Incidence and mortality of lung cancer in 2018 and the temporal trends from 2010 to 2018 in Henan province, China: a population-based registry study
Introduction
Lung cancer ranks the second most common cancer and the first leading cause of cancer deaths worldwide, with an estimated 2.2 million new cases and 1.8 million deaths in 2020 (1). China is one of the countries with the highest burden of lung cancer. According to the latest cancer statistics released by the National Cancer Center, there were about 82.8 thousand new cases and 65.7 thousand deaths from lung cancer in 2016 in China, ranking it 1st in terms of both incidence and death (2). It was also estimated that the national incidence and mortality of lung cancer increased in the past two decades, and would increase in the next decade without intervention (3). Therefore, it is great of significance to develop and perfect prevention and control strategies to curb the epidemic of lung cancer. However, the burden of lung cancer varies greatly in different regions (2). Thus, it is critical to figure its epidemiologic features in different regions to provide evidence that can be used to formulate targeted intervention measures.
Henan province is located in central China, accounting for 7.4% of the national population. In recent decades, socioeconomic and lifestyle changed greatly in Henan, as well as the development of oncology health services. For example, health education on the prevention and control for lung cancer were carried out every year and screening program has been launched in urban people at high risk of lung cancer since 2013, in Henan province. Data on the current incidence and mortality of lung cancer and the temporal trend in the past decades are important for effective prevention and control.
Therefore, this study sought to examine the latest statistics for the incidence and mortality of lung cancer in Henan province in 2018 and explore the temporal trends from 2010 to 2018. This up-to-date provincial cancer profile should provide a scientific basis for lung cancer prevention and control in Henan province. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4029/rc).
Methods
Data source
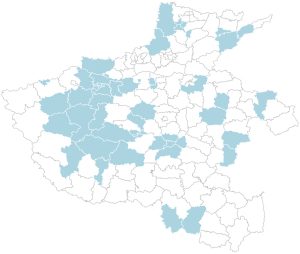
This was a population-based registry study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Cancer registries are used to continuously and dynamically monitor the incidence and mortality of cancer (4). In Henan province, records of cancer are first submitted to local cancer registries by the hospitals and medical institutions, and then submitted to the Henan Provincial Central Cancer Registry of China (HNCCR) by the local cancer registries. All the newly diagnosed lung cancer cases were coded from C33.0 to C34.9 according to the International Statistical Classification of Diseases 10th Revision. At the end of 2021, a total of 42 cancer registries had submitted registration data for 2018 to the HNCCR. After quality check, three local cancer registries (Gushi, Anyang, and Xinxiang counties) were excluded due to the lack of completeness. Finally, the data from 39 registries (10 from urban areas and 29 from rural areas) were qualified and included in the analysis database. Totally, 33,271,234 (male: 17,055,226 and female: 16,216,008) population were covered by these cancer registries, accounting for 30.51% of the provincial registered residence population at the end of 2018 (Figure 1).
The provincial data of registered residence population from 2010 to 2018 were estimated according to the Statistical Bulletin on National Economic and Social Development of Henan Province over these years in relation to the different areas (urban/rural), sex (male/female), and age groups (0–<1, 1–4, 5–9, 10–14, …, 75–79, 80–84, and 85+ years).
Quality control
The HNCCR is responsible for data quality and comparability control as per the criteria set out in the “Chinese Guideline for Cancer Registration” and “Cancer Incidence in Five Continents Volume IX” by the International Agency for Research on Cancer (5-7). Indexes including the mortality-to-incidence (M/I) ratio, the percentage of cancer cases with an unknown basis (UB%), the percentage of death-certificate-only cases (DCO%), and the percentage of morphological verification (MV%), were adopted to assess the completeness, comparability, and validity of the cancer registration data. The M/I was usually 0.6–0.8, while <0.6 indicating that death may have been underreported, and >0.8 indicating that the incidence may have been underreported. Moreover, the incidence and mortality of cancers were also checked year by year to ensure them didn’t fluctuate drastically. In summary, the total M/I ratio, UB%, DCO%, and MV% of the Henan lung cancer database in 2018 were 0.76, 0%, 2.05%, and 64.89%, respectively. In urban areas, the M/I ratio, UB%, DCO%, and MV% were 0.76, 0%, 2.52%, and 70.64%, respectively. In rural areas, the M/I ratio, UB%, DCO%, and MV% were 49%, 0%, 0.88%, and 81.91%, respectively.
Outcomes and measurement
The main outcomes and measurement reported in this study are as follows:
(I) Incidence and mortality rates
Crude incidence, crude mortality, and age-standardized rates adjusted by the Chinese standard population in 2000 and the world Segi’s population were estimated. Rates are expressed per 100,000 of the population, and 2 decimal digits are retained after an integer. The following formula was used:
(II) Proportion
Proportional distribution indicates the site-specific percentage level of incident cases (deaths) compared to the total cases (deaths) recorded, which reflects the hazard of certain cancer to human health. The formula used to calculate the proportion of lung cancer was as follows:
(III) Cumulative rate
A cumulative incidence or mortality rate indicates the probability of cancer onset between birth and a specific age. Generally, the age of 74 years is used as the specific age for cancer. The following formula was used:
Statistical analysis
The pooled qualified data were grouped by area (urban/rural), sex (male/female), and age groups (0–, 1–4, 5–9, 10–14, …, 75–79, 80–84, and 85+ years). The incidence, mortality, proportions, and cumulative rates for population aged 0 to 74 years were calculated. The estimated numbers of new cases and deaths from lung cancer in 2018 were calculated, using the age-specific rates multiplied by the corresponding estimated provincial age-specific population. Joinpoint regression analyses were performed to explore temporal trends in the age-standardized incidence rate by world standard (Segi’s) population (ASIRW) and the age-standardized mortality rate by world standard (Segi’s) population (ASMRW) from 2010 to 2018 stratified by area and sex, and the crude incidence and mortality rates from 2010 to 2018 stratified by area and age group (15–39, 40–74, and 75+ years). We assumed that the error variance was constant, and we did not log-transform our data. All the models were restricted to a maximum of 1 jointpoint. We estimated the annual percentage change (APC), the average annual percentage change (AAPC), and the 95% confidence interval (CI) for each segment. SAS software (Version 9.4, SAS Institute Inc., Cary, USA) was used for the statistical analysis.
Results
Estimated incidence of lung cancer in 2018
The estimated numbers of new cases, incidence, proportions and cumulative rates (0–74 years) for lung cancer by area and sex are shown in Table 1. Overall, there were an estimated of 55,344 new cases of lung cancer (37,280 males and 18,064 females) in 2018 in Henan province, of which 32.04% (17,730) occurred in urban areas, and 67.96% (37,614) occurred in rural areas. Lung cancer was the most common cancer in both men and women, accounting for 19.37% of all new cancers. The overall crude incidence rate was 50.75/100,000, the age-standardized incidence rate by Chinese standard population (ASIRC) was 37.05/100,000, the ASIRW was 37.14/100,000, and the cumulative rate was 4.57%. The ASIRW in urban areas was 1.01 folds as that in rural areas, and in males, it was 2.24 folds as that in females.
Table 1
| Area | Sex | No. of cases | Crude incidence (1/100,000) | Proportion (%) | ASIRC (1/100,000) | ASIRW (1/100,000) | Cumulative rate, 0–74 (%) |
|---|---|---|---|---|---|---|---|
| All | Total | 55,344 | 50.75 | 19.37 | 37.05 | 37.14 | 4.57 |
| Male | 37,280 | 65.88 | 24.94 | 51.66 | 51.84 | 6.43 | |
| Female | 18,064 | 34.43 | 13.25 | 23.10 | 23.14 | 2.70 | |
| Urban | Total | 17,730 | 52.22 | 18.56 | 37.05 | 37.32 | 4.56 |
| Male | 11,880 | 68.24 | 23.93 | 51.59 | 52.05 | 6.41 | |
| Female | 5,850 | 35.37 | 12.75 | 23.51 | 23.61 | 2.76 | |
| Rural | Total | 37,614 | 50.08 | 19.77 | 37.06 | 37.07 | 4.57 |
| Male | 25,400 | 64.83 | 25.45 | 51.70 | 51.74 | 6.44 | |
| Female | 12,214 | 33.99 | 13.51 | 22.92 | 22.93 | 2.67 |
ASIRC, age-standardized incidence rates by Chinese standard population; ASIRW, age-standardized incidence rates by world standard population (Segi’s).
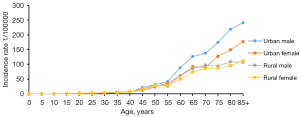
The age-specific incidence of lung cancer by area and sex is shown in Figure 2. The incidence of lung cancer increased with age in Henan province in 2018. It was relatively low in the 0–39-year age group, then increased dramatically and reached its peak in the 85+ years age group for both sexes. The pattern was similar between urban and rural areas. In the above 40-year age groups, the incidence was higher in males than females in both urban and rural areas.
Estimated mortality of lung cancer in 2018
The estimated numbers of lung cancer deaths, mortality, proportions and cumulative rates (among patients aged 0–74 years old) by area and sex are set out in Table 2. Overall, about 41,782 people died from lung cancer (29,124 males and 12,658 females) in 2018 in Henan province, of which 32.17% (13,443) occurred in urban areas, 67.83% (28,339) occurred in rural areas. Lung cancer was the 1st-leading cause of cancer deaths in both men and women, accounting for 24.83% of all cancer deaths. The overall crude mortality rate was 38.31/100,000, the age-standardized mortality rate by Chinese standard population (ASMRC) was 26.97/100,000, the ASMRW was 27.09/100,000, and the cumulative rate was 3.22%. The ASMRW in urban areas was 1.01 folds as that in rural areas, and in males, it was 2.62 folds as that in females.
Table 2
| Area | Sex | No. of cases | Crude mortality (1/100,000) | Proportion (%) | ASMRC (1/100,000) | ASMRW (1/100,000) | Cumulative rate, 0–74 (%) |
|---|---|---|---|---|---|---|---|
| All | Total | 41,782 | 38.31 | 24.83 | 26.97 | 27.09 | 3.22 |
| Male | 29,124 | 51.46 | 28.33 | 39.73 | 39.83 | 4.75 | |
| Female | 12,658 | 24.12 | 19.34 | 15.04 | 15.22 | 1.69 | |
| Urban | Total | 13,443 | 39.60 | 25.66 | 27.12 | 27.32 | 3.19 |
| Male | 9,515 | 54.65 | 29.32 | 40.78 | 40.96 | 4.82 | |
| Female | 3,928 | 23.75 | 19.69 | 14.60 | 14.86 | 1.61 | |
| Rural | Total | 28,339 | 37.73 | 24.46 | 26.92 | 27.00 | 3.24 |
| Male | 19,609 | 50.05 | 27.87 | 39.25 | 39.31 | 4.73 | |
| Female | 8,730 | 24.30 | 19.18 | 15.26 | 15.41 | 1.73 |
ASMRC, age-standardized mortality rates by Chinese standard population; ASMRW, age-standardized mortality rates by world standard population (Segi’s).
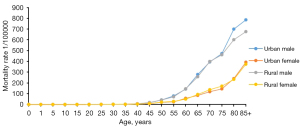
The age-specific mortality rates for lung cancer by area and sex are set out Figure 3. The lung cancer mortality rate increased with age in Henan province in 2018. It was relatively low in the 0–44-year age group, then increased dramatically and reached its peak in the 85+ years age group for both sexes. The pattern was similar between urban and rural areas. In the above 45-year age group, males had a higher mortality rate than females in both urban and rural areas.
Trends in lung cancer incidence and mortality from 2010 to 2018
The trends of ASIRW and ASMRW for lung cancer by area and sex are set out in Table 3 and Table S1. The overall ASIRW and ASMRW of lung cancer in Henan province remained stable, but both decreased in urban areas from 2014 to 2018 (ASIRW: APC =–4.7%, 95% CI: –8.2% to –1.1%, P=0.023; ASMRW: APC =–5.3%, 95% CI: –8.5% to –2.0%, P=0.012). Given the differences between area and sex, the population was further divided into four subgroups (urban males, urban females, rural males, and rural females). The ASIRW and ASMRW decreased in urban males from 2014 to 2018 (ASIRW: APC =–6.2%, 95% CI: –10.7% to –1.4%, P=0.023; ASMRW: APC =–6.5%, 95% CI: –7.8% to –5.1%, P=0.021), but remained stable in urban females, rural males and rural females from 2010 to 2018.
Table 3
| Area | Sex | Trend 1 | Trend 2 | Trend | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | P | Years | APC (95% CI) | P | 2010–2018 AAPC (95% CI) | P | ||||
| ASIRW | |||||||||||
| All | Total | 2010–2018 | 0.3 (−0.8–1.4) | 0.531 | 0.3 (−0.8–1.4) | 0.531 | |||||
| Male | 2010–2014 | 2.2 (−0.1–4.5) | 0.056 | 2014–2018 | −1.1 (−4.0–1.9) | 0.339 | 0.7 (−1.3–2.8) | 0.481 | |||
| Female | 2010–2018 | −0.1 (−1.8–1.7) | 0.937 | −0.1 (−1.8–1.7) | 0.937 | ||||||
| Urban | Total | 2010–2014 | 2.2 (−1.6–6.1) | 0.183 | 2014–2018 | −4.7 (−8.2 to −1.1) | 0.023 | −1.3 (−3.2–0.5) | 0.158 | ||
| Male | 2010–2014 | 3.1 (−1.8–8.4) | 0.158 | 2014–2018 | −6.2 (−10.7 to −1.4) | 0.023 | −1.6 (−4.0–0.8) | 0.190 | |||
| Female | 2010–2018 | −1.0 (0.1 to −2.1) | 0.072 | −1.0 (0.1 to −2.1) | 0.072 | ||||||
| Rural | Total | 2010–2018 | 0.6 (−0.7–1.9) | 0.287 | 0.6 (−0.7–1.9) | 0.287 | |||||
| Male | 2010–2018 | 0.8 (−0.5–2.0) | 0.186 | 0.8 (−0.5–2.0) | 0.186 | ||||||
| Female | 2010–2018 | 0.1 (−2.1–2.3) | 0.905 | 0.1 (−2.1–2.3) | 0.905 | ||||||
| ASMRW | |||||||||||
| All | Total | 2010–2018 | −0.2 (−1.5–1.0) | 0.687 | −0.2 (−1.5–1.0) | 0.687 | |||||
| Male | 2010–2018 | −0.1 (−1.1–1.0) | 0.904 | −0.1 (−1.1–1.0) | 0.904 | ||||||
| Female | 2010–2018 | 0.0 (−1.7–1.8) | 0.968 | 0.0 (−1.7–1.8) | 0.968 | ||||||
| Urban | Total | 2010–2014 | 0.3 (−3.1–3.9) | 0.799 | 2014–2018 | −5.3 (−8.5 to −2.0) | 0.012 | −2.5 (−4.2 to −0.8) | 0.004 | ||
| Male | 2010–2014 | 0.6 (−1.2–2.4) | 0.386 | 2014–2018 | −6.5 (−7.8 to −5.1) | 0.021 | −2.7 (−5.3 to −0.1) | 0.042 | |||
| Female | 2010–2018 | −0.7 (−1.6–0.2) | 0.121 | −0.7 (−1.6–0.2) | 0.121 | ||||||
| Rural | Total | 2010–2018 | 0.3 (−1.2–1.7) | 0.670 | 0.3 (−1.2–1.7) | 0.670 | |||||
| Male | 2010–2018 | 0.4 (−0.8–1.6) | 0.431 | 0.4 (−0.8–1.6) | 0.431 | ||||||
| Female | 2010–2018 | 0.2 (−2.0–2.4) | 0.865 | 0.2 (−2.0–2.4) | 0.865 | ||||||
ASIRW, age-standardized incidence rates by world standard population (Segi’s); ASMRW, age-standardized mortality rates by world standard population (Segi’s). APC, annual percentage change; AAPC, average annual percentage change.
The trends for the crude incidence and mortality rates for lung cancer by area and age are set out in Table 4 and Table S2. The incidence rate was increased in the population aged 75+ years old from 2010 to 2018, especially, among rural people (AAPC =4.2, 95% CI: 0.8–7.7, P=0.023), and was decreased in the urban population aged 40–74 years old (AAPC =–1.4, 95% CI: –2.3 to –0.4, P=0.013) from 2010 to 2018. The mortality rate was decreased in the urban population aged 40–74 years old (AAPC =–3.1, 95% CI: –4.2 to –1.9, P<0.001) from 2010 to 2018.
Table 4
| Area | Age | Trend 1 | Trend 2 | Trend | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | P | Years | APC (95% CI) | P | 2010–2018 AAPC (95% CI) | P | ||||
| Incidence | |||||||||||
| All | 15–39 | 2010–2018 | −0.9 (−3.4–1.7) | 0.440 | −0.9 (−3.4–1.7) | 0.440 | |||||
| 40–74 | 2010–2018 | 0.0 (−0.7–0.6) | 0.933 | 0.0 (−0.7–0.6) | 0.933 | ||||||
| 75+ | 2010–2018 | 3.4 (0.7–6.2) | 0.020 | 3.4 (0.7–6.2) | 0.020 | ||||||
| Urban | 15–39 | 2010–2018 | −4.8 (−9.8–0.5) | 0.069 | −4.8 (−9.8–0.5) | 0.069 | |||||
| 40–74 | 2010–2018 | −1.4 (−2.3 to −0.4) | 0.013 | −1.4 (−2.3 to −0.4) | 0.013 | ||||||
| 75+ | 2010–2014 | 6.5 (−1.7–15.5) | 0.093 | 2014–2018 | −1.24 (−26.8–4.9) | 0.111 | −0.2 (−4.7–4.6) | 0.931 | |||
| Rural | 15–39 | 2010–2018 | 0.1 (−2.9–3.3) | 0.917 | 0.1 (−2.9–3.3) | 0.917 | |||||
| 40–74 | 2010–2018 | 0.3 (−0.5–1.1) | 0.186 | 0.3 (−0.5–1.1) | 0.186 | ||||||
| 75+ | 2010–2018 | 4.2 (0.8–7.7) | 0.023 | 4.2 (0.8–7.7) | 0.023 | ||||||
| Mortality | |||||||||||
| All | 15–39 | 2010–2018 | 0.0 (−5.3–5.6) | 0.993 | 0.0 (−5.3–5.6) | 0.993 | |||||
| 40–74 | 2010–2018 | −0.5 (−1.5–0.6) | 0.348 | −0.5 (−1.5–0.6) | 0.348 | ||||||
| 75+ | 2010–2018 | 1.6 (−0.4–3.7) | 0.100 | 1.6 (−0.4–3.7) | 0.100 | ||||||
| Urban | 15–39 | 2010–2018 | −9.4 (−22.7–6.1) | 0.183 | −9.4 (−22.7–6.1) | 0.183 | |||||
| 40–74 | 2010–2018 | −3.1 (−4.2 to −1.9) | <0.001 | −3.1 (−4.2 to −1.9) | <0.001 | ||||||
| 75+ | 2010–2014 | 5.2 (−4.1–15.4) | 0.202 | 2014–2018 | −11.5 (−28.0–8.8) | 0.176 | −0.7 (−5.0–3.8) | 0.728 | |||
| Rural | 15–39 | 2010–2018 | 3.2 (−3.2–9.9) | 0.284 | 3.2 (−3.2–9.9) | 0.284 | |||||
| 40–74 | 2010–2018 | 0.2 (−1.1–1.6) | 0.733 | 0.2 (−1.1–1.6) | 0.733 | ||||||
| 75+ | 2010–2018 | 2.0 (0.0–4.1) | 0.051 | 2.0 (0.0–4.1) | 0.051 | ||||||
APC, annual percentage change; AAPC, average annual percentage change.
Discussion
Lung cancer is the most common cancer in China (2). In this study, we analyzed the incidence and mortality of lung cancer in 2018 and the temporal trends from 2010 to 2018 in Henan province, using data from 39 qualified cancer registries. It was estimated that about 55,344 new cases and 41,782 deaths of lung cancer occurred in Henan province in 2018. Lung cancer has the highest incidence and mortality rates among all cancers. Males had higher incidence and mortality rates than females in both urban and rural areas. The overall incidence and mortality rates were stable from 2010 to 2018, but decreased in urban areas from 2014 to 2018, particularly among males and people aged 40–74 years old. The updated statistics for incidence and mortality provide scientific evidence that can be used in the prevention and control of lung cancer.
The latest national lung cancer statistics still rely on data from 2016. We found that the age-standard mortality rate of Henan province was similar to that of the whole country, while the age-standard incidence rate of Henan province was higher (2016 ASIRW in the whole country: 36.46/100,000; 2016 ASIRW in Henan province: 37.51/100,000; 2018 ASIRW in Henan province: 37.14/100,000) (2). Many previous studies have suggested that smoking and air pollution are the main risk factors for lung cancer (8-10). A survey conducted in 2018 showed that the smoking rate of people aged 15–74 in Central China (27.42%) was higher than that of the whole country (26.59%) (11), which might be a reason for the higher incidence of lung cancer. Additionally, the air quality in Henan province is poor. According to the daily reported Air Quality Index data for 2019 (12), the continuous air pollution index of Henan province ranks among the top in China, which might be another reason for the higher incidence of lung cancer. Thus, effective tobacco control and air pollution control are urgently needed.
Previous studies have shown that both the incidence and mortality rates of lung cancer are higher in urban areas than that in rural areas, including Hunan, Fujian, and Jiangsu provinces (13-15). We also found that the gaps in the incidence and mortality rates of lung cancer between urban areas and rural areas gradually narrowed in Henan province, particularly after 2014. There may be 2 reasons for this situation. First, the “Cancer Screening Program in Urban China (CanSPUC)” was launched in Henan province among the urban population aged 40–74 years old in 2013, and those in the high-risk population for lung cancer in urban areas enrolled in CanSPUC were eligible for low-dose computed tomography (LDCT) screening, which has reduced the burden of lung cancer in urban areas to a certain extent (16). This study also indicated that both the incidence and mortality rates decreased in the urban population aged 40–74 years old from 2014 to 2018. Second, in the past, the detection rate of lung cancer in urban areas was higher than that in rural areas due to air pollution, more frequent physical examinations, and opportunistic screening (13-15). However, with the accelerating process of rural urbanization, and the continuous spread of industrialization to rural area, the burden of lung cancer in rural areas has increased (17-19). This study also showed that the AAPCs of lung cancer incidence and mortality rates in rural areas from 2010 to 2018 were >0, and these changes were statistically significant. Thus, it is recommended that health education, and lung cancer screening, early diagnosis, and early treatment should be carried out, particularly in rural areas.
Consistent with national research (2), in this study, the incidence and mortality rates of lung cancer in men were significantly higher than those in women. In Henan province, in 2018, the overall ASIRW of men was 2.24 times that of women, and the overall ASMRW was 2.62 times that of women. This may be related to different exposure levels of risk factors for lung cancer, such as smoking (20). We further observed significant downward trends in ASIRW and ASMRW in urban males from 2014 to 2018, but not in urban females. This may be partly because non-smoking females had a low participation rate in LDCT screenings (21); however, the lung cancer incidence rate increased among this population (2,22,23). Thus, more attention should be paid to non-smoking females, especially those exposed to high-risk factors for lung cancer, such as indoor cooking, passive smoking, and air pollution.
This study revealed that the incidence rate of lung cancer increased dramatically at the age of 40 years, and the mortality rate increased dramatically at the age of 45 years. A gap of only 5 years indicates that the prognosis for lung cancer is poor. Actually, the 5-year survival rate of lung cancer is closely related to the clinical stage. The 5-year survival rate of stage I can reach >90% (24), while that of stage IV is <5% (25). However, due to the non-specific nature of lung cancer, about 80% of the patients have progressed to the advanced stage at the time of diagnosis (26), leading to an overall 5-year survival rate of <20% (27,28). Thus, lung cancer screening, early diagnosis, and early treatment should be strengthened. In addition, the incidence of lung cancer in the population aged 75+ years old was increasing, particularly in rural areas. This may be related to the increased life expectancy of this population and screening inaccessibility. Under current guidelines in China, the last age for lung cancer screening is 74 years old (29). In the future, more health economics evaluation studies are needed to determine the optimal last age for lung cancer screening.
This study conducted a systematic examination of the most updated cancer data of Henan province. The Henan population accounted for 30.51% of the provincial registered residence population at the end of 2018. In particular, we reported the lung cancer incidence, mortality and temporal trends by area, sex, and age group. Such detailed information is useful in providing different perspectives for the prevention and control of lung cancer. This study had several limitations. First, the estimations in this analysis depended on the best available registry data rather than census data, which might have led to selection bias. Second, there was a lack of sufficient high-quality data in 3 registries, which may have affected the provincial estimation results.
Conclusions
In conclusion, lung cancer is the most common cancer and the 1st-leading cause of cancer-related deaths in Henan province. The overall incidence and mortality rates of lung cancer in Henan province were stable from 2010 to 2018, but decreased in urban areas from 2014 to 2018, particularly among males and people aged 40–74 years. Males had higher incidence and mortality rates than females. Smoking cessation intervention, lung cancer screening, early diagnosis and early treatment need to be strengthened. The burden of lung cancer among people aged 75+ years old has increased in Henan province; thus, the final age for lung cancer screening should probably be increased.
Acknowledgments
We gratefully acknowledge all the population-based cancer registries for their work in data collection, sorting, verification, and database creation.
Funding: This work was funded by Henan Province Medical Science and Technology Breakthrough Project (No. SBGJ202001004), and Henan Province Medical Science and Technology Project (No. RKX202102011).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4029/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4029/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent 2022;2:1-9. [Crossref]
- Fang Y, Li Z, Chen H, Zhang T, Yin X, Man J, et al. Burden of lung cancer along with attributable risk factors in China from 1990 to 2019, and projections until 2030. J Cancer Res Clin Oncol. 2022; [Crossref] [PubMed]
- Wei W, Zeng H, Zheng R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol 2020;21:e342-9. [Crossref] [PubMed]
- Jie H, Wanqing C. Chinese Guideline for Cancer Registration. Beijing: People’s Health Publishing House; 2016.
- Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer 2009;45:756-64. [Crossref] [PubMed]
- Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer 2009;45:747-55. [Crossref] [PubMed]
- Guo Y, Zeng H, Zheng R, et al. The burden of lung cancer mortality attributable to fine particles in China. Sci Total Environ 2017;579:1460-6. [Crossref] [PubMed]
- Turner MC, Andersen ZJ, Baccarelli A, et al. Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J Clin 2020; Epub ahead of print. [Crossref] [PubMed]
- Bade BC, Dela Cruz CS. Lung Cancer 2020: Epidemiology, Etiology, and Prevention. Clin Chest Med 2020;41:1-24. [Crossref] [PubMed]
- Xiao L, Nan Y, Di XB, et al. Study on smoking behavior and its changes among Chinese people aged 15 years and above in 2018. Zhonghua Liu Xing Bing Xue Za Zhi 2022;43:811-7. [PubMed]
- Zhan D, Zhang Q, Xu X, et al. Spatiotemporal Distribution of Continuous Air Pollution and Its Relationship with Socioeconomic and Natural Factors in China. Int J Environ Res Public Health 2022;19:6635. [Crossref] [PubMed]
- Han RQ, Wu M, Miao WG, et al. Analysis of Cancer Incidence and Mortality in Jiangsu 2015. China Cancer 2020;29:81-9.
- Ma JY, Zhou Y, Lin YT, et al. Analysis of Incidence and Mortality in Fujian Cancer Registries, 2016. China Cancer 2021;30:241-9.
- Xu KK, Wang J, Liao XZ, et al. Incidence and Mortality of Cancer in Hunan Cancer Registries, 2016. China Cancer 2021;30:250-61.
- Yang W, Qian F, Teng J, et al. Community-based lung cancer screening with low-dose CT in China: Results of the baseline screening. Lung Cancer 2018;117:20-6. [Crossref] [PubMed]
- Sun S, Wang H, Howard AG, et al. Loss of Novel Diversity in Human Gut Microbiota Associated with Ongoing Urbanization in China. mSystems 2022; Epub ahead of print. [Crossref] [PubMed]
- Wang W, Du W, Liu K, et al. The Evolution of China’s Railway Network (CRN) 1999-2019: Urbanization Impact and Regional Connectivity. Urban Rail Transit 2022;8:134-45. [Crossref] [PubMed]
- Yang F, Xu Q, Li K, et al. The inhibition effect of bank credits on PM2.5 concentrations: Spatial evidence from high-polluting firms in China. Environ Pollut 2022;308:119639. [Crossref] [PubMed]
- Han R, Zheng R, Zhang S, et al. Trend Analyses on the Differences of Lung Cancer Incidence Between Gender, Area and Average Age in China During 1989-2008. Zhongguo Fei Ai Za Zhi 2013;16:445-51. [PubMed]
- Guo LW, Chen Q, Shen YC, et al. Evaluation of a Low-Dose Computed Tomography Lung Cancer Screening Program in Henan, China. JAMA Netw Open 2020;3:e2019039. [Crossref] [PubMed]
- Wu YJ, Wu FZ, Yang SC, et al. Radiomics in Early Lung Cancer Diagnosis: From Diagnosis to Clinical Decision Support and Education. Diagnostics (Basel) 2022;12:1064. [Crossref] [PubMed]
- Lin KF, Wu HF, Huang WC, et al. Propensity score analysis of lung cancer risk in a population with high prevalence of non-smoking related lung cancer. BMC Pulm Med 2017;17:120. [Crossref] [PubMed]
- International Early Lung Cancer Action Program Investigators. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763-71. [Crossref] [PubMed]
- Zhang ML, Wu CX, Gong YM, et al. Survival analysis of patients with lung cancer in Shanghai. China Oncology. 2017;27:326-33.
- Shi JF, Wang L, Wu N, et al. Clinical characteristics and medical service utilization of lung cancer in China, 2005-2014: Overall design and results from a multicenter retrospective epidemiologic survey. Lung Cancer 2019;128:91-100. [Crossref] [PubMed]
- Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 2018;6:e555-67. [Crossref] [PubMed]
- Xing PY, Zhu YX, Wang L, et al. What are the clinical symptoms and physical signs for non-small cell lung cancer before diagnosis is made? A nation-wide multicenter 10-year retrospective study in China. Cancer Med 2019;8:4055-69. [Crossref] [PubMed]
- He J, Li N, Chen WQ, et al. China guideline for the screening and early detection of lung cancer (2021, Beijing). Chinese Journal of Oncology 2021;43:243-68. [PubMed]
(English Language Editor: L. Huleatt)