
Effectiveness and safety of decompression alone versus decompression plus fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a systematic review and meta-analysis
Introduction
Lumbar spinal stenosis (LSS) is the gradual narrowing of the spinal canal caused by age-related changes of the discs and facet joints in the lower back (1). Degenerative spondylolisthesis (DS) is defined as a condition whereby chronic instability and intersegmental degenerative changes result in the slip of one vertebral body over the one below (2). Commonly, LSS occurs combined with DS among patients (LSS + DS) more than 50 years (3). The incidence of LSS + DS appears to be gradually on the rise, and it is estimated that approximately 64 million elderly people will be affected by the year 2025. Due to nerve roots compression, this degenerative condition severely influences motor function, walking ability, and quality of life (4). A study showed that most patients do not respond well to conservative treatments such as physiotherapy, analgesics, and steroids (5). To relieve the associated discomfort and completely decompress the nerve roots, decompression surgery alone or combined with fusion are common clinical surgical interventions (6).
The failure to establish an accurate standard of treatment makes it difficult to appraise the relevant efficacy and safety (7). In clinical practice, spine surgeons may presume that slippage and dynamic instability at the level of spondylolisthesis are better treated with fusion (2). However, there have been lingering controversies reported in several studies regarding these two surgical options (8,9). Previous studies have shown that superior clinical results were achieved when fusion was added to decompression in patients with LSS + DS (10,11). However, some other studies have demonstrated that there are disadvantages to spinal decompression plus fusion compared with decompression alone for LSS + DS patients, including more blood loss, longer operative time, and prolonged length of stay (LOS) (6,12,13). Hua et al. demonstrated that clinical outcomes would not be different among those receiving decompression alone and those undergoing decompression with fusion (14). The differences are probably due to an inconsistent difference in study design, such as search sources, and outcome measurement. Moreover, the relative safety of fusion in addition to standard decompression remains unclear (9). Fusion may increase the risk of instability or help alleviate mechanical back pain in patients with LSS + DS; however, this must be weighed against the possible higher morbidity associated with more extensive fusion surgery, especially as many patients with LSS + DS may be elderly with significant comorbidities (15). Given that the effectiveness and safety of decompression alone or combined with fusion for patients with LSS + DS were still unclear, further study is needed. Meta-analysis is a method of summarizing similar research results, which can expand the sample size and improve statistical validity, especially in the case of inconsistent results from previous studies. Meta-analysis has the ability to obtain results based on existing research results, and comprehensive analysis, which would be closer to real life.
Herein, we conducted this systematic review and meta-analysis to assess the effectiveness and safety of decompression alone or combined with fusion in LSS with DS. We present the following article in accordance with the MOOSE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2208/rc).
Methods
Patient and public involvement
Patients or members of the public were not involved in the design, conduct, reporting, or dissemination plans of our research; the data in this study were accessed from openly-available datasets.
Literature search strategy
The databases of PubMed, Embase, Cochrane Library, and Web of Science from were searched from their inception to 28th December 2021. The search terms included: “Lumbar spondylolisthesis” AND “Decompression with fusion” OR “Posterior Lumbar Interbody Fusion” OR “Transforaminal Lumbar Interbody Fusion” OR “intervertebral fusion” OR “lumbar pedicle screw fixation” OR “Decompression surgery” OR “Laminectomy” OR “Laminectomies” OR “Laminotomy” OR “Laminotomies”. The detailed search strategy for the PubMed database is listed in Appendix 1.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (I) populations: patients with LSS + DS; (II) interventions: patients undergoing decompression alone as the DA group and (III) comparators: patients receiving decompression plus fusion as the FU group; (IV) outcomes: overall reoperation rate (%), complications, Oswestry Disability Index (ODI), operative time (mins), amount of blood loss (mL), LOS (days), and visual analog scales (VAS); (V) study design: cohort studies; (VI) literature published in English. The exclusion criteria were as follows: (I) animal experiments; (II) randomized-controlled trials (RCTs); (III) no valid data; (IV) other pathological studies related to LSS + DS, such as major degenerative lumbar scoliosis or synovial cysts; and (V) meta-analyses, reviews, case reports, conference summaries, and letters.
Data extraction and quality assessment
Two researchers (ZS and XG) reviewed the identified relevant literature and extracted the research data according to inclusion and exclusion criteria. If a discrepancy existed, a third party (RW) would participate in the extraction of data. The data extracted from articles included: names of the first author, year of publication, country, study design, surgical types, gender, age (years), levels of spondylolisthesis, follow-up duration (years), and the quality of included study.
The revised Newcastle-Ottawa scale (NOS) (16) was used for the evaluation of the cohort studies, and those scored 1–4 were considered low- or moderate-quality; those scored 5–10 were considered high quality.
Definitions of variables
Spondylolisthesis is a descriptive term derived from the Greek spondylo (spine) and olisthesis (slip) and was first described by Herbinaux (17), an obstetrician, in 1782. The common feature of the various types is an anterior translation of the cephalad vertebra relative to the adjacent caudal segment. The biomechanical force causing this translation is the anteriorly directed vector created by the contraction of the posteriorly located erector spinal muscles, coupled with the force of gravity acting on the upper body mass through the lordotic lumbar spine and lumbosacral junction.
DS was first described in 1930 by Junghanns (18), who coined the term “pseudospondylolisthesis” to describe the presence of forward slippage of a vertebral body in the presence of an intact neural arch. The clinical and pathologic features of this entity were further defined by Macnab (19), who described the condition as “spondylolisthesis with an intact neural arch”. The term DS was originally coined by Newman and Stone (20) and is the terminology most commonly used to describe the anterior slippage of one vertebral body on another in the presence of an intact neural arch.
The degree of DS was defined using the Meyerding classification grade, which was determined by measuring the degree of slip using standing, neutral lateral radiographs of the lumbar spine. The classification system divides slip into five grades: 0–25%= Grade I, 25–50%= Grade II, 50–75%= Grade III, 75–100%= Grade IV, and greater than 100%= Grade V.
Statistical analysis
The software STATA 15.1 (Stata Corporation, College Station, TX, USA) was used in this meta-analysis. Each indicator was assessed for heterogeneity. Random-effect models were adopted when the heterogeneity statistic I2≥50%; on the contrary, indicators were analyzed by fixed-effect models. All assessment indicators were subjected to sensitivity analysis to test the stability of the result. Subgroup analyses were carried out according to the levels of spondylolisthesis (single level, double levels, single/double levels) and literature quality (low, high). We also analyzed the ODI when the check time (years) was set as a subgroup. Weighted mean difference (WMD) was adopted for efficacy and safety analysis of the quantitative data. Relative risk (RR) was used as the effect indicator for categorical data. A P value <0.05 indicated a statistically significant difference.
Results
Literature search
In this meta-analysis, 3,223 studies were identified through the search of electronic databases. Finally, 12 articles (8,9,12-14,21-27) involving 14,693 patients were included in the current study based on the inclusion criteria, of which 11,598 cases underwent decompression alone and 3,095 cases underwent decompression plus fusion (Figure 1 and Table 1).
Table 1
| First author | Year | Country | Type of study | Groups | Total | M/F | Age (years) | Level of spondylolisthesis | Follow-up duration (years) |
|---|---|---|---|---|---|---|---|---|---|
| Ghogawala | 2004 | USA | CS | D | 20 | NA | 68.8±8.0 | Double levels | 1 |
| PLF | 14 | NA | 68.8±8.0 | ||||||
| Austevoll | 2017 | Norway | CS | D | 260 | 73/187 | 66.7±10.0 | Multilevel levels | 1 |
| FU | 260 | 65/195 | 66.3±9.6 | ||||||
| Ulrich | 2017 | Switzerland | CS | D | 85 | 32/53 | 75.4±7.6 | Single/double levels | 3 |
| FU | 46 | 23/23 | 68.0±7.8 | ||||||
| Aihara | 2018 | Japan | CS | MED | 25 | 14/11 | 62.7±9.74 | Single/double levels | 5 |
| FU | 16 | 6/10 | 64.3±8.98 | ||||||
| Kim | 2018 | Korea | CS | D | 68 | 15/53 | 65.47±9.03 | Single level | 2 |
| PLIF | 61 | 14/47 | 66.75±8.77 | ||||||
| Staartjes | 2018 | Switzerland | CS | D | 51 | 22/29 | 52.7±8.4 | Single level | 2 |
| TLIF | 51 | 25/26 | 53.5±11.1 | ||||||
| Turcotte | 2018 | USA | CS | D | 228 | NA | NA | Single/multilevel levels | 30 days |
| FU | 25 | NA | NA | ||||||
| Kimura | 2019 | Japan | CS | ME-MILD | 28 | 11/17 | 70.0 [34–85] | Single level | 91.3 [60–143] days |
| PLIF | 50 | 16/34 | 68.5 [46–83] | 75.0 [60–93] days | |||||
| Pieters | 2019 | USA | CS | L | 907 | 363/544 | NA | NA | 2 |
| FU | 8,699 | 3,246/5,448 | NA | ||||||
| Joelson | 2021 | Sweden | CS | D | 597 | 190/407 | 69±9.9 | Single level | 7.9 |
| FU | 1,338 | 311/1,027 | 65±9.1 | 7.8 | |||||
| Hua | 2021 | China | CS | LE-ULBD | 24 | 8/16 | 59.0±7.9 | Single level | 2 |
| MI-TLIF | 36 | 10/26 | 59.9±8.6 | ||||||
| Badhiwala | 2021 | Canada | CS | L | 802 | 305/497 | 64.4±11.6 | Single level | 2 |
| FU | 1,002 | 348/654 | 62.7±12.1 |
FU, decompression with fusion; PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; MED, microendoscopic decompression; ME-MILD, microendoscopic muscle-preserving interlaminar decompression; L, laminectomy; D, decompression; LE-ULBD, lumbar endoscopic unilateral laminotomy bilateral decompression; MI-TLIF, minimally invasive transforaminal lumbar interbody fusion; CS, cohort study; NA, missing data.
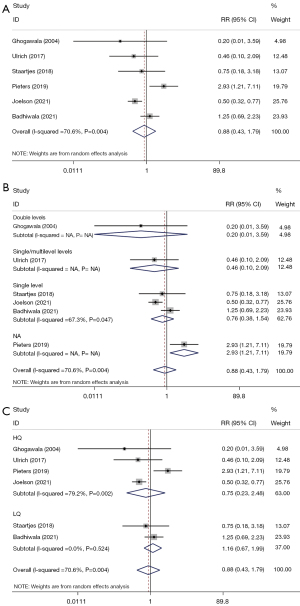
Overall reoperation rate
Six studies reported overall reoperation rate (%). Heterogeneity test results showed that I2=70.6%, so a random effects model was used for analysis. The results indicated that there was no significant difference between the DA group and the FU group [RR: 0.879, 95% confidence interval (CI): 0.432 to 1.786, P=0.721]. The subgroup analyses were based on the different study designs, the article quality, and levels of spondylolisthesis, respectively. Subgroup analyses also showed no difference of overall reoperation rate between the two groups in line with the levels of spondylolisthesis: single level (I2=67.3%, RR: 0.761, 95% CI: 0.376 to 1.542, P=0.449); double levels (RR: 0.200, 95% CI: 0.011 to 3.592, P=0.275); and single/multilevel levels (RR: 0.462, 95% CI: 0.102 to 2.086, P=0.315). Moreover, in the subgroup analysis of article quality, the results revealed no difference between the two groups in all the high-quality articles (I2=79.2%, RR: 0.754, 95% CI: 0.229 to 2.485, P=0.643) and low-quality studies (RR: 1.159, 95% CI: 0.674 to 1.994, P=0.593) (Table 2, Figure 2A-2C).
Table 2
| Characteristics | RR/WMD (95% CI) | P value | I2 |
|---|---|---|---|
| Overall reoperation rate, % | |||
| Overall | 0.879 (0.432, 1.786) | 0.721 | 70.6 |
| Sensitivity analysis | 0.879 (0.432, 1.786) | ||
| Quality | |||
| HQ | 0.754 (0.229, 2.485) | 0.643 | 79.2 |
| LQ | 1.159 (0.674, 1.994) | 0.593 | 0 |
| Level of spondylolisthesis | |||
| Double levels | 0.200 (0.011, 3.592) | 0.275 | NA |
| Single level | 0.761 (0.376, 1.542) | 0.449 | 67.3 |
| Single/multilevel levels | 0.462 (0.102, 2.086) | 0.315 | NA |
| Complications | |||
| Overall | 1.770 (1.485, 2.110) | <0.001 | 40.6 |
| Sensitivity analysis | 1.770 (1.485, 2.110) | ||
| Wound infection | |||
| Overall | 1.887 (0.631, 5.649) | 0.256 | 0 |
| Sensitivity analysis | 1.887 (0.631, 5.649) | ||
| Stroke | |||
| Overall | 0.562 (0.098, 3.237) | 0.519 | 22.6 |
| Sensitivity analysis | 0.562 (0.098, 3.237) | ||
| Sepsis | |||
| Overall | 2.120 (0.837, 5.371) | 0.113 | 0 |
| Sensitivity analysis | 2.120 (0.837, 5.371) | ||
| Pneumonia | |||
| Overall | 1.345 (0.610, 2.966) | 0.463 | 0 |
| Sensitivity analysis | 1.345 (0.610, 2.966) | ||
| Pulmonary embolism | |||
| Overall | 2.655 (0.822, 8.572) | 0.103 | 0 |
| Sensitivity analysis | 2.655 (0.822, 8.572) | ||
| Deep vein thrombosis | |||
| Overall | 1.372 (0.671, 2.808) | 0.386 | 0 |
| Sensitivity analysis | 1.372 (0.671, 2.808) | ||
| ODI | |||
| Overall | −2.569 (−6.548, 1.409) | 0.206 | 83.3 |
| Sensitivity analysis | −2.569 (−6.548, 1.409) | ||
| Level of spondylolisthesis | |||
| Multilevel levels | 2.300 (−1.122, 5.722) | 0.188 | NA |
| Single level | −3.768 (−9.063, 1.528) | 0.163 | 85.6 |
| Quality | |||
| HQ | −5.336 (−13.256, 2.584) | 0.187 | 92.7 |
| LQ | 1.337 (−1.530, 4.203) | 0.361 | 0 |
| Follow-up | |||
| 1 year | −0.675 (−5.519, 4.169) | 0.785 | 62.5 |
| 2 years | −4.491 (−13.091, 4.108) | 0.306 | 91.8 |
| Operative time | |||
| Overall | 51.037 (13.743, 88.330) | 0.007 | 98.6 |
| Sensitivity analysis | 51.037 (13.743, 88.330) | ||
| Quality | |||
| HQ | 32.940 (9.823, 56.058) | 0.005 | 85.4 |
| LQ | 76.182 (−39.456, 191.819) | 0.197 | 99.6 |
| Level of spondylolisthesis | |||
| Single/double levels | 64.500 (42.412, 86.588) | <0.001 | NA |
| Single level | 56.109 (−24.556, 136.774) | 0.173 | 99.2 |
| Double levels | 23.260 (19.101, 27.419) | <0.001 | NA |
| Bleeding | |||
| Overall | 258.354 (150.468, 366.239) | <0.001 | 96.7 |
| Sensitivity analysis | 258.354 (150.468, 366.239) | ||
| Quality | |||
| HQ | 247.917 (124.054, 371.780) | <0.001 | 97.8 |
| LQ | 300.600 (173.004, 428.196) | <0.001 | NA |
| Level of spondylolisthesis | |||
| Single/double levels | 459.200 (334.603, 583.797) | <0.001 | NA |
| Single level | 189.856 (−6.744, 386.457) | 0.058 | 89 |
| Double levels | 239.970 (229.613, 250.327) | <0.001 | NA |
| LOS | |||
| Overall | 3.838 (−2.172, 9.848) | 0.211 | 99.2 |
| Sensitivity analysis | 3.838 (−2.172, 9.848) | ||
| Quality | |||
| HQ | 5.524 (−0.612, 11.661) | 0.078 | 93.8 |
| LQ | 0.700 (0.467, 0.933) | <0.001 | NA |
| Level of spondylolisthesis | |||
| Single level | 4.586 (−3.058, 12.230) | 0.24 | 99.6 |
| Double levels | 2.230 (−0.694, 5.154) | 0.135 | NA |
| VAS | 0.000 (−0.258, 0.258) | 1 | NA |
ODI, Oswestry Disability Index; HQ, high quality; LQ, low quality; RR, relative risk; WMD, weighted mean difference; CI, confidence interval; LOS, length of stay; VAS, visual analog scale; NA, not applicable.
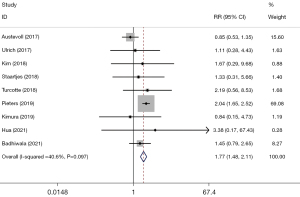
Complications
A total of 9 studies were included to evaluate the difference in complications between the two groups. Fixed effect model analysis results demonstrated that the complication rate of the FU group was higher than that of the DA group (I2=40.6%, RR: 1.770, 95% CI: 1.485 to 2.110, P<0.001) (Table 2, Figure 3). With respect to the specific complications, including wound infection (RR: 1.887, 95% CI: 0.631 to 5.649, P=0.256), stroke (RR: 0.562, 95% CI: 0.098 to 3.237, P=0.519), sepsis (RR: 2.120, 95% CI: 0.837 to 5.371, P=0.113), pneumonia (RR: 1.345, 95% CI: 0.610 to 2.966, P=0.463), pulmonary embolism (RR: 2.655, 95% CI: 0.822 to 8.572, P=0.103), and deep vein thrombosis (RR: 1.372, 95% CI: 0.671 to 2.808, P=0.386), there was no difference between the FU and DA groups (Table 2).
ODI
There were no significant differences found in ODI between the two groups (I2=83.3%, WMD: −2.569, 95% CI: −6.548 to 1.409, P=0.206) in the four articles. We also conducted subgroup analyses according to the article quality, level of spondylolisthesis, and follow-up time. Notably, no statistically significant differences between the two groups were observed across any of the above subgroups (Table 2).
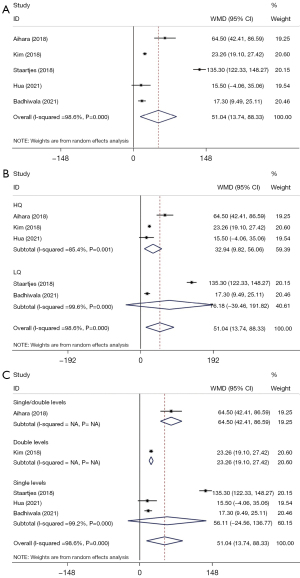
Operative time
Operative time (mins) between the two groups was compared in five studies, and the results demonstrated that the patients in the FU group had significantly longer operative time than those in the DA group (I2=98.6%, WMD: 51.037, 95% CI: 13.743 to 88.330), P=0.007) (Table 2, Figure 4A). According to the subgroup analyses based on the quality of the study, the operation time of the FU group was longer than that of the DA group in high-quality studies (WMD: 32.940, 95% CI: 9.823 to 56.058, P=0.005) (Table 2, Figure 4B). Depending on the level of spondylolisthesis, decompression plus fusion was associated with a longer of operative time in patients with double levels of spondylolisthesis (WMD: 23.260, 95% CI: 19.101 to 27.419, P<0.001) and in those with single/double levels of spondylolisthesis (WMD: 64.500, 95% CI: 42.412 to 86.588, P<0.001) (Table 2, Figure 4C).
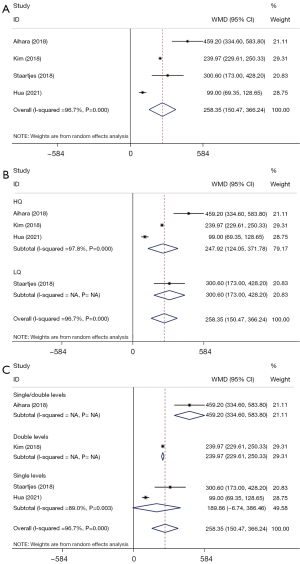
Bleeding
The amount of bleeding (mL) was reported in four studies, and results demonstrated that more blood loss occurred in the FU group than in the DA group (I2=96.7%, WMD: 258.354, 95% CI: 150.468 to 366.239, P<0.001) (Table 2, Figure 5A). Concerning the differences in study quality, the same results were observed both in high quality (I2=97.8%, WMD: 247.917, 95% CI: 124.054 to 371.780, P<0.001) and low quality (WMD: 300.600, 95% CI: 173.004 to 428.196, P<0.001) studies (Table 2, Figure 5B). Based on the level of spondylolisthesis, the FU group had a larger amount of bleeding when the levels of spondylolisthesis were double levels (I2=89.0%, WMD: 239.970, 95% CI: 229.613 to 250.327, P<0.001) and single/double levels (WMD: 459.200, 95% CI: 334 to 603,583.797, P<0.001) (Table 2, Figure 5C).
LOS
Three studies mentioned LOS (days). The results of the heterogeneity test showed I2=99.2%, so the random effects model was used for analysis. No statistically significant difference was identified between the two groups (WMD: 3.838, 95% CI: −2.172 to 9.848, P=0.211). Based on the subgroup analysis, the FU group had longer LOS among low quality studies (WMD: 0.700, 95% CI: 0.467 to 0.933, P<0.001) (Table 2).
Visual analog scales
A study by Kimura et al. (25) showed that no significant differences were found between the two groups in terms of preoperative and postoperative VAS. Hua et al. (14) reported that there was no statistical difference in VAS score between the experimental group and the control group (WMD: 0.000, 95% CI: −0.258 to 0.258, P=1.000) (Table 2).
Sensitivity analysis
Sensitivity analysis was conducted by sequentially omitting one study to explore the robustness and reliability of the overall estimated results. The sensitivity analysis confirmed the robustness and reliability of the meta-analysis results in this study (Table 2).
Discussion
The present study aimed to explore the effectiveness of decompression alone compared with additional fusion for patients with LSS + DS. A total of 14,693 patients were enrolled in the 12 included studies consisting of 11,598 cases in the DA group and 3,095 in the FU group. Our study demonstrated that the FU group had a higher complication rate, longer operative time, and more blood loss than the DA group, whereas no statistical differences were found in terms of overall reoperation rate, LOS, and ODI between the two groups. These results suggested that the efficacy of decompression alone may be superior to that of decompression plus fusion regarding the complication rate, operative time, and amount of bleeding among LSS + DS patients.
According to our results, there was no difference in the overall reoperation rate between decompression alone and decompression plus fusion, with subgroup analyses further performed. Xu et al. found a 13% reoperation rate during the follow-up time (36 months), the proximity of 10.90% in the DA group and 5.71% in the FU group, and no difference was observed between the two groups (28). Furthermore, in Ghogawala et al.’s study, also no statistically significant difference was found in the reoperation rate during the 4 years of follow-up among patients undergoing decompression-alone and those with decompression plus fusion (34% vs. 14%) (6), with both P values greater than 0.05, which was in accordance with the studies covered by this meta-analysis (6,21,23,24). More studies are required to confirm this result.
The application of decompression alone could also reduce the incidence of complications including acute myocardial infarct, pulmonary embolism, respiratory failure, and pneumonia in LSS + DS patients (29). Our study showed that decompression with fusion led to a higher rate of complications than decompression alone for the patients. A study further confirmed our findings that laminectomy plus fusion had a higher complication rate than laminectomy alone (21). The reasons may be that decompression plus fusion required more extensive dissection, decortication of bone, and longer operative time, and would cause more infections that were involved in the placement of implants or osteosynthesis materials (29,30).
As an important functional activity and motion persistence indicator, we used the ODI to evaluate the degree of disability and assess the quality of life in patients with back pain at a lumbosacral junction or leg pain (31). In our meta-analysis, the results showed that ODI did not differ significantly between the two groups, even in subgroup analyses. Hua et al. (14) found that the postoperative mean ODI scores decreased significantly in both lumbar endoscopic unilateral laminotomy bilateral decompression group and minimally invasive transforaminal lumbar interbody fusion group. In contrast to our findings, a previous study demonstrated that the ODI scores of decompression with fusion were 3.5 times that of decompression alone in patients with LSS with/without DS (32). Based on these results, we cannot assert the superiority and inferiority of decompression alone or with fusion in terms of ODI; further studies are needed to conform or refute our findings.
Fusion, as a complex invasive surgical method, could also lead to a longer duration of operation and more blood loss, especially in elderly patients (7). Chang et al. indicated in their study that patients receiving decompression with fusion experienced prolonged operation time and lost more blood, which is in line with our results (33). In the present study, subgroup analyses were performed and affirmed the overall result, which may be explained by that the degree of spondylolisthesis could influence the outcome of patients undergoing decompression without fusion. Conversely, LOS was not found to be statistically different within a 2-year follow-up period between the two groups among LSS with or without grade I DS patients (33). This was most likely attributed to less surgical dissection after laminectomy or other decompression in small target populations.
There were some strengths to the current study: (I) a considerable number of patients were included, which would improve the validity and reliability of our outcomes; (II) subgroup analyses were performed based on the different study designs, the article quality, levels of spondylolisthesis, and to further explore the efficacy and safety of decompression alone and decompression plus fusion. However, several limitations remained: (I) the relatively low- or moderate-quality of 8 included studies, in which various decompression types as well as fusion treatments were used, may have reduced the statistical power to some extent; (II) not involving the clinical satisfaction, cost-utility, and post-operative walking distance; (III) lack of evidence on radiographic findings that may have affected objective evaluation; (IV) absence of publication bias, due to the fact that the inclusion of studies was fewer than 9 of each indicator of our study, not conforming to the standard of publication bias assessment; (V) most included cohort studies did not adjust for propensity score, which may have influenced the results; and (VI) as in other observational studies included, possible presence of selection biases and unexplained confounding factors may have an impact on our findings; (VII) moreover, a language bias was generated due to non-English language databased being searched. More prospective high-quality articles are needed in the future to further compare the efficacy and safety of decompression and decompression plus fusion.
Conclusions
Decompression alone may be superior in the complication rate, operative time, LOS, and amount of blood loss to decompression plus fusion. Additional studies are needed to further verify the long-term outcomes of decompression alone as a surgical choice, which was also the anticipation of our study.
Acknowledgments
Funding: This study was supported by the Sanitary Research Servicing Capacity Promoting Project of Jilin Province (No. 2019SCI 041) and Jilin Provincial Health and Health Technology Innovation Program, China (No. 2020J045).
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2208/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2208/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang C, Yin X, Zhang L, et al. Posterolateral fusion combined with posterior decompression shows superiority in the treatment of severe lumbar spinal stenosis without lumbar disc protrusion or prolapse: a retrospective cohort study. J Orthop Surg Res 2020;15:26. [Crossref] [PubMed]
- Minamide A, Simpson AK, Okada M, et al. Microendoscopic Decompression for Lumbar Spinal Stenosis With Degenerative Spondylolisthesis: The Influence of Spondylolisthesis Stage (Disc Height and Static and Dynamic Translation) on Clinical Outcomes. Clin Spine Surg 2019;32:E20-6. [Crossref] [PubMed]
- Zhang J, Liu TF, Shan H, et al. Decompression Using Minimally Invasive Surgery for Lumbar Spinal Stenosis Associated with Degenerative Spondylolisthesis: A Review. Pain Ther 2021;10:941-59. [Crossref] [PubMed]
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016;352:h6234. [Crossref] [PubMed]
- Bydon M, Alvi MA, Goyal A. Degenerative Lumbar Spondylolisthesis: Definition, Natural History, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am 2019;30:299-304. [Crossref] [PubMed]
- Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus Fusion versus Laminectomy Alone for Lumbar Spondylolisthesis. N Engl J Med 2016;374:1424-34. [Crossref] [PubMed]
- Kuo CC, Merchant M, Kardile MP, et al. In Degenerative Spondylolisthesis, Unilateral Laminotomy for Bilateral Decompression Leads to Less Reoperations at 5 Years When Compared to Posterior Decompression With Instrumented Fusion: A Propensity-matched Retrospective Analysis. Spine (Phila Pa 1976) 2019;44:1530-7. [Crossref] [PubMed]
- Joelson A, Nerelius F, Holy M, et al. Reoperations after decompression with or without fusion for L4-5 spinal stenosis with or without degenerative spondylolisthesis: a study of 6,532 patients in Swespine, the national Swedish spine register. Acta Orthop 2021;92:264-8. [Crossref] [PubMed]
- Badhiwala JH, Leung SN, Jiang F, et al. In-hospital Course and Complications of Laminectomy Alone Versus Laminectomy Plus Instrumented Posterolateral Fusion for Lumbar Degenerative Spondylolisthesis: A Retrospective Analysis of 1804 Patients from the NSQIP Database. Spine (Phila Pa 1976) 2021;46:617-23. [Crossref] [PubMed]
- Kleinstueck FS, Fekete TF, Mannion AF, et al. To fuse or not to fuse in lumbar degenerative spondylolisthesis: do baseline symptoms help provide the answer? Eur Spine J 2012;21:268-75. [Crossref] [PubMed]
- Martin CR, Gruszczynski AT, Braunsfurth HA, et al. The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine (Phila Pa 1976) 2007;32:1791-8. [Crossref] [PubMed]
- Aihara T, Toyone T, Murata Y, et al. Degenerative Lumbar Spondylolisthesis with Spinal Stenosis: A Comparative Study of 5-Year Outcomes Following Decompression with Fusion and Microendoscopic Decompression. Asian Spine J 2018;12:132-9. [Crossref] [PubMed]
- Austevoll IM, Gjestad R, Brox JI, et al. The effectiveness of decompression alone compared with additional fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a pragmatic comparative non-inferiority observational study from the Norwegian Registry for Spine Surgery. Eur Spine J 2017;26:404-13. [Crossref] [PubMed]
- Hua W, Wang B, Ke W, et al. Comparison of Clinical Outcomes Following Lumbar Endoscopic Unilateral Laminotomy Bilateral Decompression and Minimally Invasive Transforaminal Lumbar Interbody Fusion for One-Level Lumbar Spinal Stenosis With Degenerative Spondylolisthesis. Front Surg 2020;7:596327. [Crossref] [PubMed]
- Glassman SD, Carreon LY, Dimar JR, et al. Clinical outcomes in older patients after posterolateral lumbar fusion. Spine J 2007;7:547-51. [Crossref] [PubMed]
- Wells G, Shea BJ, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Ottawa Hospital Research Institute 2014. Available online: https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis
- Newman PH. Spondylolisthesis, its cause and effect. Ann R Coll Surg Engl 1955;16:305-23. [PubMed]
- Junghanns H. Spondylolisthesen ohne spalt im Zwishengelenkstuck. Arch Orthop Unfall-Chir 1930;29:118-27. [Crossref]
- Macnab I. Spondylolisthesis with an intact neural arch: the so-called pseudo-spondylolisthesis. J Bone Joint Surg Br 1950;32:325-33. [Crossref] [PubMed]
- Newman PH, Stone KH. The etiology of spondylolisthesis. J Bone Joint Surg Br 1963;45:39-59. [Crossref]
- Ulrich NH, Burgstaller JM, Pichierri G, et al. Decompression Surgery Alone Versus Decompression Plus Fusion in Symptomatic Lumbar Spinal Stenosis: A Swiss Prospective Multicenter Cohort Study With 3 Years of Follow-up. Spine (Phila Pa 1976) 2017;42:E1077-86. [Crossref] [PubMed]
- Turcotte JJ, Patton CM. Predictors of Postoperative Complications After Surgery for Lumbar Spinal Stenosis and Degenerative Lumbar Spondylolisthesis. J Am Acad Orthop Surg Glob Res Rev 2018;2:e085. [Crossref] [PubMed]
- Staartjes VE, Schröder ML. Effectiveness of a Decision-Making Protocol for the Surgical Treatment of Lumbar Stenosis with Grade 1 Degenerative Spondylolisthesis. World Neurosurg 2018;110:e355-61. [Crossref] [PubMed]
- Pieters TA, Li YI, Towner JE, et al. Comparative Analysis of Decompression Versus Decompression and Fusion for Surgical Management of Lumbar Spondylolisthesis. World Neurosurg 2019;125:e1183-8. [Crossref] [PubMed]
- Kimura R, Yoshimoto M, Miyakoshi N, et al. Comparison of Posterior Lumbar Interbody Fusion and Microendoscopic Muscle-preserving Interlaminar Decompression for Degenerative Lumbar Spondylolisthesis With >5-Year Follow-up. Clin Spine Surg 2019;32:E380-5. [Crossref] [PubMed]
- Kim CH, Chung CK, Kim MJ, et al. Increased Volume of Surgery for Lumbar Spinal Stenosis and Changes in Surgical Methods and Outcomes: A Nationwide Cohort Study with a 5-Year Follow-Up. World Neurosurg 2018;119:e313-22. [Crossref] [PubMed]
- Ghogawala Z, Benzel EC, Amin-Hanjani S, et al. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative Grade I spondylolisthesis. J Neurosurg Spine 2004;1:267-72. [Crossref] [PubMed]
- Xu S, Wang J, Liang Y, et al. Decompression with fusion is not in superiority to decompression alone in lumbar stenosis based on randomized controlled trials: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2019;98:e17849. [Crossref] [PubMed]
- Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259-65. [Crossref] [PubMed]
- Deyo RA, Martin BI, Ching A, et al. Interspinous spacers compared with decompression or fusion for lumbar stenosis: complications and repeat operations in the Medicare population. Spine (Phila Pa 1976) 2013;38:865-72. [Crossref] [PubMed]
- Ruiz FK, Bohl DD, Webb ML, et al. Oswestry Disability Index is a better indicator of lumbar motion than the Visual Analogue Scale. Spine J 2014;14:1860-5. [Crossref] [PubMed]
- Ahmed SI, Javed G, Bareeqa SB, et al. Comparison of Decompression Alone Versus Decompression with Fusion for Stenotic Lumbar Spine: A Systematic Review and Meta-analysis. Cureus 2018;10:e3135. [Crossref] [PubMed]
- Chang W, Yuwen P, Zhu Y, et al. Effectiveness of decompression alone versus decompression plus fusion for lumbar spinal stenosis: a systematic review and meta-analysis. Arch Orthop Trauma Surg 2017;137:637-50. [Crossref] [PubMed]



