
Age, gender, geographic and clinical differences for gallstones in China: a nationwide study
Introduction
Cholelithiasis is a common disease, caused by abnormally high levels of cholesterol or bilirubin in bile in the biliary tract or gallbladder (1). The gallstone disease, usually indicating the occurrence of symptoms or complications caused by gallstones, is a costly gastrointestinal disorder leading to the hospital admission (2). According to the anatomical location of the disease, gallstones are classified into following classes: gallbladder stones (GB stones, or cholecystolithiasis) and bile-duct stones, which can be subdivided into extrahepatic duct stones (EHD stones, mostly common bile duct stones) and intrahepatic duct stones (IHD stones, or hepatolithiasis). Treatment strategies, biomedical components, pathophysiology, and associated factors are thought to be distinct for different gallstone subtypes (3,4).
Gallstone diseases affect nearly 20% of the population in Western countries (3,5,6). The prevalence of gallstones increases with age, and reaches as high as 57% in women at the age of seventies (7). Besides, there are substantial geographical and racial variations in gallstone prevalence (5,8-13). It has been reported that GB stones are predominant in the western populations, accounting for 90–95% of all gallstone cases (3), while IHD stones are more prevalent in Southeastern Asia, mainland of China and Taiwan (4,14). Moreover, common bile duct stones are much more prevalent in Asia, suggesting that the common bile duct stone is the leading associated factor for cholangiocarcinoma in several studies (15-17). However, above data was collected and reviewed by different diagnosis methods. It’s a need to confirm whether prevalence of the gallstones may be varied by its anatomical location, age, gender, geographic and metabolic factors using standardized methods. Therefore, we conducted this nationwide epidemiological study on gallstone diseases using a standardized research protocol in Chinese population.
Previous studies have revealed a large number of exogenous associated factors for cholesterol stones, including metabolic syndrome, various medications, inappropriate dietary, and factors causing gallbladder hypomotility or increasing enterohepatic bilirubin cycling (1). Nevertheless, there were few studies based on a large population to screen specific associated factors of gallstones at different anatomical locations. Herein, we also investigated prevalence and associated factors of gallstones across almost all China provinces in 2017. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-21-6186/rc).
Methods
Study participants
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Peking University (PU IRB, IRB00001052-19077) and individual consent for this retrospective analysis was waived. A total of 13,178,313 participants underwent the health checkup from January 1st to December 31st, 2017 at one of the Meinian Onehealth Healthcare clinics, who owns 323 clinics covering 30 provinces in mainland China (expect for Tibet). Since abdominal ultrasonography is included in routine health checkup in China, gallstone diseases with no symptom would be detected and recorded. Therefore, the available health checkup records provide basic information for the epidemiological study on gallstone diseases. Participants who were aged under 18, or with missing data on key characteristics including the gender and age were excluded (n=291,418). Participants who did not receive abdominal ultrasonography, or whose ultrasonography diagnosis could not be confirmed, were also excluded (n=1,941,477). It should be noted that there were 115,273 participants who had undergone cholecystectomy before the year 2017, and they were not included when analyzing the prevalence of GB stones. There were 10,937,993 participants included in the final analysis.
Examinations and diagnostic criteria
The health examination was conducted by professional/licensed clinicians according to the standardized protocol. Briefly, all participants underwent the health examination with an empty stomach in the morning. Peripheral blood was collected with the anticoagulant and tested by the automatic biochemical analyzer (all approved by authority) to measure the fasting glucose and total triglyceride. The ultrasonography scanner (all approved by authority) was used in abdominal ultrasonographic examinations and gallstones appeared as specific echogenic foci with distal hypoechoic shadows, and GB stones could move upon the participant’s position. Gallstones were sub-grouped according to their anatomical locations. The body weight and height was measured with light clothes and no shoes.
Statistical analysis
Stratified analysis was conducted for GB stones, IHD stones, EHD stones or without any type of gallstones. The distribution of age, sex, body mass index (BMI), geographic area, city scale, fasting glucose and total triglyceride of each subgroup was presented independently. The age- and gender-standardized prevalence (AGS-prevalence) was calculated according to the data of China sixth census population 2010 using direct standardization method. The AGS-prevalence of gallstone diseases was stratified by BMI and other factors. The age-standardized prevalence was calculated for specific genders, and the sex-standardized prevalence was calculated for specific age groups. Differences between subgroups were evaluated by χ2 test. Logistic regression analysis was performed to explore the association between gallstone diseases and BMI, fasting glucose, total triglyceride, and previous cholecystectomy, with covariates of the age and sex. Data was analyzed using SAS software (version 9.4). Continuous variables were represented as mean ± SD, and categorical variables were represented as frequency (%). A P value <0.05 was considered to be significant.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting, or dissemination plans of our research.
Results
Characteristics of the study participants
This study included a total of 10,937,993 participants (53.4% men and 46.6% women) with a mean age of 41.4 years old (Table 1). There were higher percentages of participants with ages 30–39 and less >70 in this study population, compared to the national consensus (Figure 1A) (18,19). Overall, GB stones were the most common gallstone subtype in Chinese population, accounting for 76.33% of all cases, while IHD and EHD stones made up to 24.31% and 0.22% respectively (concomitant cases were present) (Table 2). Apparent disparities were noted among gallstone subtypes by anatomical locations in the gender, age, geographic area, city scale, metabolic factors (including BMI, fasting glucose level, total triglyceride level), as well as a history of cholecystectomy (Table 1).
Table 1
| Characteristics | Total participants | Without gallstone | Gallstone | ||
|---|---|---|---|---|---|
| GB stones | IHD stones | EHD stones | |||
| Participants | 10,937,993 | 10,420,999 | 394,647 | 125,704 | 1,159 |
| Gender, n (%) | |||||
| Male | 5,838,763 (53.4) | 5,579,024 (53.5) | 194,827 (49.4) | 66,710 (53.1) | 460 (39.7) |
| Female | 5,099,230 (46.6) | 4,841,975 (46.5) | 199,820 (50.6) | 58,994 (46.9) | 699 (60.3) |
| Age group, n (%) | |||||
| Mean age | 41.4±13.3 | 41.1±13.2 | 50.3±13.6 | 42.1±13.6 | 55.4±14.7 |
| <30 years | 2,831,549 (25.9) | 2,772,333 (26.2) | 29,126 (7.4) | 30,341 (24.1) | 59 (5.1) |
| 30–50 years | 5,097,296 (46.6) | 4,878,422 (46.8) | 161,096 (40.8) | 59,130 (47.0) | 336 (29.0) |
| 50–70 years | 2,699,016 (24.7) | 2,498,387 (24.0) | 170,234 (43.1) | 31,831 (25.3) | 572 (49.4) |
| ≥70 years | 310,132 (2.8) | 271,857 (2.6) | 34,191 (8.7) | 4,402 (3.5) | 192 (16.6) |
| Geographic area*, n (%) | |||||
| East China | 3,182,666 (29.1) | 3,056,247 (29.3) | 105,661 (26.8) | 21,245 (16.9) | 266 (23.0) |
| Southwest China | 1,426,113 (13.0) | 1,355,101 (13.0) | 63,841 (16.2) | 7,261 (5.8) | 282 (24.3) |
| Central China | 1,633,907 (14.9) | 1,537,550 (14.8) | 63,887 (16.2) | 33,585 (26.7) | 209 (18.0) |
| South China | 1,542,632 (14.1) | 1,466,417 (14.1) | 44,584 (11.3) | 32,351 (25.7) | 104 (9.0) |
| North China | 1,369,685 (12.5) | 1,322,131 (12.7) | 44,557 (11.3) | 3,000 (2.4) | 110 (9.5) |
| Northeast China | 1,041,154 (9.5) | 974,963 (9.4) | 40,637 (10.3) | 26,499 (21.1) | 79 (6.8) |
| Northwest China | 741,836 (6.8) | 708,590 (6.8) | 31,480 (8.0) | 1,763 (1.4) | 109 (9.4) |
| City scale†, n (%) | |||||
| Small or medium sized city | 2,733,213 (25.0) | 2,587,171 (24.8) | 111,341 (28.2) | 35,806 (28.5) | 435 (37.5) |
| Large city | 4,557,380 (41.7) | 4,359,040 (41.8) | 157,615 (39.9) | 41,794 (33.2) | 398 (34.3) |
| Mega city and above | 3,647,400 (33.3) | 3,474,788 (33.3) | 125,691 (31.8) | 48,104 (38.3) | 326 (28.1) |
| BMI (kg/m2), n (%) | |||||
| ≤18.50 | 464,574 (4.3) | 452,423 (4.3) | 6,285 (1.6) | 5,933 (4.7) | 39 (3.4) |
| 18.5–24.9 | 5,541,018 (50.7) | 5,309,719 (51.0) | 161,836 (41.0) | 71,097 (56.6) | 607 (52.4) |
| 25.0–29.9 | 3,006,047 (27.5) | 2,835,096 (27.2) | 143,237 (36.3) | 28,791 (22.9) | 322 (27.8) |
| ≥30 | 545,393 (5.0) | 511,261 (4.9) | 31,236 (7.9) | 3,052 (2.4) | 41 (3.5) |
| Unknown | 1,380,961 (12.6) | 1,312,500 (12.6) | 52,053 (13.2) | 16,831 (13.4) | 150 (12.9) |
| Fasting glucose (mmol/L), n (%) | |||||
| <7 | 9,955,196 (91.0) | 9,496,421 (91.1) | 345,523 (87.6) | 116,246 (92.5) | 1,023 (88.3) |
| ≥7 | 448,941 (4.1) | 409,821 (3.9) | 35,682 (9.0) | 3,680 (2.9) | 97 (8.4) |
| Unknown | 533,856 (4.9) | 514,757 (4.9) | 13,442 (3.4) | 5,778 (4.6) | 39 (3.4) |
| Total triglyceride (mmol/L), n (%) | |||||
| <2.27 | 8,793,655 (80.4) | 8,382,363 (80.4) | 307,679 (78.0) | 106,438 (84.7) | 954 (82.3) |
| ≥2.27 | 1,573,226 (14.4) | 1,486,178 (14.3) | 74,111 (18.8) | 13,374 (10.6) | 169 (14.6) |
| Unknown | 571,112 (5.2) | 552,458 (5.3) | 12,857 (3.3) | 5,892 (4.7) | 36 (3.1) |
| Previous cholecystectomy, n (%) | |||||
| No | 10,822,273 (98.9) | 10,307,553 (98.9) | 394,200 (99.9) | 124,132 (98.8) | 871 (75.2) |
| Yes | 115,720 (1.1) | 113,446 (1.1) | 447 (0.11) | 1,572 (1.3) | 288 (24.8) |
*, seven geographical regions of China: https://www.chinacheckup.com/blogs/articles/regions-of-china; †, according to the new standards in 2014, urban population are more than 10 million for megacity behemoth, 5–10 million for mega city, 1–5 million for large city (3–5 million for type I large city, 1–3 million for type II large city), 0.5–1 million for the medium-sized city, less than 0.5 million for small city (0.2–0.5 million for type I small city, less than 0.2 million for the type II small city). The city size is divided according to the sixth census in 2010 (18,19). BMI, body mass index; GB, gall bladder; IHD, intrahepatic bile duct; EHD, extrahepatic bile duct.
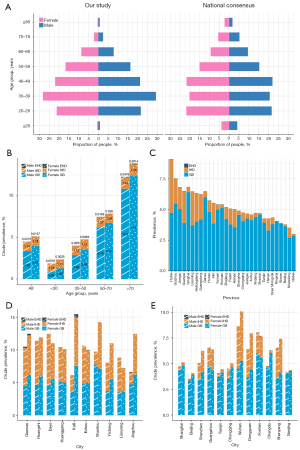
Table 2
| Characteristics | Gallstone | GB stones | IHD stones | EHD stones | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Crude prevalence (%) | Standardized prevalence* (%) | N | Crude prevalence (%) | Standardized prevalence (%) | N | Crude prevalence (%) | Standardized prevalence (%) | N | Crude prevalence (‱) | Standardized prevalence (‱) | ||||
| Overall | 516,994 | 4.73 (4.71–4.74) | 5.13 (5.11–5.14) | 394,647 | 3.65 (3.64–3.66) | 4.09 (4.08–4.10) | 125,704 | 1.15 (1.14–1.16) | 1.16 (1.15–1.17) | 1,159 | 1.06 (1.00–1.12) | 1.36 (1.27–1.45) | |||
| Age group, years | |||||||||||||||
| <30 | 59,216 | 2.09 (2.07–2.11) | 2.11 (2.09–2.13) | 29,126 | 1.03 (1.02–1.04) | 1.05 (1.03–1.06) | 30,341 | 1.07 (1.06–1.08) | 1.07 (1.06–1.09) | 59 | 0.21 (0.16–0.26) | 0.21 (0.16–0.27) | |||
| 30–50 | 218,874 | 4.29 (4.28–4.31) | 4.31 (4.30–4.33) | 161,096 | 3.18 (3.17–3.20) | 3.20 (3.19–3.22) | 59,130 | 1.16 (1.15–1.17) | 1.16 (1.15–1.17) | 336 | 0.66 (0.59–0.73) | 0.67 (0.60–0.74) | |||
| 50–70 | 200,629 | 7.43 (7.40–7.46) | 7.44 (7.41–7.47) | 170,234 | 6.45 (6.42–6.48) | 6.46 (6.43–6.49) | 31,831 | 1.18 (1.17–1.19) | 1.18 (1.16–1.19) | 572 | 2.12 (1.95–2.29) | 2.14 (1.96–2.31) | |||
| ≥70 | 38,275 | 12.3 (12.2–12.5) | 12.4 (12.3–12.6) | 34,191 | 11.5 (11.4–11.6) | 11.6 (11.5–11.7) | 4,402 | 1.42 (1.38–1.46) | 1.42 (1.37–1.46) | 192 | 6.19 (5.32–7.07) | 6.43 (5.51–7.35) | |||
| P value | <0.001 | <0.001 | <0.001 | <0.001 | |||||||||||
| Gender | |||||||||||||||
| Male | 259,739 | 4.45 (4.43–4.47) | 4.85 (4.83–4.87) | 194,827 | 3.36 (3.35–3.38) | 3.79 (3.77–3.81) | 66,710 | 1.14 (1.13–1.15) | 1.16 (1.15–1.17) | 460 | 0.79 (0.72–0.86) | 1 (0.90–1.10) | |||
| Female | 257,255 | 5.04 (5.03–5.06) | 5.41 (5.38–5.43) | 199,820 | 3.97 (3.95–3.99) | 4.39 (4.37–4.42) | 58,994 | 1.16 (1.15–1.17) | 1.16 (1.15–1.17) | 699 | 1.37 (1.27–1.47) | 1.72 (1.57–1.86) | |||
| P value | <0.001 | <0.001 | 0.026 | <0.001 | |||||||||||
| BMI, kg/m2 | |||||||||||||||
| ≤18.50 | 12,151 | 2.62 (2.57–2.66) | 3.94 (3.84–4.04) | 6,285 | 1.36 (1.32–1.39) | 2.58 (2.50–2.66) | 5,933 | 1.28 (1.24–1.31) | 1.43 (1.38–1.48) | 39 | 0.84 (0. 58–1.10) | 1.98 (1.23–2.73) | |||
| 18.5–24.99 | 231,299 | 4.17 (4.16–4.19) | 4.67 (4.65–4.69) | 161,836 | 2.95(2.93–2.96) | 3.48 (3.46–3.50) | 71,097 | 1.28 (1.27–1.29) | 1.30 (1.29–1.31) | 607 | 1.10 (1.01–1.18) | 1.45 (1.32–1.59) | |||
| 25.0–29.99 | 170,951 | 5.69 (5.66–5.71) | 5.75 (5.72–5.78) | 143,237 | 4.84 (4.81–4.86) | 4.95 (4.92–4.98) | 28,791 | 0.96 (0.95–0.97) | 0.96 (0.94–0.97) | 322 | 1.07 (0.95–1.19) | 1.28 (1.12–1.44) | |||
| ≥30 | 34,132 | 6.26 (6.19–6.32) | 6.91 (6.82–7.00) | 31,236 | 5.82 (5.76–5.88) | 6.52 (6.44–6.61) | 3,052 | 0.56 (0.54–0.58) | 0.60 (0.58–0.63) | 41 | 0.75 (0.52–0.98) | 0.87 (0.57–1.18) | |||
| P value | <0.001 | <0.001 | 0.099 | <0.001 | |||||||||||
| Fasting glucose, mmol/L | |||||||||||||||
| <7 | 458,775 | 4.61 (4.60–4.62) | 5.04 (5.03–5.06) | 345,523 | 3.51 (3.49–3.52) | 3.98 (3.96–3.99) | 116,246 | 1.17 (1.16–1.17) | 1.18 (1.17–1.19) | 1,023 | 1.03 (0.96–1.09) | 1.35 (1.26–1.45) | |||
| ≥7 | 39,120 | 8.71 (8.63–8.80) | 6.85 (6.72–6.99) | 35,682 | 8.15 (8.07–8.23) | 6.39 (6.26–6.52) | 3,680 | 0.82 (0.79–0.85) | 0.66 (0.62–0.71) | 97 | 2.16 (1.73–2.59) | 1.35 (1.05–1.65) | |||
| Unknown | 19,099 | 3.58 (3.53–3.63) | 4.67 (4.59–4.76) | 13,442 | 2.54 (2.49–2.58) | 3.65 (3.57–3.73) | 5,778 | 1.08 (1.05–1.11) | 1.13 (1.09–1.17) | 39 | 0.73 (0.50–0.96) | 1.34 (0.80–1.89) | |||
| P value | <0.001 | <0.001 | <0.001 | <0.001 | |||||||||||
| Total triglyceride, mmol/L | |||||||||||||||
| <2.27 | 411,292 | 4.68 (4.66–4.69) | 5.07 (5.05–5.08) | 307,679 | 3.53 (3.52–3.55) | 3.97 (3.95–3.98) | 106,438 | 1.21 (1.20–1.22) | 1.22 (1.21–1.23) | 954 | 1.08 (1.02–1.15) | 1.38 (1.28–1.48) | |||
| ≥2.27 | 87,048 | 5.53 (5.50–5.57) | 5.83 (5.78–5.89) | 74,111 | 4.78 (4.75–4.82) | 5.13 (5.08–5.19) | 13,374 | 0.85 (0.84–0.86) | 0.86 (0.84–0.88) | 169 | 1.07 (0.91–1.24) | 1.31 (1.05–1.57) | |||
| Unknown | 18,654 | 3.27 (3.22–3.31) | 4.9 (4.80–5.00) | 12,857 | 2.26 (2.22–2.30) | 3.86 (3.77–3.95) | 5,892 | 1.03 (1.01–1.06) | 1.14 (1.09–1.18) | 36 | 0.63 (0.42–0.84) | 1.23 (0.66–1.80) | |||
| P value | <0.001 | <0.001 | <0.001 | 0.005 | |||||||||||
| City scale | |||||||||||||||
| Small or medium sized city | 146,042 | 5.34 (5.32–5.37) | 5.25 (5.22–5.28) | 111,341 | 4.13 (4.10–4.15) | 4.08 (4.05–4.11) | 35,806 | 1.31 (1.30–1.32) | 1.29 (1.28–1.31) | 435 | 1.59 (1.44–1.74) | 1.75 (1.57–1.93) | |||
| Large city | 198,340 | 4.35 (4.33–4.37) | 4.75 (4.73–4.78) | 157,615 | 3.50 (3.48–3.51) | 3.93 (3.91–3.96) | 41,794 | 0.92 (0.91–0.93) | 0.93 (0.92–0.94) | 398 | 0.87 (0.79–0.96) | 1.13 (1.00–1.26) | |||
| Mega city and above | 172,612 | 4.73 (4.71–4.75) | 5.57 (5.54–5.60) | 125,691 | 3.48 (3.46–3.50) | 4.39 (4.36–4.41) | 48,104 | 1.32 (1.31–1.33) | 1.32 (1.30–1.33) | 326 | 0.89 (0.80–0.99) | 1.31 (1.15–1.48) | |||
| P value | <0.001 | <0.001 | <0.001 | <0.001 | |||||||||||
*, standardized prevalence: the age-standardized and gender-standardized prevalence was calculated according to data of China sixth census population 2010 using direct standardization method. Age-standardized prevalence was calculated for specific gender, sex-standardized prevalence was calculated for specific age group. BMI, body mass index; GB, gall bladder; IHD, intrahepatic bile duct; EHD, extrahepatic bile duct.
Prevalence of gallstones
Among Chinese adults (≥18 years old), the crude prevalence of gallstones was 4.73%, and the AGS-prevalence was 5.13% (95% CI: 5.11–5.14%) (Table 2). The AGS-prevalence of GB stones, IHD stones and EHD stones was 4.09%, 1.16% and 0.0136%, respectively.
The prevalence of gallstones, regardless of the anatomical locations, significantly increased with the age (P<0.001), especially for the GB stones whose prevalence increased from 1.05% (age <30) to 11.60% (age ≥70) (P<0.001), and for the EHD stones whose prevalence increased from 0.21% (age <30) to 6.43% (age ≥70) (P<0.001) (Table 2, Figure 1B). Furthermore, a gender disparity was clearly noted in the AGS-prevalence of GB and EHD stones, which was higher in women than that in men (4.39% vs. 3.79% and 1.72% vs. 1.00% respectively, P<0.001), whereas the disparity in IHD stones is minimal (P<0.05) (Table 2). More interestingly, although the prevalence of GB stones increased with a higher BMI, fasting glucose level or total triglyceride level and EHD stones increased with a higher fasting glucose level or total triglyceride level, the prevalence of IHD stones for individuals with BMI ≥25.0, fasting glucose ≥7 or total triglyceride level ≥2.27 was decreased. The prevalence of any gallstone subtypes varied among different city scales (P<0.001) and the prevalence of gallstone diseases was the lowest consistently among all three subtypes in individuals from large cities.
Regional differences on the prevalence of gallstones
Next, we evaluated the impact of geographic and regional differences on the disease prevalence. The provinces with the highest AGS-prevalence of gallstones were Hubei (8.86%), Guizhou (7.01%), Jiangxi (6.67%), Guangxi (6.41%), and Liaoning (6.36%), while the provinces with the lowest gallstones’ AGS-prevalence were Hebei (3.00%), Shandong (3.50%) and Beijing (3.72%) (Figure 1C). Among top 5 provinces, IHD stones accounted for 28–51% of all gallstones, which was dramatically higher than the average level of 24.3% nationwide (Table S1). Similarly, IHD stones accounted for around 50% of all gallstones in top 10 cities with the highest crude prevalence of all gallstones (Figure 1D). More interestingly, the crude prevelance of IHD stones varied among top 12 cities with the largest population in China from 0.07% to 4.46%, whereas the crude prevelance of GB stones was around 4% in all 12 cities (Figure 1E).
Associated factors for gallstones at different anatomical locations
We then performed the multivariate logistic regression analysis of odds ratios (ORs) of the age, gender, metabolic syndrome related associated factors (BMI, fasting glucose level, and total triglyceride level) and a history of previous cholecystectomy to assess their associations with gallstones at different anatomical locations (Table 3). We observed that the age was a strong associated factor of GB stones and EHD stones while to a less extend for IHD stones (Figure 2). Male gender was a protective factor for GB stones and EHD stones (OR <1), but it was a associated factor for IHD stones [OR =1.1 (1.09, 1.11)].
Table 3
| Characteristics | Overall | GB stones | IHD stones | EHD stones | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (%) | OR (95% CI) | Cases (%) | OR (95% CI) | Cases (%) | OR (95% CI) | Cases (‱) | OR (95% CI) | ||||
| Age, years | |||||||||||
| <30 | 45,614 (2.1) | Ref | 22,455 (1.0) | Ref | 23,356 (1.1) | Ref | 46 (0.2) | Ref | |||
| 30–50 | 175,090 (4.3) | 1.97 (1.95–2.00) | 129,567 (3.2) | 2.83 (2.79–2.87) | 46,614 (1.1) | 1.14 (1.12–1.16) | 258 (0.6) | 2.88 (2.10–3.96) | |||
| 50–70 | 166,089 (7.4) | 3.39 (3.36–3.43) | 141,343 (6.4) | 5.49 (5.42–5.57) | 25,907 (1.2) | 1.21 (1.19–1.23) | 476 (2.1) | 8.1 (5.93–11.06) | |||
| ≥70 | 29,958 (12.2) | 6.07 (5.98–6.16) | 26,825 (11.4) | 10.51 (10.32–10.70) | 3,361 (1.4) | 1.42 (1.37–1.47) | 152 (6.2) | 19.28 (13.70–27.12) | |||
| Gender | |||||||||||
| Women | 208,979 (5.1) | Ref | 163,163 (4.0) | Ref | 47,075 (1.1) | Ref | 568 (1.4) | Ref | |||
| Men | 207,772 (4.5) | 0.83 (0.82–0.83) | 157,027 (3.4) | 0.77 (0.76–0.77) | 52,163 (1.1) | 1.10 (1.09–1.11) | 364 (0.8) | 0.67 (0.58–0.76) | |||
| BMI, kg/m2 | |||||||||||
| ≤18.50 | 10,987 (2.7) | Ref | 5,776 (1.4) | Ref | 5,272 (1.3) | Ref | 37 (0.9) | Ref | |||
| 18.5–24.99 | 214,212 (4.2) | 1.23 (1.21–1.26) | 151,047 (3.0) | 1.50 (1.46–1.54) | 64,645 (1.3) | 0.96 (0.93–0.99) | 565 (1.1) | 0.75 (0.54–1.05) | |||
| 25.0–29.99 | 159,759 (5.7) | 1.52 (1.49–1.55) | 134,210 (4.9) | 2.14 (2.08–2.20) | 26,535 (1.0) | 0.72 (0.69–0.74) | 295 (1.1) | 0.57 (0.40–0.81) | |||
| ≥30 | 31,793 (6.3) | 1.77 (1.73–1.81) | 29,157 (5.9) | 2.77 (2.69–2.85) | 2,786 (0.6) | 0.43 (0.41–0.45) | 35 (0.7) | 0.39 (0.24–0.62) | |||
| Fasting glucose, mmol/L | |||||||||||
| <7 | 384,599 (4.6) | Ref | 290,841 (3.5) | Ref | 96,246 (1.1) | Ref | 853 (1.0) | Ref | |||
| ≥7 | 32,152 (8.6) | 1.31 (1.30–1.33) | 29,349 (8.1) | 1.41 (1.39–1.43) | 2,992 (0.8) | 0.77 (0.74–0.79) | 79 (2.1) | 1.14 (0.90–1.44) | |||
| Total triglyceride, mmol/L | |||||||||||
| <2.27 | 344,889 (4.6) | Ref | 258,737 (3.5) | Ref | 88,473 (1.2) | Ref | 798 (1.1) | Ref | |||
| ≥2.27 | 71,862 (5.5) | 1.02 (1.01–1.02) | 61,453 (4.8) | 1.09 (1.08–1.10) | 10,765 (0.8) | 0.77 (0.76–0.79) | 134 (1.0) | 0.89 (0.74–1.07) | |||
| Previous cholecystectomy | |||||||||||
| No | 414,797 (4.8) | Ref | 319,817 (3.7) | – | 97,870 (1.1) | Ref | 689 (0.8) | Ref | |||
| Yes | 1,954 (2.0) | 0.27 (0.25–0.28) | 373 (100.0) | – | 1,368 (1.4) | 1.27 (1.21–1.34) | 243 (24.9) | 17.98 (15.42–20.97) | |||
*, logistic model was used by adjusting age (<30, 30–50, 50–70, ≥70 years old), gender (men, women), BMI (≤18.50, 18.5–24.99, 25.0–29.99, ≥30 kg/m2), fasting glucose (<7, ≥7 mmol/L), total triglyceride (<2.27, ≥2.27 mmol/L), and previous cholecystectomy (no, yes). BMI, body mass index; OR, odds ratio; GB, gall bladder; IHD, intrahepatic bile duct.

Moreover, individuals with a higher BMI [OR =1.77 (1.73, 1.81) for BMI ≥30.0], fasting glucose level [OR =1.31 (1.30, 1.33)] and total triglyceride level [OR =1.02 (1.01, 1.02)] had substantially higher odds ratios of gallstones. This is concurrent with the strong associations of these factors with GB stones. In contrast, participants with a higher BMI showed lower odds ratios of IHD [OR =0.43 (0.41, 0.45) for BMI ≥30.0] and EHD stones [OR =0.39 (0.24, 0.62) for BMI ≥30.0]. The level of fasting glucose ≥7 mmol/L [OR =0.77 (0.74, 0.79)] or total triglyceride ≥2.27 mmol/L [OR =0.77 (0.76, 0.79)] were weak protective factors for developing IHD stones but not associated with the EHD stone formation (Table 3). A history of cholecystectomy was positively associated with the incidence of bile duct stones, especially with EHD stones [OR =17.98 (15.42, 20.97)], but not with GB stones (Table 3).
Discussion
In this cross-sectional study with 10,937,993 participants covered all provinces in mainland China except for Tibet, the AGS-prevalence of all gallstone cases was 5.13%, increased from 4.3% reported in 2008 (13). Different from the previous study in 2008 showing that the age standardized prevalence of gallstones was slightly higher in men (4.4%) than that in women (4.3%) (13), we found that the AGS-prevalence of overall gallstones was higher in women (5.41% vs. 4.85%). Our results are in line with previous studies from other parts of Asia, Europe and USA (5,20-23).
The risk factors for gallstone in China and Western countries may be very different. Unlike the western population where 90–95% of gallstones were formed at the gallbladder (3), approximately 25% of gallstone cases in Chinese population were located in the IHD, which was suggested to be related to the chronic biliary track infestation (8). In consistent with findings from other studies (9,10,22), the female gender, oldness and metabolic disorders, as represented by a higher BMI, fasting glucose or total triglycerides, were strongly correlated with GB stones, but not with IHD stones. Instead, the prevalence of IHD stones was even higher in people with a lower BMI, fasting glucose or total triglycerides level. Moreover, the AGS-prevalence of GB stones and IHD stones was not correlated among 30 provinces. On the contrary, AGS-prevalence of GB and EHD stones was highly correlated among 30 provinces (Spearman test, r=0.77, P<0.05), suggesting that EHD stones were prone to be concomitant with GB stones, or resulting from the passage of stones from the gallbladder to the extrahepatic bile duct.
Furthermore, the incidence of gallstone diseases in China was suggested to be correlated with significant regional differences in a few single-center based or single-city based studies (15,16,20-24). For most provinces in mainland China, no previous data was available on the prevalence of gallstones as a reference, including ones demonstrating the highest prevalence in our study. We presented that the prevalence of gallstone diseases in China varies substantively across geographic regions, due to the inconsistent economic status and life style. Among all three gallstone subtypes, the percentage of IHD gallstones in all gallstone cases was considerably correlated with the overall AGS-prevalence of gallstones across different regions. This study revealed that a higher proportion of IHD stones links to a higher burden of gallstone disease among different provinces of China. As such, health policies aimed at specifically eliminating the risk factors for IHD stones might potentially reduce the national disease burden of gallstones in China.
Taken together, our nationwide study herein provided an update on the prevalence of gallstone diseases by anatomical locations in China. Nevertheless, the majority of participants included in this study were from urban areas of China and sampling deviation may exist. In addition, because of the extremely large sample size, questionnaire was not applied and therefore, some potential associated factors were not investigated, such as smoking, alcohol intake, ethnicity, family history and underlying chronic diseases (11,25,26). Lastly, although we found IHD stones shared few associated factors with GB stones, additional case control or cohort studies are required to determine and validate risk factors for IHD stones in China.
Conclusions
The prevalence of gallstones in China largely varied by anatomical locations, demographic factors, geographic locations and metabolic factors, suggesting that etiology of each subtype may be different. Further investigation should be conducted. Evidence-based public health policy strategized on the basis of epidemiological studies will greatly help to reduce the national disease burden of the gallstone disease.
Acknowledgments
We thank the participants who volunteered to participate in this study. We also thank Prof. Simon C. Robson for his assistance with the manuscript revision.
Funding: This research was funded by International Science and Technology Cooperation Projects (Nos. 2016YFE0107100 and 2015DFA30650), CAMS Clinical and Translational Medicine Research Funds (No. 2019XK320006), CAMS Innovation Fund for Medical Science (CIFMS) (Nos. 2017-I2M-4-003 and 2018-I2M-3-001), Capital Special Research Project for Health Development (No. 2014-2-4012), Beijing Natural Science Foundation (NOs. L172055 and 7192158), the Fundamental Research Funds for the Central Universities (No. 3332018032), and National Ten-thousand Talent Program.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-21-6186/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-21-6186/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-21-6186/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Peking University (PU IRB, IRB00001052-19077) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lammert F, Gurusamy K, Ko CW, et al. Gallstones. Nat Rev Dis Primers 2016;2:16024. [Crossref] [PubMed]
- Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: Liver, biliary tract, and pancreas. Gastroenterology 2009;136:1134-44. [Crossref] [PubMed]
- European Association for the Study of the Liver. Electronic address eee. EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 2016;65:146-81. [Crossref] [PubMed]
- Tazuma S, Unno M, Igarashi Y, et al. Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol 2017;52:276-300. [Crossref] [PubMed]
- Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am 2010;39:157-69. vii. [Crossref] [PubMed]
- Ruhl CE, Everhart JE. Gallstone disease is associated with increased mortality in the United States. Gastroenterology 2011;140:508-16. [Crossref] [PubMed]
- Volzke H, Baumeister SE, Alte D, et al. Independent risk factors for gallstone formation in a region with high cholelithiasis prevalence. Digestion 2005;71:97-105. [Crossref] [PubMed]
- Shaffer EA. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol 2006;20:981-96. [Crossref] [PubMed]
- Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology 2009;136:376-86. [Crossref] [PubMed]
- Everhart JE, Yeh F, Lee ET, et al. Prevalence of gallbladder disease in American Indian populations: findings from the Strong Heart Study. Hepatology 2002;35:1507-12. [Crossref] [PubMed]
- Everhart JE, Khare M, Hill M, et al. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999;117:632-9. [Crossref] [PubMed]
- Chen YC, Chiou C, Lin MN, et al. The prevalence and risk factors for gallstone disease in taiwanese vegetarians. PLoS One 2014;9:e115145. [Crossref] [PubMed]
- Zeng Q, He Y, Qiang DC, et al. Prevalence and epidemiological pattern of gallstones in urban residents in China. Eur J Gastroenterol Hepatol 2012;24:1459-60. [Crossref] [PubMed]
- Tsui WM, Chan YK, Wong CT, et al. Hepatolithiasis and the syndrome of recurrent pyogenic cholangitis: clinical, radiologic, and pathologic features. Semin Liver Dis 2011;31:33-48. [Crossref] [PubMed]
- Cai H, Kong WT, Chen CB, et al. Cholelithiasis and the risk of intrahepatic cholangiocarcinoma: a meta-analysis of observational studies. BMC Cancer 2015;15:831. [Crossref] [PubMed]
- Lee BS, Cha BH, Park EC, et al. Risk factors for perihilar cholangiocarcinoma: a hospital-based case-control study. Liver Int 2015;35:1048-53. [Crossref] [PubMed]
- Welzel TM, Mellemkjaer L, Gloria G, et al. Risk factors for intrahepatic cholangiocarcinoma in a low-risk population: a nationwide case-control study. Int J Cancer 2007;120:638-41. [Crossref] [PubMed]
- Qi W, Liu S, Jin H. Applicability of the new standard of city-size classification in China. Prog Geogr 2016;35:47-56.
- Fang C. A review of Chinese urban development policy, emerging patterns and future adjustments. Geographical Research 2014;33:674-86.
- Gu Q, Zhou G, Xu T. Risk factors for gallstone disease in Shanghai: An observational study. Medicine (Baltimore) 2020;99:e18754. [Crossref] [PubMed]
- Zhu L, Aili A, Zhang C, et al. Prevalence of and risk factors for gallstones in Uighur and Han Chinese. World J Gastroenterol 2014;20:14942-9. [Crossref] [PubMed]
- Sun H, Tang H, Jiang S, et al. Gender and metabolic differences of gallstone diseases. World J Gastroenterol 2009;15:1886-91. [Crossref] [PubMed]
- Song ST, Shi J, Wang XH, et al. Prevalence and risk factors for gallstone disease: A population-based cross-sectional study. J Dig Dis 2020;21:237-45. [Crossref] [PubMed]
- Nakayama F, Koga A, Ichimiya H, et al. Hepatolithiasis in East Asia: comparison between Japan and China. J Gastroenterol Hepatol 1991;6:155-8. [Crossref] [PubMed]
- Walcher T, Haenle MM, Mason RA, et al. The effect of alcohol, tobacco and caffeine consumption and vegetarian diet on gallstone prevalence. Eur J Gastroenterol Hepatol 2010;22:1345-51. [Crossref] [PubMed]
- Shebl FM, Andreotti G, Meyer TE, et al. Metabolic syndrome and insulin resistance in relation to biliary tract cancer and stone risks: a population-based study in Shanghai, China. Br J Cancer 2011;105:1424-9. [Crossref] [PubMed]


