
The better surgical timing and approach for orbital fracture: a systematic review and meta-analysis
Introduction
Orbital fracture is a disease wherein an external force acting on the eye causes the orbital pressure to rise and the orbital bone wall to rupture (1,2). Safety accidents frequently occur in traffic or industrial production. In recent years, with the increasing economic development, the incidence of orbital fractures has also risen. Orbital fractures can lead to soft tissue herniation in the orbit and incarceration of extraocular muscles, with clinical manifestations such as entropion, eye movement disorders, and diplopia, which seriously affect the quality of life of patients (3,4). Surgery is the main treatment method to release the incarcerated extraocular muscles, incorporate soft tissue herniation into the paranasal sinuses, and repair orbital wall defects(5).
There are many factors affecting the results of surgery, including the timing of surgery, repair materials, and surgical approach (6-9). Most orbital fractures do not require immediate repair, depending on the severity and type of fracture. Some authors believe that repair of orbital fractures within 2 weeks is acceptable in the absence of an indication for urgent surgery (10,11). Some studies have even suggested that the earliest time to repair orbital fractures should be within 2 weeks, but there is insufficient evidence for how early surgical treatment of orbital fractures should start and how prognosis is influenced if surgical treatment is delayed (12,13).
The most classic surgical approaches are mainly divided into transconjunctival approach (TCA) and subciliary approach (SCA) (14,15). In 1921, Lynch first used a medial canthal skin incision to expose the inner orbital wall, and it has been widely used since (16). There are also many scholars who use a transconjunctival incision to treat orbital medial wall, inferior wall, or combined medial-inferior wall fractures to avoid visible skin scarring after surgery (17-19). However, for inferior orbital wall or intraorbital inferior wall combined fractures, exposure of the surgical field is not sufficient through the conjunctival incision, and there is interference of intraorbital fat (20). In the past, both the SCA and the TCA have been widely used for the treatment of orbital fractures. However, there is still controversy as to which is the best surgical approach for orbital fractures (21,22).
The key to the surgical treatment of orbital fractures lies in the incidence of postoperative complications. In this paper, through meta-analysis, with the more controversial 2 weeks as the threshold, the incidence of complications after surgery within 2 weeks and after 2 weeks of injury was compared. In addition, we also compared the post-surgical complications of TCA and SCA. The purpose of this study was to determine the better surgery timing and approach for orbital fractures, and provide a reference for clinicians. We present the following article in accordance with the MOOSE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1465/rc).
Methods
Literature search strategy
We performed a systematic search for relevant studies from inception to December 2021 in the databases of PubMed, Cochrane Clinical Trials Database, Embase, and Web of Science (WOS). We used the following keywords: “orbital fractures”, “orbital fracture”, “orbital trauma”, “orbital injury”, “surgery”, “surgical”, “timing”, “14 days”, “2 weeks”, “approach”, “transconjunctival”, and “subciliary”. All these search words were combined using the Boolean operators “AND” or “OR”. The search strategies for all databases are presented in Table 1. Disagreements were resolved through consensus between the 2 reviewers (P Zhou and Y Qi).
Table 1
| Search number | Queries |
|---|---|
| Queries in PubMed | |
| #1 | Search “orbital fractures” [Mesh] |
| #2 | Search ((((orbital fractures [Title/Abstract]) OR orbital fracture [Title/Abstract]) OR orbital trauma [Title/Abstract]) OR orbital injury [Title/Abstract]) |
| #3 | #1 OR #2 |
| #4 | Search ((((((((surgery [Title/Abstract]) OR surgical [Title/Abstract]) OR timing [Title/Abstract]) OR 14 days [Title/Abstract]) OR 2 weeks [Title/Abstract]) OR approach [Title/ Abstract]) OR transconjunctival [Title/Abstract]) OR subciliary [Title/Abstract]) |
| #5 | #3 AND #4 |
| Queries in Cochrane | |
| #1 | MeSH descriptor: (orbital fractures) explode all trees |
| #2 | ((orbital fractures*) OR (orbital fracture*) OR (orbital trauma*) OR (orbital injury*)): ti, ab, kw |
| #3 | #1 OR #2 |
| #4 | MeSH descriptor: (surgery) explode all trees |
| #5 | ((surgery*) OR (surgical*) OR (timing*) OR (14 days*) OR (2 weeks*) OR (approach*) OR (transconjunctival*) OR (subciliary*)): ti, ab, kw |
| #6 | #4 OR #5 |
| #7 | #3 AND #6 |
| Queries in Embase | |
| #1 | 'orbital fractures'/exp OR 'orbital fracture' OR 'orbital trauma' OR 'orbital injury': ti, ab |
| #2 | 'surgery': ti, ab OR 'surgical': ti, ab OR 'timing': ti, ab OR '14 days': ti, ab OR '2 weeks': ti, ab OR 'approach': ti, ab OR 'transconjunctival': ti, ab OR 'subciliary': ti, ab |
| #3 | #1 AND #2 |
| Queries in WOS | |
| #1 | TS = (orbital fractures OR orbital fracture OR orbital trauma OR orbital injury) |
| #2 | TI = (surgery OR surgical OR timing OR 14 days OR 2 weeks OR approach OR transconjunctival OR subciliary) |
| #3 | #1 AND #2 |
MeSH, Medical Subject Headings.
Study selection
We considered studies eligible for inclusion if they met the following criteria: (I) inclusion only of patients diagnosed with orbital fracture; (II) the article involved the comparison of surgical timing or approach; and (III) there were at least 1 of the primary outcomes of interest. The exclusion criteria were as follows: (I) studies that did not meet the inclusion criteria; (II) relevant results that were not adequately reported or could not be used; and (III) studies were reviews, letters, abstracts, or duplicate publications.
Data extraction
Data were extracted in duplicate by 2 investigators independently and inputted to a dedicated database. Prespecified data elements were extracted from each trial using a structured data form, including baseline characteristics, sample size, and related results of major complications.
Quality assessment
Since the included studies were mainly retrospective or prospective cohort studies, we used the Newcastle-Ottawa scale (NOS) as the evaluation tool for methodological quality, which included adequacy selection of cohort, comparability of studies, and outcome assessment.
Statistical analysis
Analyses were performed using Review Manager version 5.4 (RevMan 5.4; The Cochrane Collaboration, Copenhagen, Denmark, 2020), while Egger’s test was performed using Stata version 14.0 (Stata Corp., College Station, TX, USA). As our outcome variables were dichotomous variables, we used the Mantel-Haenszel odds ratio (OR) model with 95% confidence interval (CI) for combined analysis. Heterogeneity between the studies in effect measures was assessed using both the chi-squared test and the I2 statistic with an I2 value >50%, indicative of substantial heterogeneity. The fixed-effects model was used in the absence of significant heterogeneity; otherwise, the random-effects model was applied. To further evaluate the robustness of the final results, we conducted sensitivity analysis. Funnel plots and Egger's test were used to examine the publication bias among the included studies.
Results
Search process
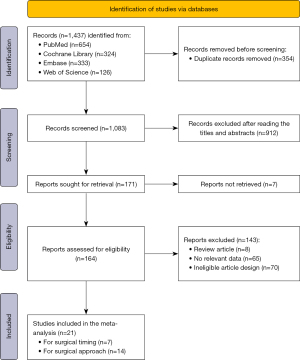
A total of 1,473 relevant articles were identified through a primary literature search using the described search strategy and inclusion/exclusion criteria. After duplicate elimination, 1,083 studies underwent title and abstract screening, resulting in 171 studies considered suitable for inclusion. Following full paper review, 21 articles met the criteria for inclusion, of which 7 were included in the meta-analysis of surgical timing for orbital fracture (23-29), and the other 14 were included in the meta-analysis of surgical approach for orbital fracture (30-43). The results of the search process, which followed the Meta-analyses of Observational Studies in Epidemiology (MOOSE) checklist, including reasons for exclusion of studies, are illustrated in Figure 1.
Characteristics of the included studies
The detailed characteristics of the 7 studies included for surgical timing analysis and 14 studies included for surgical approach analysis are summarized in Tables 2,3, respectively.
Table 2
| Study | Study design | Country | Gender (M/F) | Age (years) |
No. of patients | No. of diplopia | No. of enophthalmos | Follow-up | Duration | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤14 days | >14 days | ≤14 days | >14 days | ≤14 days | >14 days | |||||||||
| Dal Canto 2008 | Retrospective study | USA | NR | 5–68 | 36 | 22 | 3 | 1 | 1 | 0 | 24 weeks | September 1994 to December 2006 | ||
| Brucoli 2011 | Retrospective study | Italy | 29/11 | 47.7 [30–60] | 36 | 4 | 13 | 4 | 7 | 4 | 39 months | January 2001 to December 2007 | ||
| Hosal 2002 | Retrospective study | USA | 30/12 | 32 [12–74] | 25 | 12 | 2 | 5 | 1 | 2 | 11 months | 1992 to 1998 | ||
| Shin 2011 | Retrospective study | Korea | 433/148 | NR | 485 | 106 | 23 | 6 | 3 | 1 | 6 months | May 2000 to December 2007 | ||
| Hwang 2012 | Retrospective study | Korea | NR | 33.4 [6–77] | 228 | 14 | 5 | 0 | 2 | 0 | 12 months | March 2006 to February 2011 | ||
| Poeschl 2012 | Retrospective study | Austria | 38/22 | 36 [4–48] | 43 | 17 | – | – | 1 | 0 | 14 months | NR | ||
| Yu 2016 | Retrospective study | China | 181/74 | 27.6 [7–74] | 167 | 88 | 31 | 26 | – | – | 14.2 months | July 2003 to December 2014 | ||
NR, no reported.
Table 3
| Study | Study design | Country | Gender (M/F) | Age | No. of patients | No. of ectropion | No. of entropion | No. of scleral show | No. of canthal malposition | No. of visible scar | Follow-up | Duration | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TCA | SCA | TCA | SCA | TCA | SCA | TCA | SCA | TCA | SCA | TCA | SCA | ||||||||||||
| Appling 1993 | Retrospective study | USA | 41/18 | 11–60 | 36 | 27 | 0 | 3 | – | – | 1 | 7 | 3 | 0 | – | – | 4 months | March 1987 to February 1992 | |||||
| Ridgway 2009 | Retrospective study | USA | 72/28 | 39 [16–90] | 45 | 56 | 0 | 7 | 2 | 0 | – | – | – | – | 0 | 2 | 6 months | 1998 to 2008 | |||||
| Salgarelli 2010 | Retrospective study | Italy | 169/105 | 37.1 [16–78] | 32 | 219 | 0 | 0 | – | – | 0 | 3 | – | – | 1 | 38 | 48 months | 2000 to 2007 | |||||
| Giraddi 2012 | Prospective study | India | 19/1 | 28.4 [12–45] | 10 | 10 | 1 | 3 | 3 | 0 | – | – | – | – | – | – | 3 months | NR | |||||
| Raschke 2012 | Prospective study | Germany | 171/50 | 44.76±19.15 | 129 | 92 | 2 | 6 | – | – | 11 | 29 | – | – | – | – | 9 months | September 2006 to September 2011 | |||||
| Ishida 2016 | Retrospective study | Japan | NR | NR | 179 | 29 | 1 | 2 | 6 | 0 | 0 | 2 | 1 | 0 | – | – | 12 months | 1992 to 2012 | |||||
| Kesselring 2016 | Retrospective study | USA | NR | 37.5 [4–83] | 26 | 47 | 0 | 1 | 0 | 0 | – | – | – | – | – | – | NR | 2011 to 2011 | |||||
| Pausch 2016 | Retrospective study | Germany | 248/98 | 42.7 [5–89] | 121 | 225 | 0 | 8 | 3 | 0 | – | – | – | – | – | – | 6 months | January 2001 to December 2010 | |||||
| Vaibhav 2016 | Prospective study | India | 36/4 | 20–60 | 20 | 20 | 0 | 0 | 1 | 0 | – | – | – | – | 0 | 4 | 3 months | NR | |||||
| Haghighat 2017 | Retrospective study | Italy | NR | 26.7 [17–44] | 17 | 17 | 0 | 3 | – | – | – | – | – | – | – | – | 4 weeks | 2015 | |||||
| Neovius 2017 | Retrospective study | Sweden | 249/68 | 41 [8–88] | 91 | 37 | 2 | 3 | 0 | 0 | 4 | 4 | 2 | 0 | – | – | 6 months | June 2005 to December 2012 | |||||
| Bronstein 2020 | Retrospective study | USA | 151/33 | 35.1±12.1 | 102 | 82 | 2 | 2 | 4 | 1 | – | – | – | – | – | – | 6 months | 2005 to 2016 | |||||
| Mohamed 2020 | Prospective study | Egypt | 20/10 | 35.5±11.8 | 15 | 15 | 1 | 3 | 3 | 0 | 2 | 4 | – | – | – | – | 6 months | August 2017 to April 2019 | |||||
| Trevisiol 2021 | Retrospective study | Italy | 53/16 | 42 [6–78] | 33 | 36 | 0 | 3 | 0 | 0 | – | – | – | – | – | – | 35 months | January 2013 to September 2018 | |||||
TCA, transconjunctival approach; SCA, subciliary approach; NR, no reported.
All of the 7 studies included in the meta-analysis of surgical timing were retrospective studies. The total number of patients was 1,283, including 1,020 patients in the ≤14 days group and 263 patients in the >14 days group. The main complications were diplopia and enophthalmos, with 119 patients (9.28%) and 22 patients (1.72%), respectively. The included studies were published between 2008 and 2016.
The 14 studies included in the meta-analysis of surgical approach contained 10 retrospective studies and 4 prospective studies. The total number of patients was 1,768, including 856 patients in the TCA group and 912 patients in the SCA group. The main complications were ectropion, entropion, scleral show, canthal malposition, and visible scar, with 53 patients (3.00%), 23 patients (1.30%), 67 patients (3.79%), 6 patients (0.34%), and 45 patients (2.55%), respectively. The included studies were published between 1993 and 2021.
Results of quality assessment
After identifying the trials, abstracts and full texts were carefully read and risk of bias was screened and evaluated according to the NOS. Table 4 shows a summary of all kinds of bias in each study included in the surgical timing meta-analysis, while Table 5 shows the bias in each study included in the surgical approach meta-analysis. The results showed that the quality of all articles was higher than 7 points, and some articles were only deducted in terms of comparability and outcome evaluation.
Table 4
| Study | Selection | Comparability of cohorts | Outcomes | Score* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of cohort | Selection of nonexposed cohort | Ascertainment of exposure | Outcome lacking at the beginning |
Outcome assessment | Sufficient follow-up time | Follow up adequacy | |||
| Dal Canto 2008 | ★ | ★ | ★ | ★ | ★★ | ☆ | ★ | ★ | 8 |
| Brucoli 2011 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Hosal 2002 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Shin 2011 | ★ | ★ | ★ | ☆ | ★★ | ★ | ★ | ★ | 8 |
| Hwang 2012 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
| Poeschl 2012 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Yu 2016 | ★ | ★ | ★ | ☆ | ★★ | ★ | ★ | ★ | 8 |
*, the total score of NOS evaluation is 9 points; ★ represents that the item has obtained the score, ☆ represents that the item has not been scored.
Table 5
| Study | Selection | Comparability of cohorts | Outcomes | Score* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of cohort | Selection of nonexposed cohort | Ascertainment of exposure | Outcome lacking at the beginning |
Outcome assessment | Sufficient follow-up time | Follow up adequacy | |||
| Appling 1993 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
| Ridgway 2009 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Salgarelli 2010 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
| Giraddi 2012 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Raschke 2012 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Ishida 2016 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Kesselring 2016 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
| Pausch 2016 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
| Vaibhav 2016 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Haghighat 2017 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Neovius 2017 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Bronstein 2020 | ★ | ★ | ★ | ★ | ★☆ | ★ | ★ | ★ | 8 |
| Mohamed 2020 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Trevisiol 2021 | ★ | ★ | ★ | ★ | ★☆ | ☆ | ★ | ★ | 7 |
*, the total score of NOS evaluation is 9 points; ★, represents that the item has obtained the score; ☆, represents that the item has not been scored.
Results of the meta-analysis for surgical timing
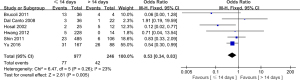
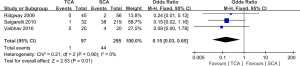
Diplopia
In 1,223 patients across 6 studies, surgical timing in the ≤14 days group indicated a lower incidence of diplopia than in the >14 days group (OR: 0.53, 95% CI: 0.34 to 0.83, P=0.005), without significant heterogeneity (I2=23%, P=0.26) (Figure 2). Sensitivity analysis showed that the results were relatively stable (Figure S1). Nonsignificant publication bias was found according to the funnel plot or Egger’s test (P=0.536) (Figure S2).
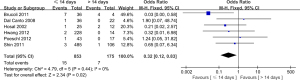
Enophthalmos
Enophthalmos was reported in 6 studies involving 1,028 patients. The ≤14 days group also showed a lower incidence of enophthalmos compared to the >14 days group (OR: 0.32, 95% CI: 0.12 to 0.83, P=0.02), there was no significant heterogeneity (I2=0%, P=0.44) (Figure 3). We performed sensitivity analysis and the results showed that there was no obvious change (Figure S1). Neither funnel plot nor Egger’s test (P=0.641) revealed any publication bias (Figure S2).
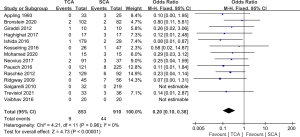
Results of the meta-analysis for surgical approach
Ectropion
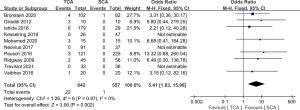
In 14 studies involving 1,763 patients, TCA was associated a significantly lower incidence of ectropion compared to SCA (OR: 0.20, 95% CI: 0.10 to 0.38, P<0.00001), without significant heterogeneity (I2=0%, P=0.96) (Figure 4). Sensitivity analysis showed that the results were robust (Figure S3). Although the funnel plot was not symmetrical, the results of Egger’s test showed no significant publication bias (P=0.319) (Figure S4).
Entropion
A total of 10 studies involving 1,199 patients contributed to the analysis of entropion, wherein TCA showed a significantly higher incidence of entropion compared to SCA (OR: 5.41, 95% CI: 1.83 to 15.96, P=0.002), without significant heterogeneity (I2=0%, P=0.97) (Figure 5). No significant change was found after the sensitivity analysis (Figure S3). The funnel plot showed some evidence of asymmetry, but Egger’s test indicated no significant publication bias (P=0.254) (Figure S4).
Scleral show
A total of 6 studies reported the incidence of scleral show, and TCA was associated with a significantly lower incidence compared to SCA (OR: 0.22, 95% CI: 0.12 to 0.38, P<0.00001). We used the fixed-effects model to perform the pooled analysis because of the low heterogeneity (I2=0%, P=0.49) (Figure 6). The result did not change after the sensitivity analysis (Figure S3). There was no significant publication bias according to the Egger’s test (P=0.428) (Figure S4).
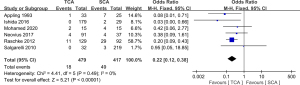
Canthal malposition
Data was available in 3 studies to assess canthal malposition. The meta-analysis showed that there was no difference between TCA and SCA regarding the incidence of canthal malposition (OR: 2.36, 95% CI: 0.42 to 13.40, P=0.33), and the heterogeneity among included studies was not significant (I2=0%, P=0.53) (Figure 7). The result of sensitivity analysis indicated that it was stable (Figure S3). The funnel plot was roughly asymmetric; however, Egger’s test indicated that there was no publication bias (P=0.382) (Figure S4).

Visible scar
There was a total of 392 patients enrolled in 3 studies which compared the incidence of visible scar. The pooled analysis showed that TCA had a significantly lower incidence of visible scar than SCA (OR: 0.15, 95% CI: 0.03 to 0.65, P=0.01), without significant heterogeneity (I2=0%, P=0.90) (Figure 8). The result of sensitivity analysis showed no obvious change, suggesting that it was reliable (Figure S3). The funnel plot appeared symmetric, and the Egger’s test was nonsignificant (P=0.486) (Figure S4).
Discussion
As the orbit is an important aesthetic component of the face, fracture repair surgery faces certain challenges, and its complications often cause aesthetic and functional concerns (44,45). The timing and approach of surgery for orbital fractures has been widely debated, with some authors suggesting that conservative management is more beneficial than early surgical intervention (46). Isolated orbital floor fractures do not require urgent surgical intervention in the absence of specific indications such as muscle entrapment and/or visual threat. Orbital edema or hematoma can also improve significantly after several weeks without intervention (47). However, when symptoms persist, surgery may be required, and there is no clear consensus on the optimal timing of orbital fractures in these cases (48). For the surgical procedure, orthopedic surgery usually requires adequate exposure of the bone. The SCA takes the most direct route through the soft tissue to the bone, and in doing so, scars are easily produced. Making an incision through the TCA can effectively conceal scarring, but because the bones cannot be sufficiently exposed, it may occasionally lead to functional and aesthetic complications, such as eyelid asymmetry, scleral show, and so on (49,50).
In this meta-analysis, we used the 14 days surgical margin as a threshold for optimal timing of surgery and compared the incidence of complications between the TCA and the SCA to determine the optimal surgical approach. The results showed that surgery with 14 days after injury significantly reduced the incidence of diplopia (OR: 0.53, 95% CI: 0.34 to 0.83, P=0.005) and enophthalmos (OR: 0.32, 95% CI: 0.12 to 0.83, P=0.02). The incidence of ectropion (OR: 0.20, 95% CI: 0.10 to 0.38, P<0.00001), scleral show (OR: 0.22, 95% CI: 0.12 to 0.38, P<0.00001), and visible scar (OR: 0.15, 95% CI: 0.03 to 0.65, P=0.33) in the TCA group decreased significantly when compared with the SCA group, but the incidence of entropion (OR: 5.41, 95% CI: 1.83 to 15.96, P=0.002) increased significantly, in addition, there was no significant difference in the incidence of canthal malposition (OR: 2.36, 95% CI: 0.42 to 13.40, P=0.33) between the 2 approaches.
Regarding the timing of surgery, this study demonstrated better outcomes when surgery was performed within 14 days after injury, and other reports have shown that early intervention may lead to better postoperative outcomes, with lower incidences of diplopia and entropy (51). For example, Jazayeri et al. found that the cut-off point of 14 days or 28 days showed a significant improvement in the results of early intervention (52); Byeon’s study confirmed that the effect of correcting intraocular lesions within 1 month after injury was significantly better, while delayed surgical intervention lead to more serious complications such as tissue fibrosis and atrophy (53). The feasible reason is that early intervention can significantly reduce periorbital soft tissue scarring, and early reversal of persistent tissue compression, stretching, and displacement may limit advanced fibrosis, especially in the presence of massive soft tissue swelling (54,55).
For the surgical approach, both the TCA and the SCA seem to have their own advantages and disadvantages. With SCA, although the fracture area is fully exposed and it is easy to perform surgical repair operations, skin scars may easily form, and it is carries a higher risk of damaging the muscle tissue at the incision site, resulting in increased ectropion and sclera exposure and other complications (56,57). With TCA, combined lateral canthotomy may be required, which will easily increase the surgical duration and tissue damage, and may also lead to conjunctival edema, entropion, foreign body sensation, and eyelid tearing. Although the complication rate of the TCA is not high, it often requires secondary surgery (34,40).
This study had certain limitations. There were large differences in fracture types, repair materials, methods of assessing complications, and follow-up time among all included studies, and we were unable to classify, which may have reduced the accuracy of the evidence. In addition, the 21 studies included were all cohort studies, and most of the studies were retrospective studies, which may have involved selection bias and retrospective bias; no randomized controlled trials were included, which may have reduced the strength of the conclusions. Finally, the timing of surgery may interact with the surgical approach, resulting in differences in the complications analyzed separately. We hope that more robust articles will assist the validation of our stratified analysis in the future.
Conclusions
In conclusion, this study confirmed that early surgical intervention can achieve better clinical outcomes. When considering the surgical approach, the TCA and SCA have their own advantages and disadvantages. The literature and related evidence levels included in this study were limited, so more research should be performed to confirm the optimal surgical timing and approach for orbital fractures.
Acknowledgments
Funding: This work was supported by research grants from the Scientific Research Project of Heilongjiang Provincial Health Commission (No. 2019-333).
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1465/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1465/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harris GJ. Orbital blow-out fractures: surgical timing and technique. Eye (Lond) 2006;20:1207-12. [Crossref] [PubMed]
- Bhatti N, Kanzaria A, Huxham-Owen N, et al. Management of complex orbital fractures. Br J Oral Maxillofac Surg 2016;54:719-23. [Crossref] [PubMed]
- Sukegawa S, Kanno T, Shibata A, et al. Treatment of Orbital Fractures with Orbital-Wall Defects using Anatomically Preformed Orbital Wall Reconstruction Plate System. J Hard Tissue Biol 2017;26:231-6. [Crossref]
- Gruss JS. Complex nasoethmoid-orbital and midfacial fractures: role of craniofacial surgical techniques and immediate bone grafting. Ann Plast Surg 1986;17:377-90. [Crossref] [PubMed]
- Zimmerer RM, Ellis E 3rd, Aniceto GS, et al. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Craniomaxillofac Surg 2016;44:1485-97. [Crossref] [PubMed]
- Chen YH, Tsai YJ, Tzeng IS. Factors influencing surgical outcomes in orbital trapdoor fracture. Sci Rep 2021;11:17547. [Crossref] [PubMed]
- Patel S, Andrecovich C, Silverman M, et al. Biomechanic Factors Associated With Orbital Floor Fractures. JAMA Facial Plast Surg 2017;19:298-302. [Crossref] [PubMed]
- Graham DO, Lim CGT, Coghlan P, et al. A Literature Review of Rapid Prototyping and Patient Specific Implants for the Treatment of Orbital Fractures. Craniomaxillofac Trauma Reconstr 2022;15:83-9. [Crossref] [PubMed]
- Kooger T, Joosse MV, Minderhout E, et al. Epidemiology of Orbital Fractures in a Large Hospital in the Netherlands: Results of Implementation of a Multidisciplinary Orbital Trauma Team. Open J Ophthalmol 2021;15:122-9. [Crossref]
- Bregman JA, Vakharia KT, Idowu OO, et al. Outpatient Surgical Management of Orbital Blowout Fractures. Craniomaxillofac Trauma Reconstr 2019;12:205-10. [Crossref] [PubMed]
- Yamanaka Y, Watanabe A, Sotozono C, et al. Impact of surgical timing of postoperative ocular motility in orbital blowout fractures. Br J Ophthalmol 2018;102:398-403. [Crossref] [PubMed]
- Su Y, Shen Q, Bi X, et al. Delayed surgical treatment of orbital trapdoor fracture in paediatric patients. Br J Ophthalmol 2019;103:523-6. [Crossref] [PubMed]
- Dubois L, Steenen SA, Gooris PJJ, et al. Controversies in orbital reconstruction—II. Timing of post-traumatic orbital reconstruction: A systematic review. Int J Oral Maxillofac Surg 2015;44:433-40. [Crossref] [PubMed]
- Sales PHDH, Rocha SSD, Rodrigues PHC, et al. Surgical Treatment of Posttraumatic Ophthalmoplegia Through the Reconstruction of the Lateral Orbital Wall. J Craniofac Surg 2017;28:e444-6. [Crossref] [PubMed]
- Strobel L, Hölzle F, Riediger D, et al. Subtarsal Versus Transconjunctival Approach-Esthetic and Functional Long-Term Experience. J Oral Maxillofac Surg 2016;74:2230-8. [Crossref] [PubMed]
- Kim DW, Choi SR, Park SH, et al. Versatile use of extended transconjunctival approach for orbital reconstruction. Ann Plast Surg 2009;62:374-80. [Crossref] [PubMed]
- Santosh BS, Giraddi G. Transconjunctival preseptal approach for orbital floor and infraorbital rim fracture. J Maxillofac Oral Surg 2011;10:301-5. [Crossref] [PubMed]
- Raschke G, Djedovic G, Peisker A, et al. The isolated orbital floor fracture from a transconjunctival or subciliary perspective-A standardized anthropometric evaluation. Med Oral Patol Oral Cir Bucal 2016;21:e111-7. [Crossref] [PubMed]
- Procacci P, Trevisiol L, Nocini PF, et al. Modified technique for endoscopic endonasal reduction of medial orbital wall fracture using an absorbable packing. Oral Maxillofac Surg 2017;21:91-8. [Crossref] [PubMed]
- Trento G, Primo BT, Corso P, et al. Treatment of Zygomatic-Orbital Complex Fracture Through Transconjunctival Approach. Int J Med Surg Sci 2015;2:420-5. [Crossref]
- Gooris PJ, Jansen J, Bergsma JE, et al. Evidence-Based Decision Making in Orbital Fractures. Atlas Oral Maxillofac Surg Clin North Am 2021;29:109-27. [Crossref] [PubMed]
- Patel S, Shokri T, Ziai K, et al. Controversies and Contemporary Management of Orbital Floor Fractures. Craniomaxillofac Trauma Reconstr 2021;7:194-8. [Crossref]
- Yu DY, Chen CH, Tsay PK, et al. Surgical Timing and Fracture Type on the Outcome of Diplopia After Orbital Fracture Repair. Ann Plast Surg 2016;76:S91-5. [Crossref] [PubMed]
- Poeschl PW, Baumann A, Dorner G, et al. Functional outcome after surgical treatment of orbital floor fractures. Clin Oral Investig 2012;16:1297-303. [Crossref] [PubMed]
- Hwang K, Huan F, Hwang PJ. Diplopia and enophthalmos in blowout fractures. J Craniofac Surg 2012;23:1077-82. [Crossref] [PubMed]
- Hoşal BM, Beatty RL. Diplopia and enophthalmos after surgical repair of blowout fracture. Orbit 2002;21:27-33. [Crossref] [PubMed]
- Shin KH, Baek SH, Chi M. Comparison of the outcomes of non-trapdoor-type blowout fracture repair according to the time of surgery. J Craniofac Surg 2011;22:1426-9. [Crossref] [PubMed]
- Dal Canto AJ, Linberg JV. Comparison of orbital fracture repair performed within 14 days versus 15 to 29 days after trauma. Ophthalmic Plast Reconstr Surg 2008;24:437-43. [Crossref] [PubMed]
- Brucoli M, Arcuri F, Cavenaghi R, et al. Analysis of complications after surgical repair of orbital fractures. J Craniofac Surg 2011;22:1387-90. [Crossref] [PubMed]
- Raschke GF, Rieger UM, Bader R, et al. Transconjunctival versus subciliary approach for orbital fracture repair—an anthropometric evaluation of 221 cases. Clin Oral Investig 2013;17:933-42. [Crossref] [PubMed]
- Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg 1993;119:1000-7. [Crossref] [PubMed]
- Trevisiol L, D'Agostino A, Gasparini S, et al. Transconjunctival and Subciliary Approach in the Treatment of Orbital Fractures: A Study on Oculoplastic Complication. J Clin Med 2021;10:2775. [Crossref] [PubMed]
- Ridgway EB, Chen C, Colakoglu S, et al. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg 2009;124:1578-86. [Crossref] [PubMed]
- Bronstein JA, Bruce WJ, Bakhos F, et al. Surgical Approach to Orbital Floor Fractures: Comparing Complication Rates Between Subciliary and Subconjunctival Approaches. Craniomaxillofac Trauma Reconstr 2020;13:45-8. [Crossref] [PubMed]
- Giraddi GB, Syed MK. Preseptal transconjunctival vs. subciliary approach in treatment of infraorbital rim and floor fractures. Ann Maxillofac Surg 2012;2:136-40. [Crossref] [PubMed]
- Kesselring AG, Promes P, Strabbing EM, et al. Lower Eyelid Malposition Following Orbital Fracture Surgery: A Retrospective Analysis Based on 198 Surgeries. Craniomaxillofac Trauma Reconstr 2016;9:109-12. [Crossref] [PubMed]
- Neovius E, Clarliden S, Farnebo F, et al. Lower Eyelid Complications in Facial Fracture Surgery. J Craniofac Surg 2017;28:391-3. [Crossref] [PubMed]
- Pausch NC, Sirintawat N, Wagner R, et al. Lower eyelid complications associated with transconjunctival versus subciliary approaches to orbital floor fractures. Oral Maxillofac Surg 2016;20:51-5. [Crossref] [PubMed]
- Ishida K. Evolution of the surgical approach to the orbitozygomatic fracture: From a subciliary to a transconjunctival and to a novel extended transconjunctival approach without skin incisions. J Plast Reconstr Aesthet Surg 2016;69:497-505. [Crossref] [PubMed]
- Haghighat A, Moaddabi A, Soltani P. Comparison of Subciliary, Subtarsal and Transconjunctival Approaches for Management of Zygomaticoorbital Fractures. Br J Med Med Res 2017;20:1-9. [Crossref]
- Vaibhav N, Keerthi R, Nanjappa M, et al. Comparison of ‘sutureless’ Transconjunctival and Subciliary Approach for Treatment of Infraorbital Rim Fractures: a Clinical Study. J Maxillofac Oral Surg 2016;15:355-62. [Crossref] [PubMed]
- Mohamed FI, Reda HM, Khalifa GA. Anthropometric changes in the morphology of the lower eyelid after using three different approaches in patients with orbital fractures. J Craniomaxillofac Surg 2020;48:985-93. [Crossref] [PubMed]
- Salgarelli AC, Bellini P, Landini B, et al. A comparative study of different approaches in the treatment of orbital trauma: an experience based on 274 cases. Oral Maxillofac Surg 2010;14:23-7. [Crossref] [PubMed]
- Gander T, Essig H, Metzler P, et al. Patient specific implants (PSI) in reconstruction of orbital floor and wall fractures. J Craniomaxillofac Surg 2015;43:126-30. [Crossref] [PubMed]
- Amin D, Al-Mulki K, Henriquez OA, et al. Review of Orbital Fractures in an Urban Level I Trauma Center. Craniomaxillofac Trauma Reconstr 2020;13:174-9. [Crossref] [PubMed]
- Nowinski D, Messo E, Hedlund A. Treatment of orbital fractures: evaluation of surgical techniques and materials for reconstruction. J Craniofac Surg 2010;21:1033-7. [Crossref] [PubMed]
- Losee JE, Afifi A, Jiang S, et al. Pediatric orbital fractures: classification, management, and early follow-up. Plast Reconstr Surg 2008;122:886-97. [Crossref] [PubMed]
- Lee CA, Sun H, Yun JY. Usefulness of a Transconjunctival Approach in the Reconstruction of the Medial Blow-Out Wall Fracture. Arch Craniofac Surg 2017;18:76-81. [Crossref] [PubMed]
- Al-Moraissi E, Elsharkawy A, Al-Tairi N, et al. What surgical approach has the lowest risk of the lower lid complications in the treatment of orbital floor and periorbital fractures? A frequentist network meta-analysis. J Craniomaxillofac Surg 2018;46:2164-75. [Crossref] [PubMed]
- Kim CY, Jeong BJ, Lee SY, et al. Comparison of surgical outcomes of large orbital fractures reconstructed with porous polyethylene channel and porous polyethylene titan barrier implants. Ophthalmic Plast Reconstr Surg 2012;28:176-80. [Crossref] [PubMed]
- Cole P, Boyd V, Banerji S, et al. Comprehensive management of orbital fractures. Plast Reconstr Surg 2007;120:57S-63S. [Crossref] [PubMed]
- Jazayeri HE, Khavanin N, Yu JW, et al. Does Early Repair of Orbital Fractures Result in Superior Patient Outcomes? A Systematic Review and Meta-Analysis. J Oral Maxillofac Surg 2020;78:568-77. [Crossref] [PubMed]
- Byeon JY, Choi HJ. Orbital Cellulitis Following Orbital Blow-out Fracture. J Craniofac Surg 2017;28:1777-9. [Crossref] [PubMed]
- He D, Blomquist PH, Ellis E 3rd. Association between ocular injuries and internal orbital fractures. J Oral Maxillofac Surg 2007;65:713-20. [Crossref] [PubMed]
- Campbell BC, Shipchandler TZ, Ting JY, et al. Ocular motility and diplopia measurements following orbital floor fracture repair. Am J Otolaryngol 2021;42:102879. [Crossref] [PubMed]
- Joshi S, Kassira W, Thaller SR. Overview of pediatric orbital fractures. J Craniofac Surg 2011;22:1330-2. [Crossref] [PubMed]
- Bansagi ZC, Meyer DR. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology 2000;107:829-36. [Crossref] [PubMed]


