
A nationwide comparative analysis of medical complications in fibromyalgia patients following total knee arthroplasty
Introduction
The diagnostic label of fibromyalgia is often debated because its etiology and pathogenesis remain unclear (1,2). Although typically classified as a musculoskeletal disorder, the condition is now considered to be a central sensitivity disorder which results in augmentation of pain (3). Thus, these patients experience pain differently to those without the condition. Fibromyalgia is associated with several conditions with and without structural pathology. The disease is commonly seen with comorbid conditions such as rheumatoid arthritis, systemic lupus, ankylosing spondylitis, and osteoarthritis (4). The relationship between fibromyalgia and rheumatic diseases is well-established (5-7) and this comorbidity is estimated to be between 11% and 30% (6). For example, a study in the United Kingdom reported that 12% to 17% of rheumatoid arthritis patients attending an outpatient clinic were found to have a diagnosis of fibromyalgia based the American College of Rheumatology criteria (5). Furthermore, a longitudinal study of hip and knee osteoarthritis patients (n=613) in Canada found that 11% of the sample met the diagnostic criteria for fibromyalgia.
As musculoskeletal pain is the primary manifestation of fibromyalgia, orthopaedic physicians commonly find themselves treating these patients. Given the altered pain processing mechanisms underlying the condition and its increased comorbidity, it is important to examine the clinical outcomes of these patients to enable and promote optimal orthopaedic care. There is evidence to suggest that fibromyalgia patients are less satisfied (8), have poorer functional outcomes (8), show less improvement in pain (9) and have increased opioid consumption (10,11) post-operatively. Fibromyalgia patients have also been found to have a higher likelihood of experiencing 30- and 90-day postoperative complications following posterior lumbar spine fusion (12). Although few studies have reported on total knee arthroplasties (TKAs) outcomes in fibromyalgia patients, there is a lack of extensive studies focusing specifically on the postoperative surgical outcomes of these patients.
Thus, the purpose of this study was to evaluate whether fibromyalgia patients, compared to a matched cohort of non-fibromyalgia patients, were more likely to experience medical complications following TKA. Specifically, we assessed the risk of developing any medical complication as well as specific medical complications of these patients after TKA.
Methods
Data source
A retrospective review was performed from January 1, 2004 to December 31, 2015 using the Standard Analytical Files of the Medicare database from the PearlDiver (PearlDiver Technologies, Fort Wayne, Indiana) supercomputer. PearlDiver is compliant with the Health Information Portability and Affordability Act (HIPAA) and is exempt from International Review Board (IRB) as the information is de-identified. The database includes information on diagnoses, complications, procedures, lengths-of-stay, costs, reimbursements, discharge dispositions, as well as other information related to a patient’s episode of care. Patients were queried using the International Classification of Disease, ninth revision (ICD-9) codes, as described below.
Study population
All patients who underwent primary a TKA were queried using the ICD-9 procedural code 81.54. A total of 3,974,092 patients were initially identified. From this cohort, patients with a diagnosis of fibromyalgia were identified using ICD-9 diagnosis code 729.1. Patients undergoing TKA without fibromyalgia served as the control group. In order to control for potential confounding variables, fibromyalgia patients and non-fibromyalgia TKA patients were matched in a 1:1 ratio with the use of propensity score matching based on age, sex, and the Charlson Comorbidity Index (CCI). Each cohort was longitudinally followed for 90-days following the index procedure.
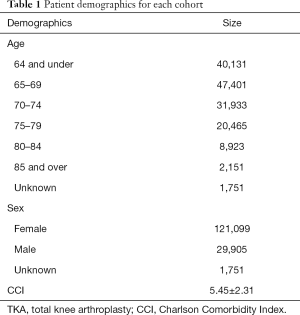
Propensity score matching yielded a total study population cohort of 305,510 patients (female =242,198; male =59,810; and unknown =3,502) with (n=152,755) and without fibromyalgia (n=152,755) (Table 1). Average CCI between the study group and control group was 5.45±2.31, with a P value =1.00, indicating the study and control group were properly matched.
Full table
Outcomes assessed
Patients were first assessed for any medical complication before being further examined for specific medical complications. The medical complications examined were urinary tract infections, acute post-hemorrhagic anemia, thoracic or lumbosacral neuritis or radiculitis, respiratory abnormalities, transfusions, acute kidney failure, postoperative infection, ankylosis of joint lower leg, acute venous embolism or thrombosis, and contracture of joint lower leg.
Data analysis
The fibromyalgia and non-fibromyalgia cohorts were evaluated for any medical complication as well as specific medical complications, as listed above. Statistical analyses were performed using MedCalc for Windows, version 18.2.1 (MedCalc Software, Ostend, Belgium). Odds ratios, 95% confidence intervals (95% CI), and P values (<0.05) were calculated and compared for the fibromyalgia and non-fibromyalgia patients with respect to any and specific medical outcomes.
Results
Any medical complication
In the 90-days following TKA, 5,537 medical complications were reported among fibromyalgia patients compared to 2,889 among non-fibromyalgia patients, indicating that fibromyalgia patients had significantly greater odds of developing any medical complication [odds ratio (OR): 1.95, 95% CI: 1.86–2.04, P<0.001] compared to a matched cohort.
Specific medical complications
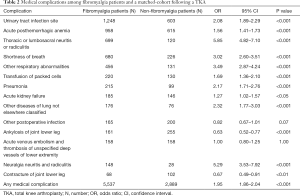
In the 90-days following primary TKA, patients with fibromyalgia had significantly greater odds of developing urinary tract infections (OR: 2.08, 95% CI: 1.89–2.29, P<0.001), acute posthemorrhagic anemia (OR: 1.56, 95% CI: 1.41–1.73, P<0.001), and thoracic or lumbosacral neuritis or radiculitis (OR: 5.85, 95% CI: 4.82–7.10, P<0.001). Fibromyalgia patients also had substantially greater respiratory complications such as shortness of breath (OR: 3.02, 95% CI: 2.60–3.51, P<0.001), pneumonia (OR: 2.17, 95% CI: 1.71–2.76, P<0.001), lung disease (OR: 2.32, 95% CI: 1.77–3.03, P<0.001), and other respiratory abnormalities (OR: 3.49, 95% CI: 2.87–4.24, P<0.001). Furthermore, fibromyalgia patients had greater rates of transfusion (OR: 1.69, 95% CI: 1.36–2.10, P<0.001), acute kidney failure (OR: 1.27, 95% CI: 1.02–1.57, P<0.05), and neuralgia neuritis and radiculitis (OR: 5.29, 95% CI: 3.53–7.92, P<0.001) compared to the matched cohort of non-fibromyalgia cohort (Table 2).
Full table
Fibromyalgia patients were significantly less likely than non-fibromyalgia patients to develop ankylosis of joint lower leg (OR: 0.63, 95% CI: 0.52–0.77, P<0.001) and contracture of joint lower leg (OR: 0.67, 95% CI: 0.49–0.91, P<0.01). These patients were no more likely than a matched cohort to develop other postoperative infections (OR: 0.82, 95% CI: 0.67–1.01, P=0.07) and acute venous embolism and thrombosis of unspecified deep vessels of lower extremity (OR: 1.00, 95% CI: 0.80–1.25, P=1.00).
Discussion
Fibromyalgia is characterized by widespread pain and a range of associated symptoms including fatigue, depression and cognitive impairment (13). The orthopaedic management of these patients may be challenging given their abnormal experience of pain (14) and increased comorbidities (4). With the escalating rate of TKAs (15), it is important that orthopaedic specialists caring for these patients are aware of the potential risks and complications following TKA. There is a paucity of literature on fibromyalgia and TKAs, possibly due to the previous lack of widespread consensus of the condition (16), therefore the findings of this study provide valuable information for physicians and their patients.
This is the first study to assess and find out that fibromyalgia patients were more likely than a matched-cohort of non-fibromyalgia patients to develop medical complications following TKA. Specifically, they were more likely to develop urinary tract infections, acute posthemorrhagic anemia, thoracic or lumbosacral neuritis or radiculitis, shortness of breath, other diseases of lung not elsewhere classified, other respiratory abnormalities, transfusion of packed cells, pneumonia, acute kidney failure, neuralgia neuritis, and radiculitis.
The present study has some limitations. The studied cohort had a post-operative follow up of 90 days which does not account for medical complications that could arise outside of the 90-day window. However, the 90-day window is of most importance in the setting of bundled payments. Also, fibromyalgia patients were selectively chosen for analysis, while non-fibromyalgia patients were not selectively chosen. In order to reduce the impact of a number of potential confounders, propensity score matching was carried out. Furthermore, this study examined aggregated data as opposed to raw data. This indicates a potential loss of information and eliminates the option of analyzing individual-level data. Nevertheless, this study is the first of its kind and will direct the path of future studies.
Other related studies have found similar results. D’Apuzzo et al. examined 110 fibromyalgia patients who underwent primary TKA between 1990 and 2001. The most common postoperative complication was arthrofibrosis (9%) followed by instability (12%), wound problems (4%), periprosthetic fracture (<1%), and quadriceps tendon rupture (<1%). Furthermore, 82% of patients were satisfied with the results of surgery however 44% continued with some degree of pain (17). More recently, a study by Donnally et al. assessed postoperative medical complications of fibromyalgia patients following primary 1 to 2 level lumbar fusions (12). The group found that fibromyalgia patients were more likely to develop acute post hemorrhagic anemia within the first 30 days post-operative, and were more likely to contract pneumonia within 90-days post-operative.
The literature on fibromyalgia and TKA, however, focuses primarily on patient satisfaction, opioid consumption, and analgesic outcomes. In 2011, a matched cohort study by Bican et al. examining fibromyalgia patients compared to non-fibromyalgia patients who underwent a TKA reported that at mean of 3 years follow-up, fibromyalgia patients were less satisfied with the outcome of the surgery despite demonstrating improvement that was comparable to the controls (8). Regarding opioid consumption, there is evidence to suggest that a higher fibromyalgia survey score is independently associated with increased opioid consumption following TKA and total hip arthroplasty (THA) (10,11). Also, Brummett et al., in a prospective observational study, showed that a higher fibromyalgia survey score was independently associated with less improvement in the pain in the affected knee or hip, in overall bodily pain, and in global impression of global following TKA or THA (10).
Conclusions
This is the first study to examine whether fibromyalgia patients are more likely than non-fibromyalgia patients to develop medical complications following TKA. The results demonstrate that patients diagnosed with fibromyalgia are more likely to develop a number of medical complication than non-fibromyalgia patients. In light of these, fibromyalgia patients and orthopaedic surgeons can more optimally plan for a TKA in a way that minimizes, or potentially avoids, post-operative complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. G Scuderi: Acelity; Biomet; Convatec; Force Therapeutics; Medtronic; Operation Walk USA; Pacira; SpringerElsevierThiemeWorld Scientific; Zimmer. MW Roche: Stryker, Orthosensor, Cayenne. The other authors have no conflicts of interest to declare.
Ethical Statement: IRB determined this study exempt as it utilized de-identified, publicly available data.
References
- Bidari A, Ghavidel Parsa B, Ghalehbaghi B. Challenges in fibromyalgia diagnosis: from meaning of symptoms to fibromyalgia labeling. Korean J Pain 2018;31:147-54. [Crossref] [PubMed]
- Cohen H. Controversies and challenges in fibromyalgia: a review and a proposal. Ther Adv Musculoskelet Dis 2017;9:115-27. [Crossref] [PubMed]
- Burgmer M, Pogatzki-Zahn E, Gaubitz M, et al. Altered brain activity during pain processing in fibromyalgia. Neuroimage 2009;44:502-8. [Crossref] [PubMed]
- Yunus MB. The prevalence of fibromyalgia in other chronic pain conditions. Pain Res Treat 2012;2012:584573. [Crossref] [PubMed]
- Pollard LC, Kingsley GH, Choy EH, et al. Fibromyalgic rheumatoid arthritis and disease assessment. Rheumatology (Oxford) 2010;49:924-8. [Crossref] [PubMed]
- Haliloglu S, Carlioglu A, Akdeniz D, et al. Fibromyalgia in patients with other rheumatic diseases: prevalence and relationship with disease activity. Rheumatol Int 2014;34:1275-80. [Crossref] [PubMed]
- Ranzolin A, Brenol JC, Bredemeier M, et al. Association of concomitant fibromyalgia with worse disease activity score in 28 joints, health assessment questionnaire, and short form 36 scores in patients with rheumatoid arthritis. Arthritis Rheum 2009;61:794-800. [Crossref] [PubMed]
- Bican O, Jacovides C, Pulido L, et al. Total knee arthroplasty in patients with fibromyalgia. J Knee Surg 2011;24:265-71. [Crossref] [PubMed]
- Brummett CM, Urquhart AG, Hassett AL, et al. Characteristics of fibromyalgia independently predict poorer long-term analgesic outcomes following total knee and hip arthroplasty. Arthritis Rheumatol 2015;67:1386-94. [Crossref] [PubMed]
- Brummett CM, Janda AM, Schueller CM, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology 2013;119:1434-43. [Crossref] [PubMed]
- Namba RS, Singh A, Paxton EW, et al. Patient Factors Associated With Prolonged Postoperative Opioid Use After Total Knee Arthroplasty. J Arthroplasty 2018;33:2449-54. [Crossref] [PubMed]
- Donnally CJ 3rd, Vakharia RM, Rush AJ 3rd, et al. Fibromyalgia as a Predictor of Increased Post-Operative Complications, Readmission Rates and Hospital Costs in Patients Undergoing Posterior Lumbar Spine Fusion. Spine (Phila Pa 1976) 2019;44:E233-8. [Crossref] [PubMed]
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 2010;62:600-10. [Crossref] [PubMed]
- Jay GW, Barkin RL. Fibromyalgia. Dis Mon 2015;61:66-111. [Crossref] [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Fitzcharles MA, Yunus MB. The clinical concept of fibromyalgia as a changing paradigm in the past 20 years. Pain Res Treat 2012;2012:184835. [Crossref] [PubMed]
- D’Apuzzo MR, Cabanela ME, Trousdale RT, et al. Primary total knee arthroplasty in patients with fibromyalgia. Orthopedics 2012;35:e175-8. [PubMed]


