
Descending perineal syndrome cure by deep transversus perinei ligament repair: surgical options
Highlight box
Key findings
• Shortening and reinforcing the deep transversus perinei (DTP) ligaments corrects perineocele and may cure descending perineal syndrome (DPS).
What is known and what is new?
• It has been stated that “It is controversial whether surgical management is even an option for patients with DPS”.
• DPS pathogenesis is elongation of DTP ligaments and may be cured by DTP shortening and repair using either a minisling tape or No. 2 polyester sutures.
What is the implication, and what should change now?
• DPS is surgically treatable by repairing DTP ligaments.
Introduction
The key points of the article are summarized in the video abstract (Video S1).
Descending perineal syndrome (DPS) was described by Parks et al. (1) as descent of the anus on straining, typically 3–4 cm below a line drawn from the coccyx to the lower end of the symphysis (Figure 1) (1). DPS is associated with obstructed defecation, with increased bulging of the perineum with straining, although perineal descent can also be seen at rest (2). In their review, Chaudhry and Tarnay stated: “It is controversial whether surgical management is even an option for patients with DPS” (2). This has not been the experience of the many authors who have achieved successful repair of DTP in patients with obstructed defecation, large perineocele and assisted defecation using a Tissue Fixation System (TFS) minisling to shorten and reinforce the deep transversus perinei (DTP) ligaments (3-6). At 12-month follow-up for women with DPS who had minisling surgical repair of their DTP ligaments 27 (90%) reported normal defecation and the median obstructive defecation syndrome score was significantly reduced (3,5).

The TFS sling operation is no longer available in many countries where all mesh slings (other than the midurethral) have been banned by government decree. This ban has created a search for collagen creation methods, other than commercial mesh tape kits, to repair collagen deficient ligaments. We describe two methods which can repair damaged DTPs: a wide-bore No. 2 polyester suture method for repair of DPS, and an artisan tape method (7) which can perform a similar function to the TFS minisling (7). The experimental biomechanical basis of collagen creation by the wide-bore No. 2 polyester sutures for repair of damaged ligaments is described later in the discussion. The aim of this review is to discuss an anatomical pathogenesis and surgical options where sling bans remain.
Anatomy of the perineal body (PB)
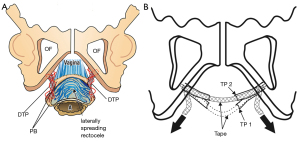
The DTP are the suspensory ligaments of the PB (3-6). Though described as DTP “muscles”, their appearance and histological analysis indicate the same structure as ligaments: collagen, elastin and smooth muscle. With reference to Figures 1-3, and Video S1, the PB is suspended from the descending rami by the DTP ligaments which are approximately 4 cm long and insert behind the upper two thirds and lower one third of the descending ischial rami.
Pathogenesis of DPS
During childbirth, the PB is stretched and displaced laterally and inferiorly. In women with DPS, the DTPs are elongated and descended to below the ischial tuberosities (Figure 2). In such patients there is virtually no separation between the vagina and rectum which are adhered together and bulge downwards on straining (Figure 1).
DPS presentation
Typically, women experiencing DPS present with a history of obstructed defecation and require manual support of the perineum during defecation. Examination reveals distinct bulging perineal defect, most noticeable on straining. Almost invariably, other prolapses (cystocoele, uterine or vault prolapse) co-exist in women with DPS as well as additional disorders including pain and symptoms related to the bladder and bowel.
Clinical history and anatomically-based vaginal and rectal examination are usually sufficient as regards the decision for surgery, although transperineal ultrasound and defecography can be useful to exclude other dysfunctions such as co-existing intussusception.
Surgical rationale for repair of DPS
Repair of the DPS using the TFS minisling has been described previously (3-6). The surgical basis of a procedure using wide-bore No. 2 polyester sutures is summarised in Video S1. An essential component of DPS repair (and indeed the most difficult) is the surgical dissection of a thin rectal mucosa from the vagina and PB. This dissection technique is the same, regardless of the method for DPS repair (3,5,6) (Video S2). The second component of the operation is the repair of elongated DTPs, either with tapes, or collagen-creating No. 2 polyester sutures. The tapes or polyester sutures shorten and reinforce the DTP (Figure 3). At times, one of the DTPs may be found ruptured. In such cases, the No. 2 polyester method cannot adequately repair the DTP. The only solution is a 10 cm × 1 cm artisan tape which needs to be inserted as a sling to suspend the PB. The artisan tape will also create a collagenous DTP neoligament in a similar manner to that of a TFS minisling (7).
Surgical technique for polyester suture of DTP
A laxative suppository inserted the night before surgery ensures the rectum is empty. It is useful to ensure that the buttocks protrude 3 cm from the edge of the operating table to ensure adequate vaginal access. An 18 G Foley catheter is inserted. Whether a tape or polyester No. 2 suture method is used, the dissection and surgical principles are identical. The PB anatomy is restored, and the supporting ligaments of the PB, the DTP, are identified, shortened and reinforced by a method creates new collagen.
A full thickness incision is made on the posterior vaginal wall. Depending on surgeon preference, this incision is either a 5 cm transverse incision immediately cephalad to the hymen or a midline incision from the introitus to mid-vagina. Contralateral stretching of vaginal tissues is critical during dissection to allow precise access to the tissue planes. DPS patients may have only a very slender layer of rectal mucosa, as thin as 1 mm, adherent to a layer of thin vaginal epithelium. The rectal mucosa has invariably spread laterally, as in Figure 3, and is densely adherent to the PB components, which are usually displaced downwards and laterally, to below the ischial tuberosity. Very careful rectal examination with one finger is most helpful in determining the spread of the adherent rectum.
Location of displaced PB
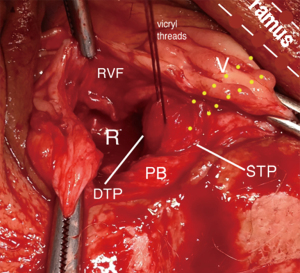
This is an essential part of the operation. The PB is firm and whitish in appearance and women with DPS is generally located below the ischial tuberosities. The PB is dissected fully from the adherent rectum and grasped with Littlewood forceps. A No. 1 polyglactin holding suture is inserted to elevate the PB to the operating field (Figure 2) allowing it to be included in the DTP suture (Figure 3) (see Video S2).
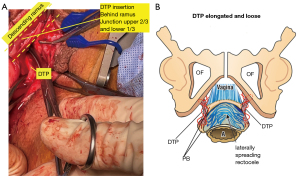
Identification of the DTP ligament requires dissection of the rectum from the vaginal epithelium and the laterally displaced PB components. The polyglactin suture identifying PB (Figure 2) is stretched toward the operator, and using a finger, the surgeon can identify the insertion of the DTP into the posterior part of the descending ischial ramus. This insertion point is at the junction of the upper two thirds and lower one third of the descending ramus.
In patients suffering with DPS, the smooth muscle layer of the rectum has usually split and retracted laterally. In such cases, the rectal mucosa is very thin (approximately 1 mm) and can be found ballooning out between the split and laterally displaced rectal walls. The rectal mucosa is invariably adherent to the posterior vaginal wall and the laterally/downwardly displaced PB. The two ends of the split rectal serosa and smooth muscle layers are located and approximated in the midline with three 00 polyglactin sutures, as in Video S2.
The identification of DTP insertion behind the descending ramus is also an important component of the operation. There is an anatomical continuum from PB to DTP and to the insertion point of the DTP which is behind the ramus (Figure 2, parallel lines of dots). Lateral retraction of the PB holding suture allows digital confirmation of its insertion point on the descending ramus. It is important to be aware of the puborectalis muscle (PRM) which lies behind the DTP insertion so it is not sutured in error during the operation. The PRM can be distinguished by its red colour, unlike the whitish colour of the PB/DTP. Retraction of the PB suture, with a finger simultaneously placed below the symphysis, indicates if one is grasping the PRM rather than the DTP.
Restoration of anatomy using tapes
The TFS tape method (Figure 3) has been described in previous publications (3-6). After the dissection, a tunnel is made to the origin of the DTP. The TFS applicator is inserted on one side, then the other, and tightened until the PB is elevated to its normal position. It is possible to use an artisan tape (7) which used techniques very similar to those of the TFS: cardinal, uterosacral and pubourethral ligaments were repaired by inserting 10 cm × 1 cm artisan tapes in the position of these ligaments to shorten and repair them (7). For DPS repair, the tape needs to penetrate the two displaced PB components and elevate them towards the descending ramus, in the position of the DTP. At 12-month follow-up, 27 patients (90%) reported normal defaecation and the median obstructive defaecation syndrome score was significantly reduced to 4 (range, 1–6; P<0.001) (1,2). The second group comprised 234 women where the technique was discussed further in the context of total pelvic ligament repair (3). The tape erosion rate was 3%, but there was no infection or abscess.
Native DTP repair using No. 2 polyester sutures
In the context of total mesh bans, the stated “non-curability” of DPS (2), and the unwillingness of the first author (R.H.) to use an artisan tape, R.H. performed a standard PB repair with one difference, identification of the DTP ligaments, and plication thereof with wide-bore native ligament sutures.
Technique for repair of DTP
A polyester suture attached to a firm 1.25 cm needle shortens and reinforces the DTP (Figure 3). The first suture is applied immediately behind the descending ramus, brought down to the PB held by the No. 1 polyglactin suture, and then brought back up to be tied, as in Figure 3. This tie should be firm but not tight. The DTP repair is repeated contralaterally. Shortening the DTP ligaments elevates the PB which then rotates somewhat inwards, causing downward displacement of the rectum. The superficial transverse muscles and the two sides of PB are gently approximated with polyglactin sutures. Figure 4 more precisely demonstrates elongation of the DTP from its normal length 4 cm to an estimated 5–6 cm. Note also its looseness and its insertion behind the lower part of the descending ramus. The right figure (Figure 4B) is added to illustrate the principles of the procedure: reconnection of the DTP to the PB and concertina plication of the DTP to cause shortening of these ligaments and eventually the creation of new collagen. The medium-term data available, 6–18 months, concerns four women who underwent the modified PB repair with DPS plication. There were no complications, with successful anatomical and clinical results.
Discussion
Regardless of the technique applied to PB repair, the first (and most difficult) steps are always the same: restoration of the anatomy by dissecting the rectum from the vagina and repairing its damaged walls. Regarding the polyester suture DTP repair, the questions arising are: “What are the prospects for longer-term success?”; “Is the collagen reaction to No. 2 polyester wide-bore sutures sufficient to reinforce elongated or weakened DTPs?” and “Will the presence of the polyester sutures lead to extrusion?”.
Collagen from a rejected polyester aortic graft was tested on an Instron tensiometer; the polyester pulled out of the grips at a force of 0.64 megapascals (92 lbs/sq inch) (8). The known breaking strain of collagen, 18,000 lbs/sq inch (124 Megapascals) (9), was confirmed by Svensson et al. (10) who tested collagen fibrils to a mean strain value corresponding to a stress of 89±15 MPa. Collagen fascicles tested by Svensson et al. had a mean diameter of 0.27±0.16 mm, comparable to the neocollagen calculated to be produced from No. 2 wide-bore polyester sutures. It was calculated that the collagen produced would sustain a force equivalent to e12 MPa, well beyond the breaking point of a ligament breaking strength of 300 mg/mm2 (0.00294 megapascals) (11). The conclusion from revisiting this experimental data is that repair of damaged ligaments using polyester sutures is likely to be sufficient for longer-term repair, consistent with long-term Tension-free Vaginal Tape (TVT) data (12).
The discussion would not be complete without commenting on reports of DPS cure as part of pelvic organ prolapse surgery using 3–4 large abdominal promontofixated meshes per DPS patient (13). Based on questionnaires and telephone contact, the authors reported significant improvement for constipation, and obstructed defecation syndrome (ODS) and the need for digital maneuvers in about 60% of patients. No observed anatomical results were offered. We see the mesh as holding the PB in place, but without repairing the displaced anatomical components of the PB (Figure 3). The other concern is the huge amount of mesh inserted between vagina, bladder and rectum, that will inevitably create scar tissue in the vagina, which transgresses a basic surgical principle of the Integral Theory Paradigm (ITP), which is to conserve vaginal elasticity which is critical for bladder function.
Conclusions
In the absence of any concepts for pathogenesis and cure for DPS (1,2), it is reasonable for interested surgeons to more precisely restore the anatomy of the PB. The surgical dissection is not so different to thorough PB repair which dissects the rectum and the vagina from the PB and approximates its displaced components. Identifying the DTPs, shortening and reinforcing them with a tape or with No. 2 polyester sutures creates neocollagen to reinforce the suspensory ligaments of the PB. If the addition of the polyester suturing of the DPS to standard PB repair is successful, it will not be so difficult for experienced vaginal surgeons to add this small step to their technique. Though promising, only long-term results can determine the effectiveness of this innovation.
Acknowledgments
We wish to express our gratitude to Editors Professor Peter Petros and Vani Bardetta for their exceptional support in the design and refinement of the article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1803/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1803/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article, accompanying images and videos. Human participation in the videos was by patient permission on the basis it was deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parks AG, Porter NH, Hardcastle J. The syndrome of the descending perineum. Proc R Soc Med 1966;59:477-82.
- Chaudhry Z, Tarnay C. Descending perineum syndrome: a review of the presentation, diagnosis, and management. Int Urogynecol J 2016;27:1149-56. [Crossref] [PubMed]
- Petros P, Inoue H. Transvaginal perineal body repair for low rectocele. Tech Coloproctol 2013;17:449-54. [Crossref] [PubMed]
- Wagenlehner FM, Del Amo E, Santoro GA, et al. Live anatomy of the perineal body in patients with third-degree rectocele. Colorectal Dis 2013;15:1416-22. [Crossref] [PubMed]
- Wagenlehner FM, Del Amo E, Santoro GA, et al. Perineal body repair in patients with third degree rectocele: a critical analysis of the tissue fixation system. Colorectal Dis 2013;15:e760-e765. [Crossref] [PubMed]
- Petros PE. Tissue Fixation System Perineal Body Repair: A Minimally Invasive Method for Repair of Descending Perineal Syndrome. Dis Colon Rectum 2016;59:e455. [Crossref] [PubMed]
- Piñango-Luna S, Level-Córdova L, Petros PE, et al. A low cost artisan tension-free tape technique cures pelvic organ prolapse and stress urinary incontinence - proof of concept. Cent European J Urol 2020;73:490-7. [Crossref] [PubMed]
- Petros PE. Development of the Intravaginal Slingplasty and other ambulatory vaginal operations. Doctor of Surgery Thesis. Perth (WA): University of Western Australia; 1999.
- Florey H. General Pathology. 4th ed. London: Lloyd Luke; 1971:457.
- Svensson RB, Hassenkam T, Grant CA, et al. Tensile properties of human collagen fibrils and fascicles are insensitive to environmental salts. Biophys J 2010;99:4020-7. [Crossref] [PubMed]
- Yamada H. Aging rate for the strength of human organs and tissues. In: Evans FG, editor. Strength of biological materials. Baltimore: Williams & Wilkins Co; 1970:272‐80.
- Nilsson CG, Palva K, Aarnio R, et al. Seventeen years' follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J 2013;24:1265-9. [Crossref] [PubMed]
- Nessi A, Kane A, Vincens E, et al. Descending Perineum Associated With Pelvic Organ Prolapse Treated by Sacral Colpoperineopexy and Retrorectal Mesh Fixation: Preliminary Results. Front Surg 2018;5:50. [Crossref] [PubMed]


