
Long-acting glucagon-like peptide-1 receptor agonist—status December 2018
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are now included in most guidelines for treatment of type 2 diabetes, most recently in the Consensus Report by the European Society for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) (1). However, it is still just a few percent of the diabetes patients that actually receive GLP-1 RA therapy. This is an interesting paradox which needs serious contemplation. It may of course be related to trivial matters such as pricing and the need for injections, but perhaps also bad reputation due to the side effects (nausea etc.) and the previous accusations of associations with cancers and pancreatitis, concerns that no longer receive much attention. In view of the documented beneficial effects of these drugs, this is something the health care providers should consider more carefully.
GLP-1 RAs are available in several forms with remarkably different characteristics. The short-acting agonists comprise exenatide and lixisenatide with a duration of action of only few hours after subcutaneous (s.c.) injections. Long acting agonists include liraglutide (once daily), and exenatide once weekly (ow), albiglutide, dulaglutide and semaglutide which, except for liraglutide, are intended for weekly s.c. administration. The long acting agonists are all capable of maintaining a relevant agonist level in plasma throughout the 24 hours of the day, although the actual profiles may show some variation (perhaps most with liraglutide and least with semaglutide). Today, there is little doubt that the long acting GLP-1 RAs have better overall effects than the short acting RAs.
The GLP-1 RAs all build on the actions of the intestinal hormone, GLP-1, as mediated by its interaction with the G-protein coupled GLP-1 receptor. GLP-1 was isolated as an insulin-stimulating hormone (2), and the beta cells also show a particularly dense expression of the GLP-1 receptor. The receptor couples to the Gs protein (3) which activates adenylate cyclase and via cAMP formation activates protein kinase A. Many of the subsequent actions can be ascribed to the protein kinase A activation, but activation of guanine nucleotide exchange factor II (epac 2) also plays an important role. Growth effects on beta cells are probably mediated via the PI-3 kinase pathway (4). In terms of insulin secretion, the effect of the GLP-1 RAs is usually described as a potentiation of glucose-induced insulin secretion. More precisely, the GLP-1 RAs improve the sensitivity of the beta cell to glucose. This parameter may in humans be estimated from the slope of insulin secretory rates (as determined from C-peptide pharmacokinetics and deconvolution) versus a range of plasma glucose concentrations obtained by glucose infusions at increasing rates; it has the dimension: nmoles of insulin secreted per min, per kg, per increase in glucose concentration (mM) (5). This slope is severely reduced in type 2 diabetes mellitus (T2DM), but may be virtually normalized by the normal therapeutic doses of GLP-1 (5). This explains that insulin concentrations usually are not changed during chronic therapy with a GLP-1 RA (6). What is observed is a maintained insulin secretion occurring in spite of lower glucose levels. In other words, the beta cells have been sensitized to glucose, enabling them to produce the same amount of insulin in spite of lower glucose levels.
However, GLP-1 and the GLP-1 RAs have numerous other actions that are extremely important for their clinical actions. A list of these actions is provided as Table 1.
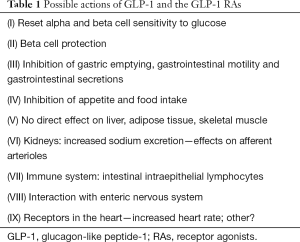
Full table
Numerous GLP-1 actions are mentioned in various reviews and publications, but common to most of the alleged actions, they have not been rigorously confirmed and/or their human relevance has not been ascertained.
Point no. (I) on the list deals with the glucose sensitivity of the beta cells as already discussed, but also the alpha cells are affected. It is usually described that GLP-1 inhibits alpha cell secretion, and this is easily observed also in patients with T2DM upon GLP-1 infusion (2). In one study, glucagon secretion was studied in T2DM during a glucose clamp, and whereas glucagon secretion was rapidly and profoundly suppressed in glucose tolerant matched control subjects, the patients showed a delayed and reduced suppression (7). A superimposed GLP-1 infusion, however, completely restored the glucose-induced suppression, suggesting that also the alpha cell sensitivity to glucose may be restored by GLP-1. It has been demonstrated that the inhibition of glucagon secretion may be responsible for at least 50% of the glucose lowering effects of GLP-1 in T2DM patients (8). Given that the effects of GLP-1 on alpha cell secretion mainly consist of facilitating suppression by glucose, then this may also explain that GLP-1 and the GLP-1RAs do not at all suppress glucagon responses to hypoglycemia (i.e., no glucose) (6).
Bullet (II), beta cell protection is clearly observed in numerous animal experiments, but human beta cells do not seem to respond to GLP-1 with proliferation, perhaps because this effect may only be observed in very young beta cells. Inhibition of apoptosis might also lead to beta cell protection but is it observed in humans? Two clinical studies suggest that there may be a protective effect: one is the 3 years study where intensive therapies with either exendin 4 or insulin were compared. In both groups beta cell function was preserved over a period of 3 years (9). In the course of 3 years, one would have expected some impairment of beta cell function to occur in patients with T2DM, so it may be concluded that GLP-1 therapy was indeed protective, but that intensive insulin therapy was similarly protective (which may be true). In the LEADER cardiovascular outcome trial of liraglutide (10), therapy was continued for up to 5 years in >9,000 T2DM patients, and it turned out that HbA1c levels were fairly well maintained throughout this period. Again, a deterioration of beta cell function would have been expected in this large group of patients with longstanding diabetes, so perhaps there is some beta cell protection after all.
Bullet (III), inhibition of gastric emptying is one of the most conspicuous actions of native GLP-1, and also the long acting GLP-1 RAs inhibit gastric emptying to some extent (11), in spite of the pronounced tachyphylaxis elicited during chronic therapy. This mechanism, therefore, does to some extent contribute to the effects of chronic GLP-1 RA treatment.
(IV) The weight loss effects of the GLP-1 RAs are of paramount importance, but here we find some important differences between the GLP-1RAs, with very weak effects exerted by albiglutide (12) and very strong effects exerted by semaglutide (13) although they have not yet all been compared in head-to-head studies (which are indispensable for such comparisons). The mechanism of action is still somewhat unclear—there is no increase in energy expenditure to explain weight loss, but the evidence points to inhibition of appetite as the driver of the decrease in food intake. There is evidence that the inhibition of appetite is exerted via centers in the brain, including hypothalamic centers as well as centers related to the reward system. Regulation of both the AGRP/NPY neurons and the POMC/CART neurons in the arcuate nucleus may play an important role (14). Endogenous GLP-1 is thought to signal to the brain via sensory afferents of the vagus nerve (15), terminating in the nucleus of the solitary tract in the brain stem, whereas exogenous GLP-1 and the GLP-1RAs probably mainly reach the brain via the leaks of the blood brain barrier in the circumventricular organs, notably the area postrema, the median eminence and the subfornical organ (14). This may also explain some of the differences between the GLP-1 RAs regarding inhibition of food intake. Liraglutide and semaglutide are noncovalently bound to albumin and therefore act as protein-bound hormones, where the free fraction is responsible for the biological activity. Free sema- or lira-glutide may reach regions in the brain that the macro-molecules, dulaglutide and albiglutide (in which the GLP-1 moiety is covalently bound to a large molecule), can access only with difficulty. For exenatide ow, the two mg dose developed may simply be too low to compete with the relatively higher doses of lira and sema-glutide.
The effects on lipid metabolism of the GLP-1 RAs are unclear; lowering of postprandial triglyceride levels has been reported (11), but is difficult to separate from the effects on gastric emptying. Long term studies with lira- and sema-glutide [LEADER and SUSTAIN 6 (10,16)] did not reveal major changes in plasma lipid concentrations, and the small changes actually observed could also be associated with the weight loss in these studies.
(V) Importantly, there are no convincing studies to suggest that there are direct actions of the GLP-1 RAs on the liver (hepatocytes), the adipose tissue (white adipocytes) or the skeletal muscles (myocytes). However, this does not exclude possible actions on other cell types in these tissues (blood vessels, immune cells).
(VI) In some of the long cardiovascular endpoint trials there were markedly beneficial effects (40% reductions) on renal endpoints (time to macroalbuminuria, doubling of serum creatinine, end stage renal disease or renal death) (10,16). So, was this an effect of improved metabolic control or direct effects on the kidneys? It is generally thought that there may be several effects of GLP-1 and the GLP-1RAs on the kidneys, but receptor expression has only been convincingly documented in the afferent arterioles (17). In experimental animals, GLP-1 has hemodynamic effects consistent with this receptor localization, but in humans this has been difficult to demonstrate, both acutely and during chronic GLP-1RA therapy. The only action that has been well documented in humans is an effect on lithium fractional excretion (consistent with inhibited proximal sodium reabsorption), although a significantly increased sodium excretion has been difficult to demonstrate except after fluid and salt challenge (18,19). In a couple of studies, there has been a clear inhibitory effect on angiotensin II levels, which may play a role (19), and could be consistent with the co-expression of renin and GLP-1 R in some cells of the juxtaglomerular afferent arterioles. At any rate, the renoprotective effects are quite marked, and clearly deserve further attendance.
(VII) GLP-1 and the immune system was the subject of a recent review in which it was concluded that GLP-1 may play an important role in inflammation (20). However, the field has been confused by reports that IL-6 might be essential for mediating GLP-1 secretion and responses under inflammatory conditions, but this is not seen in humans (21). There are also several reports that GLP-1 is secreted in response to inflammation, e.g., induced by LPS, but this is also controversial (22). However, there is agreement that there is a dense expression of the GLP-1 receptor on intestinal intraepithelial lymphocytes, and it is likely that GLP-1 and perhaps also the GLP-1 RAs may modulate enteric immune responses via this route and link mucosal integrity to innate immunity (23). However, if it turns out that the GLP-1 RAs have anti-inflammatory actions also in humans, these are likely to contribute to the beneficial cardiovascular actions of the agonists (20).
(VIII) The GLP-1R is also heavily expressed on neurons of the enteric nervous system, and this may provide the structural substrate for several both motor and vascular actions locally in the gut, as well as for ascending sensory impulses transmitted to the brain and involved in appetite and glucose control (24). Indeed, vagotomy in humans has been shown to eliminate the appetite suppressant effects of GLP-1 (25), but it must be recognized that the overall importance of this pathway, particularly when it comes to exogenous GLP-1RAs is uncertain. Indeed, deletion of sensory vagal afferents in mice had no influence on the food intake inhibiting effects of liraglutide whereas deletion of GLP-1 receptor in the brain lead to loss of effects (26).
(IX) The results of cardiovascular outcome trials regarding the GLP-1RAs are rolling in. The ELIXA trial (27) with lixisenatide was the first, soon to be followed by LEADER (10) (liraglutide 1.8 mg), SUSTAIN 6 (16) (semaglutide 1.0 mg), EXSCEL (28) (exenatide ow), HARMONY (12) (albiglutide) and REWIND (dulaglutide) (for REWIND there is so far only a company press release). What can we learn regarding the cardiovascular effects of the GLP-1 RAs from these trials? First of all, it is important to note that these are safety trials design to investigate cardiovascular safety of these compounds. The first conclusion, therefore, is that they are all safe, i.e., they do not increase the risk of a CV event during prolonged therapy. All studies had time to MACE, i.e., major adverse cardiovascular events (defined as non-fatal myocardial infarction, non-fatal stroke or cardiovascular death) as the primary end point. The pleasant surprise is that some of the studies actually showed a reduced risk of MACE. In the ELIXA trial there was no risk reduction, but this trial was of relative short duration, involved a short-acting GLP-1RA (lixisenatide with few hours’ daily exposure) and the patients had extremely high risk of an event (most had acute coronary syndrome within the last 90 days of inclusion) (27). In the LEADER study (>9,000 patients mostly with established CVD treated for at least 3.5 years) there was a 13% significant reduction in the risk of MACE, and with semaglutide in similar population (>3,000), but for 2 years only, in SUSTAIN 6, there was a highly significant 26% reduction. In EXSCEL, there was an 11% reduction (P=0.061 in almost 15,000 patients), but a significant 14% reduction in all-cause mortality. HARMONY (albiglutide) resulted in a highly significant 22% reduction in MACE. For REEWIND (dulaglutide), carried out in a population with mainly increased CVD risk but without established disease, we only have a press release (from Eli Lilly as of November 11, 2018) stating significant reduction of MACE.
The studies also have looked at the individual components of the MACE, and in the study with the strongest risk reduction (SUSTAIN 6) (16), the result was driven by significant reductions in stroke and near significant reductions in myocardial infarction, and similar changes were seen in LEADER (although insignificant). Confusing results were observed regarding cardiovascular death, where LEADER showed a 22% highly significant reduction, while there was absolutely no reduction in SUSTAIN 6. One interesting finding in SUSTAIN 6 was a very significant 35% reduction in revascularization procedures. It should also be mentioned that the therapies appeared renoprotective with very significant reductions in nephropathy risk, e.g., by 36% in SUSTAIN 6, where improvements were mainly due to reduced risk of albuminuria. In stark contrast to the results obtained with the SGLT-2 inhibitors, with empagliflozin being an outstanding example (29), there is no effect on heart failure by the GLP-1 agonists, whether as a reduced risk of MACE among those with heart failure at base line, or as a diminished risk of developing heart failure during the course of therapy. Indeed, in studies dedicated to study the effects of liraglutide in patients with heart failure (whether or not in combination with diabetes), there was no benefit, rather a tendency to increased risk (30,31). Thus, the mechanisms behind the beneficial effects of the SGLT-2 inhibitors versus the GLP-1RAs are clearly distinct. Since the RA with the strongest CV effect is also the one with strongest effects on metabolic parameters (body weight and HbA1c), one could suspect that metabolic improvement by the GLP-1 RAs play an important role. Like in SUSTAIN 6, there was also no effect on cardiovascular death in the HARMONY trial, whereas the highly significant improvement in MACE was driven almost exclusively by reduced risk of AMI. Remarkably, in that study (12) there was no effect at all on body weight or blood pressure, seemingly ruling out these parameters from being responsible for the effects. There was however a good effect on A1c. The positive results of the REWIND study (and supported by the EXSCEL results) suggest that the beneficial effects are not only reserved for those with established cardiovascular disease, but that reductions in event rates can also expected in patients with type 2 diabetes and increased risk, but without established disease. Unfortunately, there isn’t much help to gain from preclinical studies regarding the mechanisms involved. It is almost certain that there will be important differences between species, and there isn’t a lot of good evidence regarding the exact location of the GLP-1 receptor in the human heart, although robust expression of the receptor in all 4 chambers of the human heart was recently reported (32). Importantly, there was no receptor expression in cardiac fibroblasts or in coronary endothelial or vascular smooth muscle cells. The only place where everybody can agree that there may be expression is in the sinoatrial node (24), which is where the GLP-1RAs are supposed to act when they generate increased heart rate, which they all do. Clearly, these findings cannot at present be used to explain the cardiovascular benefits of the GLP-1 RAs.
However, the great promise is that there is an effect in the clinical trials, and currently the best interpretation of the data seems to be that the GLP-1 RAs exert an anti-atherogenic effect, which shows up in a reduced rate of myocardial infarctions, sometimes reduced stroke (the good effects on blood pressure in the SUSTAIN 6 trial might contribute) and perhaps most clearly in the beneficial renal effects and the reduced frequency of revascularizations procedures (16). So, it may be justified to expect, as you start therapy with a GLP-1 RAs, that not only will you obtain a strong anti-diabetogenic effect (better than with any other agent in the second line of therapies of T2DM), but you may also be able to prevent, to some extent, atherosclerotic complications from occurring.
Thus, there are many good reasons why GLP-1RAs are recommended for second line therapy in T2DM.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has appeared on advisory boards for NovoNordisk.
References
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669-701. [Crossref] [PubMed]
- Holst JJ. The Physiology of Glucagon-like Peptide 1. Physiol Rev 2007;87:1409-39. [Crossref] [PubMed]
- Zhang Y, Sun B, Feng D, et al. Cryo-EM structure of the activated GLP-1 receptor in complex with a G protein. Nature 2017;546:248-53. [Crossref] [PubMed]
- Drucker DJ, Habener JF, Holst JJ. Discovery, characterization, and clinical development of the glucagon-like peptides. J Clin Invest 2017;127:4217-27. [Crossref] [PubMed]
- Kjems LL, Holst JJ, Volund A, et al. The Influence of GLP-1 on Glucose-Stimulated Insulin Secretion: Effects on beta-Cell Sensitivity in Type 2 and Nondiabetic Subjects. Diabetes 2003;52:380-6. [Crossref] [PubMed]
- Kapitza C, Dahl K, Jacobsen JB, et al. Effects of semaglutide on beta cell function and glycaemic control in participants with type 2 diabetes: a randomised, double-blind, placebo-controlled trial. Diabetologia 2017;60:1390-9. [Crossref] [PubMed]
- Vilsbøll T, Krarup T, Madsbad S, et al. Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 2002;45:1111-9. [Crossref] [PubMed]
- Hare KJ, Vilsboll T, Asmar M, et al. The Glucagonostatic and Insulinotropic Effects of Glucagon-Like Peptide-1 Contribute Equally to its Glucose-Lowering Action. Diabetes 2010;59:1765-70. [Crossref] [PubMed]
- Bunck MC, Corner A, Eliasson B, et al. Effects of exenatide on measures of beta-cell function after 3 years in metformin-treated patients with type 2 diabetes. Diabetes Care 2011;34:2041-7. [Crossref] [PubMed]
- Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 2016;375:311-22. [Crossref] [PubMed]
- Hjerpsted JB, Flint A, Brooks A, et al. Semaglutide improves postprandial glucose and lipid metabolism, and delays first-hour gastric emptying in subjects with obesity. Diabetes Obes Metab 2018;20:610-9. [Crossref] [PubMed]
- Hernandez AF, Green JB, Janmohamed S, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet 2018;392:1519-29. [Crossref] [PubMed]
- O’Neil PM, Birkenfeld AL, McGowan B, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet 2018;392:637-49. [Crossref] [PubMed]
- Secher A, Jelsing J, Baquero AF, et al. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest 2014;124:4473-88. [Crossref] [PubMed]
- Krieger JP, Arnold M, Pettersen KG, et al. Knockdown of GLP-1 Receptors in Vagal Afferents Affects Normal Food Intake and Glycemia. Diabetes 2016;65:34-43. [PubMed]
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2016;375:1834-44. [Crossref] [PubMed]
- Jensen EP, Poulsen SS, Kissow H, et al. Activation of GLP-1 receptors on vascular smooth muscle cells reduces the autoregulatory response in afferent arterioles and increases renal blood flow. Am J Physiol Renal Physiol 2015;308:F867-77. [Crossref] [PubMed]
- Muskiet MH, Tonneijck L, Smits MM, et al. GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes. Nat Rev Nephrol 2017;13:605-28. [Crossref] [PubMed]
- Skov J, Pedersen M, Holst JJ, et al. Short-term effects of liraglutide on kidney function and vasoactive hormones in type 2 diabetes: a randomized clinical trial. Diabetes Obes Metab 2016;18:581-9. [Crossref] [PubMed]
- Drucker DJ. The Cardiovascular Biology of Glucagon-like Peptide-1. Cell Metab 2016;24:15-30. [Crossref] [PubMed]
- Lang Lehrskov L, Lyngbaek MP, Soederlund L, et al. Interleukin-6 Delays Gastric Emptying in Humans with Direct Effects on Glycemic Control. Cell Metab 2018;27:1201-11.e3. [Crossref]
- Lebrun LJ, Lenaerts K, Kiers D, et al. Enteroendocrine L Cells Sense LPS after Gut Barrier Injury to Enhance GLP-1 Secretion. Cell Rep 2017;21:1160-8. [Crossref] [PubMed]
- Yusta B, Baggio LL, Koehler J, et al. GLP-1R Agonists Modulate Enteric Immune Responses Through the Intestinal Intraepithelial Lymphocyte GLP-1R. Diabetes 2015;64:2537-49. [Crossref] [PubMed]
- Pyke C, Heller RS, Kirk RK, et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology 2014;155:1280-90. [Crossref] [PubMed]
- Plamboeck A, Veedfald S, Deacon CF, et al. The effect of exogenous GLP-1 on food intake is lost in male truncally vagotomized subjects with pyloroplasty. Am J Physiol Gastrointest Liver Physiol 2013;304:G1117-27. [Crossref] [PubMed]
- Sisley S, Gutierrez-Aguilar R, Scott M, et al. Neuronal GLP1R mediates liraglutide’s anorectic but not glucose-lowering effect. J Clin Invest 2014;124:2456-63. [Crossref] [PubMed]
- Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in Patients with Type 2 Diabetes and Acute Coronary Syndrome. N Engl J Med 2015;373:2247-57. [Crossref] [PubMed]
- Holman RR, Bethel MA, Mentz RJ, et al. Effects of Once-Weekly Exenatide on Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 2017;377:1228-39. [Crossref] [PubMed]
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 2015;373:2117-28. [Crossref] [PubMed]
- Jorsal A, Kistorp C, Holmager P, et al. Effect of liraglutide, a glucagon-like peptide-1 analogue, on left ventricular function in stable chronic heart failure patients with and without diabetes (LIVE)-a multicentre, double-blind, randomised, placebo-controlled trial. Eur J Heart Fail 2017;19:69-77. [Crossref] [PubMed]
- Margulies KB, Hernandez AF, Redfield MM, et al. Effects of Liraglutide on Clinical Stability Among Patients With Advanced Heart Failure and Reduced Ejection Fraction: A Randomized Clinical Trial. JAMA 2016;316:500-8. [Crossref] [PubMed]
- Baggio LL, Yusta B, Mulvihill EE, et al. GLP-1 Receptor Expression Within the Human Heart. Endocrinology 2018;159:1570-84. [Crossref] [PubMed]


