrant cancer patients and their relatives. Aust N Z J Med 1999;29:207-13. [PubMed]
- Hoffman BM, Zevon MA, D'Arrigo MC, et al. Screening for distress in cancer patients: the NCCN rapid-screening measure. Psychooncology 2004;13:792-9. [PubMed]
- Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer 2005;103:1494-502. [PubMed]
- Trask PC, Paterson A, Riba M, et al. Assessment of psychological distress in prospective bone marrow transplant patients. Bone Marrow Transplant 2002;29:917-25. [PubMed]
- Ransom S, Jacobsen PB, Booth-Jones M. Validation of the Distress Thermometer with bone marrow transplant patients. Psychooncology 2006;15:604-12. [PubMed]
- Becker G, Jors K, Block S. Discovering the truth beyond the truth. J Pain Symptom Manage 2015;49:646-9. [PubMed]
- Costantini M, Morasso G, Montella M, et al. Diagnosis and prognosis disclosure among cancer patients. Results from an Italian mortality follow-back survey. Ann Oncol 2006;17:853-9. [PubMed]
- Kawakami S, Arai G, Ueda K, et al. Physician's attitudes towards disclosure of cancer diagnosis to elderly patients: a report from Tokyo, Japan. Arch Gerontol Geriatr 2001;33:29-36. [PubMed]
- Yoshida S, Hirai K, Morita T, et al. Experience with prognostic disclosure of families of Japanese patients with cancer. J Pain Symptom Manage 2011;41:594-603. [PubMed]
- Figg WD, Smith EK, Price DK, et al. Disclosing a diagnosis of cancer: where and how does it occur? J Clin Oncol 2010;28:3630-5. [PubMed]
- Jordan P, Quadrelli S, Heres M, et al. Examining patients' preferences for participation in clinical decision-making: the experience in a Latin American chronic obstructive pulmonary disease and cancer outpatient population. Intern Med J 2014;44:281-7. [PubMed]
- Yun YH, Kwon YC, Lee MK, et al. Experiences and attitudes of patients with terminal cancer and their family caregivers toward the disclosure of terminal illness. J Clin Oncol 2010;28:1950-7. [PubMed]
- Zheng J, Li XB, Sun TJ. Effect of knowing the fact to psycho-requirement of cancer patients. China Journal of Modern Medicine 2005;15:791-3. (in Chinese).
- Piriz IE, Ferro NE, Di Pretoro M, et al. Distress in oncology patients: Distress thermometer in a Latin American study. J Clin Oncol 2005;23:abstr 8211.
- Badr H, Gupta V, Sikora A, et al. Psychological distress in patients and caregivers over the course of radiotherapy for head and neck cancer. Oral Oncol 2014;50:1005-11. [PubMed]


