A patient with situs inversus totalis and lung cancer—a rare combination
Introduction
Situs inversus totalis (SIT) is a rare clinical entity which is characterized by a complete reverse anatomy of the thoracic and abdominal organs. It is a congenital autosomal recessive disease, which has also been connected with X-chromosome defect, and occurs in between 1/8,000 and 1/20,000 newborns. Twenty percent to twenty five percent of the cases are associated with Kartagener syndrome. Cardiac and vascular anomalies are more frequent in patients with SIT compared to the general population (1). In this article we aim to present a case of an 80 years old male patient with SIT and lung cancer. Staging was defined by biopsies using uniportal video-assisted thoracoscopic surgery (VATS) and mediastinoscopy; afterwards a left lower lobectomy was performed.
Case presentation
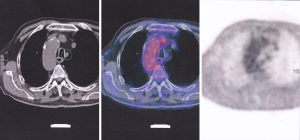
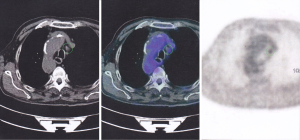
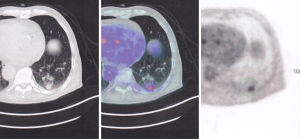
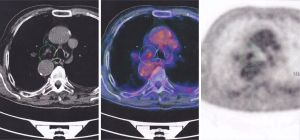
An 80 years old male patient presented to our department with a tumor of the left lower lobe diagnosed using computed tomography (CT) and positron emission tomography–computed tomography (PET/CT). The CT scan revealed an anatomically inverted situs that was already known to the patient since childhood. The arrangement of the pulmonary vessels and the bronchi were a mirror image of those normally found on the other side. The CT scan also revealed a left lower lobe nodule of 1.8 cm in diameter, 6–7 distinct lymph nodes (LN) No. 4L of 1–1.2 cm in size and 2–3 LN No. 5R with diameter up to 2 cm. A PET/CT was also performed, which revealed PET(+) No. 5R and No. 4L LN. A biopsy of No. 5 PET(+) and preaortic PET(−) lymph note was performed with a uniportal VATS procedure. Mediastinoscopy was used for access and sampling of No. 4L PET(+) LN. In both cases PET(+) 5R and 4L LN were found reactive, anthracotic and negative for metastatic carcinoma (Figures 1-4, Table 1).

Full table
The stage of the tumor was categorized as cT1aN0M0 and thus we proceeded with a left lower lobectomy. The mirror image of the normal anatomy that was revealed in CT was verified intraoperatively. During the operation properly sided double-lumen intubation tube was used. The patient’s postoperative course was largely uneventful. He was discharged on the 10th postoperative day. Histopathology confirmed an invasive papillary predominant adenocarcinoma (pT1aN0) according to IASLC/ATS/ERS 2011.
Discussion
This patient was the first case with coexistence of lung cancer and SIT surgically treated by our department and also the first patient in Greece to be reported in PubMed. There are 21 cases of SIT and lung cancer reported in Literature. Eleven of those were treated surgically with either a pneumonectomy or lobectomy. Left sided cancer was predominant over right sided and left sided operations were performed more frequently (1,2). Our case was the second in the literature to be treated with a left lower lobectomy. The first case of left lower lobectomy performed on a patient with SIT was described by Shimizu et al. in 2011 (3).
Preoperative diagnosis of SIT is very important in order for the clinician to plan further treatment (3,5). Diagnosis of the syndrome can be confirmed using chest X-ray, CT, bronchoscopy, ultrasonography (u/s), echocardiography and/or angiography (1,3). In particular the proper use of the X-ray and its correct initial interpretation by the clinician can raise the suspicion of SIT (1). As in most of the patients, our patient was diagnosed with SIT since his childhood (1). A high suspicion of lung cancer was set using PET/CT, which also confirmed the patient’s inverted but proper anatomy. Bronchoscopy was not performed. Because the findings of the PET/CT scanning possibly suggested N2 or N3 stage, further examinations followed. We preceded with uniportal VATS to sample LN because of the existence of SIT (7). Subsequently a mediastinoscopy and PET(+) No. 4L lymph node biopsy was performed. According to Mahmoud et al., a mediastinoscopy in those patients was deemed to be safe with a thorough knowledge of the anatomy of the region and the application of proper surgical techniques (8).
Endoscopic ultrasound (EUS) and endobronchial ultrasound (EBUS) can provide us with vital information for the staging and surgical anatomy (1,7). In our case based on the CT findings the LN were regarded as not feasible for EBUS or EUS. Subotich et al. suggested that in all patients with SIT, a preoperative angiography should be performed to investigate the vascular anatomy of the region, because of the increased possibility of vascular anomalies (5). A CT 3D reconstruction and magnetic resonance imaging (MRI) may be helpful (1). In our preoperative CT scan, when employing 3D reconstruction, the branches of the pulmonary vessels and bronchial tree of the left lower lobe were a mirror image of the right lower lobe. The anatomy of the region was considered well identified and angiography was not performed.
A left lower lobectomy was performed through an anterolateral thoracotomy (1). Yoshida et al. has described a right lower lobectomy using VATS, after carefully examining the anatomical relations of the vascular and bronchial tree (4).
Conclusions
SIT is a very rare entity that the clinician should have in mind. The syndrome diagnosis should be made early. Pre- and perioperative attention should be paid for vascular and bronchial anomalies in order to avoid intra-operative injuries and complications. If necessary, various imaging techniques should be employed before proceeding with surgery so that anatomy is as accurately as possible identified.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Wójcik J, Grodzki T, Bielewicz M, et al. Lung cancer in situs inversus totalis (SIT)--literature review. Adv Med Sci 2013;58:1-8. [Crossref] [PubMed]
- Masuda Y, Marutsuka T, Saishoji T. Lung resection for lung cancer in patient with situs inversus totalis. Kyobu Geka 2013;66:481-4. [PubMed]
- Shimizu J, Arano Y, Adachi I, et al. Adenosquamous carcinoma of the lung in a patient with complete situs inversus. Ann Thorac Cardiovasc Surg 2011;17:178-81. [Crossref] [PubMed]
- Yoshida M, Hino H, Machida H, et al. Video-assisted thoracic surgery lobectomy for lung cancer in a patient with complete situs inversus. Gen Thorac Cardiovasc Surg 2013;61:155-9. [Crossref] [PubMed]
- Subotich D, Mandarich D, Katchar V, et al. Lung resection for primary bronchial carcinoma in a patient with complete situs inversus. Clin Anat 2006;19:358-62. [Crossref] [PubMed]
- Murakawa T, Nakajima J, Fukami T, et al. Lung cancer operation in situs inversus totalis patient. Kyobu Geka 2009;62:1010-3. [PubMed]
- Cerfolio RJ, Bryant AS, Eloubeidi MA. Accessing the aortopulmonary window (#5) and the paraaortic (#6) lymph nodes in patients with non-small cell lung cancer. Ann Thorac Surg 2007;84:940-5. [Crossref] [PubMed]
- Mahmoud A, Pham H, Matolo N, et al. Safety of mediastinoscopy in anatomical variations of the mediastinum: the situs inversus syndrome. Am Surg 2006;72:64-7. [PubMed]


