
Comparison of readmission and early revision rates as a quality metric in total knee arthroplasty using the Nationwide Readmission Database
Introduction
The 2012 Affordable Care Act’s shift from a fee-for-service model to one associated with quality of care has grouped hospital and professional care into a single payment over a 90-day period for total knee arthroplasty (TKA) (1,2). As a result, reducing readmission rates for TKA, one of the most common and largest procedural expenditures for Medicare, has become a generally accepted quality metric and initial target for minimizing excess post-discharge costs (3,4). TKA readmission rates, however, tend to be relatively low compared to other major index procedures. For example, readmission rates at 30 days after discharge for spine, posterior spinal instrumentation, and hip fractures are all greater than 10% while TKA readmissions rates are significantly less, ranging from 2% and 6% (4,5). This makes improving TKA quality or reducing cost by decreasing already low readmission rates a challenge secondary to floor effects.
Reoperation procedures in the first year are an alternative metric that could be used to quantify quality. Early TKA complications have been well-documented and require surgical revision procedures (6,7). Unlike many reasons for readmission that include non-modifiable comorbidities such as congestive heart failure that are not related to the knee itself, reoperation within the first year represents a more modifiable factor related to the knee where the surgeon may have increased control. Long term follow-up of TKA has demonstrated implant survivorship of approximately 95% at 10 years (8). Minimizing revision rates at 1 year would naturally improve overall quality. Large national registries and administrative databases report a reoperation rate in the first year after TKA between 1% and 3.4% (6,9-11). This has a comparable scale to 30-day readmission rates that range between 2% and 6% (4,5). Although there is limited data outside of large centers documenting first year TKA revision rates, the New Zealand Joint Registry indicated that periprosthetic joint infection is the most common early complication encountered with a 0.8% reoperation rate within 1 year while accounting for 47% of all TKA reoperations (6). This suggests that first-year reoperation rates may have a comparable scale to readmission rates and that periprosthetic joint infection may be a major cause of reoperation. Readmission rates have not been directly compared to differences in reoperation rates after the index TKA. We have previously reported on readmission rates after TKA (1) as have other groups (12-15). There is no data available comparing the actual costs of these readmissions and reoperation procedures.
For these reasons, we compared national rates and costs for readmissions and reoperations following TKA in the United States. The Nationwide Readmissions Database (NRD) accounts for 49% of all hospitalizations in the United States and, as the largest database of all-payer hospital admissions, addresses gaps in readmission and revision data by following readmissions and reoperations across different hospitals (16). This database contains discharge data from the National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality. The objective of this study was to determine the reasons for TKA revisions and compare TKA revision rates and payments at approximately 1 year to readmission rates and payments at 30 and 90 days. We hypothesized that there would be little correlation between readmission rates and reoperation rates. Findings from this study provide important context and patterns in determining quality metrics for TKA procedures across all payers and geographic regions in the United States.
Methods
Data source and study population
We used the HCUP’s NRD to identify adult men and women who underwent TKA in 2013. The NRD provides a nationally representative dataset to examine hospital readmissions. Based on the State Inpatient Database, the NRD is the largest database of all-payer hospital admissions that contains patient linkages to follow readmissions across different hospitals in different states. The NRD website summarizes the core data file and data elements. This is a retrospective study as the dataset became available in 2016 (7). Missing data in this set was 0.08%.
We used the initial month of 2013 to follow readmission and reoperation episodes of care. Since the NRD is not linked between different years, we identified reoperations over the following 11 months in 2013 to calculate an approximate 1-year revision rate. We identified TKA index and revisions procedures using designated International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes. As there may be more than one procedure code for each patient, we included all patients with the ICD-9 procedure code 8154 (TKA) and excluded any patients with the ICD-9 procedure code 8151 (total hip arthroplasty), 8006 (arthrotomy for removal of prosthesis), 8155 (revision knee replacement), 0080 (revision knee replacement), 0081–0084 (revision knee replacement), 27486 (reconstruction of thigh region), 27487 (reconstruction of femur), 27488 (reconstruction of femur) and diagnosis codes 73310 (pathologic fracture), 73314 (pathologic fracture femoral neck), 73315 (pathologic fracture of other part of femur), 73316 (pathologic fracture of tibia), 808 (fracture of pelvis), 820 (femoral neck fracture), 821 (fracture of femur unspecified), 827 (multiple fractures of lower limb), 828 (multiple fracture of lower and upper limbs). The cohort starts with 21,044 eligible patients with qualified TKA admission. The qualified admission means age being 45 or older, no missing length of stay (LOS), not died in Hospital admission, January 2013 TKA admission and with TKA procedure and diagnosis code. After we excluded transfers, against Medical Advice, and discharged alive but destination unknown, there are 20,851 patients in the cohort.
Outcomes
The objective of this study was to assess readmission and reoperation rates among patients undergoing TKA. We defined a readmission as a hospital admission that occurred within two specific time periods (i.e., 30 and 90 days) of the index surgery that was not planned. We used 30 and 90 days to be consistent with the readmission definition used by the Hospital Readmissions Reduction Program and the time period included in the Comprehensive Care for Joint Replacement bundle, respectively (17). Revision rates were defined as a reoperation within 11 months of the initial index TKA population. If there were a series of readmissions for a single patient, only the first readmission was counted in determining the readmission rate. If there were a series of procedures for a single patient, only the first procedure was counted in determining the reoperation rate. The order of priority to count these observations included TKA revision procedure, excisional debridement, and non-excisional debridement. The reasons for revision procedures were determined using diagnosis and procedure codes as noted above. As a note, the National Readmission Database defines hospital size by bed number which varies based on geographic location. This does not represent overall arthroplasty procedure volume for the hospital.
Statistical analysis
We calculated the readmission and reoperation costs for each episode of care using an established method (18,19) based on total readmission and reoperation charges and hospital-specific cost-to-charge ratios developed by the HCUP (20). The cost-to-charge ratio provides a way to estimate the cost of hospital services, as opposed to the hospital charges. We determined mean readmission and reoperation costs and then calculated what the cost would be if distributed across the entire TKA population in our cohort.
We divided reoperation procedures between revision procedures and debridements. Revision procedure codes were defined as 00.80 (all component revision), 00.81 (tibial component revision), 00.82 (femoral component revision), 00.83 (patellar component revision), 00.84 (isolated tibial insert exchange), 80.06 (arthrotomy/removal of prosthesis), and 81.55 (revision TKA, not otherwise specified). Debridement was classified as either excisional (86.22) or non-excisional (86.28). Analyses were performed using SAS v9.4 (Cary, NC, USA).
Results
We identified 20,851 patients having TKA surgery across the states participating in NRD in the first month of 2013. Demographics of the cohort are described in Table 1. A comparison of reoperation and readmission rates in the first year of the index TKA procedure are described in Table 2. The mean unadjusted 30- and 90-day readmission rates were 3.4% and 5.8%, respectively. Although, there is little relevance in the current health care model, 1-year readmission rates were included for the sake of completeness. The mean unadjusted 3-month and approximate 1-year reoperation rates were 1.0% and 1.6%, respectively. The majority of the reoperation were from TKA revision surgical procedures (84%) as opposed to excisional or non-excisional debridements (16%).
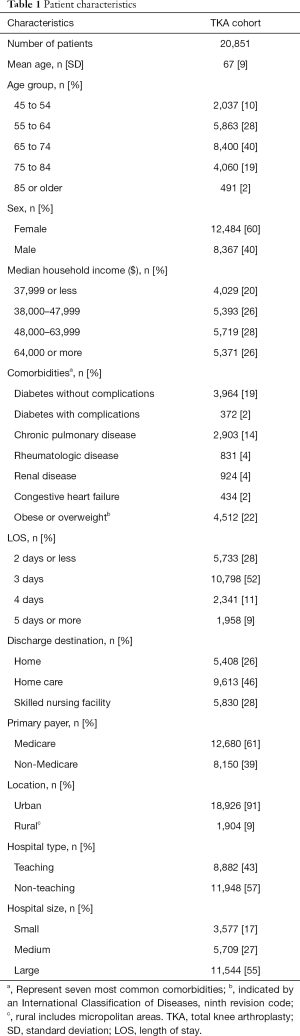
Full table
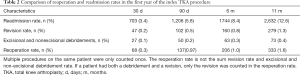
Full table
The most common causes for revision in the first year (Table 3) were periprosthetic joint infection (42.3%, n=242), other mechanical complication (13.8%, n=79), and dislocation of prosthetic joint (10%, n=57). Overall, periprosthetic joint infection accounted for 62% (n=242) of all reported revision procedures. This correlates with the most common procedure performed was isolated tibial insert revision (19.2%; Table 4). This diagnosis contributed to 56% (n=61) of all isolated tibial insert revisions, the most common revision procedure at 29% (n=110) of all identifiable procedures. The other most common surgical revision diagnoses were mechanical loosening of the prosthetic joint at 8% (n=36), dislocation of the prosthetic joint at 12% (n=57), and other mechanical complications at 17% (n=79). These diagnoses are the heaviest contributors to the femoral, patella, and tibial component revisions, respectively.
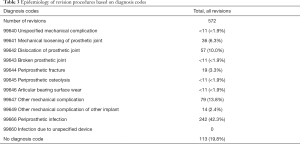
Full table

Full table
The costs of readmissions and reoperations were compared (Table 5). The average cost of each 30- and 90-day readmission episode was $9,936 (±$11,360) and $10,589 (±$11,084), respectively. In comparison, the mean inpatient cost of a single admission for a reoperation (revisions or debridement) ranged between $20,150 and $21,939. As debridements were a low percentage of overall procedures, mean revision costs during this time period ranged between $20,346 and $23,408. Distributed across the entire cohort, the 30- and 90-day readmission cost distributed across all TKA patients were $354 and $705, respectively. The approximate 1-year cost of reoperation and revision procedures were $396 and $310, respectively.
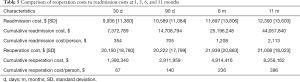
Full table
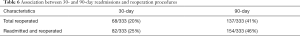
We performed a sensitivity analysis to examine if there was a relationship between patients readmitted at 30 or 90 days and patients who had a reoperation procedure (Table 6). At 30 days, 68 of the 333 readmissions (20%) had a reoperation. At 90 days, 137 of the 333 readmissions (41%) had a reoperation. At 1 year, 25% of patients readmitted at 30 days and 46% of patients readmitted at 90 days had a reoperation.
Full table
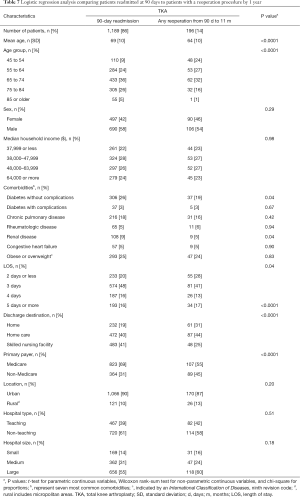
We performed a logistic regression analysis to determine if there were any correlations between patients readmitted at 90 days and those that later had a reoperation at 1 year (Table 7). There were 1,206 patients readmitted within 90 days and 196 patients with a reoperation. There were 16 patients that were both reoperated and readmitted and they were excluded in analysis. Age, diabetes, LOS more than 5 days, and primary payer were the only factors that predicted a correlation between a 90-day readmission and a later reoperation. Older patients with diabetes that had a LOS more than 5 days that were then readmitted had an increased risk of a reoperation within 1 year.
Full table
Discussion
Our study has three main findings that support the notion of looking at 1-year revision rates as a quality and value metric following TKA. First, the approximate 1-year revision and reoperation rate for TKA is comparable in magnitude to 30- and 90-day readmission rates. Second, the mean cost of reoperation procedures are twice the mean cost of 30- and 90-day readmissions, but when distributed across the entire TKA population, the costs are comparable in scale. Finally, the proportion of patients readmitted at 90 days that had a reoperation event at approximately 1 year from the index procedure was impressive (46%). These findings suggest the first year TKA reoperation rate has potential as a metric for quality and value as compared to readmission rates, but that 90-day readmission rates may be associated with these reoperations.
Reoperation rates at one year are comparable in scale to readmission rates at 30 and 90 days. Reoperation rates in TKA within a year were 1.8%. Readmission rates were 4% within 30 days and 5.8% within 90 days. These observed readmission rates are comparable to those previously reported in the literature (1,21-29). The Standard Analytical File 5% Sample Insurance Claims dataset reported overall revision arthroplasty or liner exchange rate of 3.4% (11). Our data are consistent with national registries, showing 1.0% to 1.2% revision rates [8]. Prior to ICD-9 diagnosis codes, 2-year revision rates in the Medicare database have been reported at approximately 3% [7]. Overall, our observations agree with these other large databases.
An important detail in our dataset is investigating the role of excisional and non-excisional debridements in the overall reoperation rate. The distinction between reoperation and revision rate is important. Reoperation rates include all surgical procedures related to the index procedure whereas revision rate includes surgical procedures with exchange of an implant related to the index procedure. Our study suggests that non-revision procedures (i.e., irrigation and debridement with no exchange of components) contribute little to the overall reoperation rate in the first year from the index procedure.
The primary cause of early revision during the first year in this population was periprosthetic joint infection. More than 60% of all reoperations were related to infection. The most common revision surgical procedure to treat infection was isolated tibial insert exchange. This adds evidence to the growing body of literature that infection remains the primary cause of both acute and long-term failure. Rates of early failure in the New Zealand registry were similar with almost 50% of all reoperations at 2 years (6). Infection was either the primary or major cause of failure at early and long-term time points in both single center studies (30-32) and other large registries and administrative databases (6,7,33).
Cost is an important measure of evaluating value in a surgical procedure. As care after a TKA has grouped hospital and professional care into a single payment over a 90-day period, the composition of cost in this period includes all aspects of a patient care including any readmission. Accurate measurement of the cost is challenging as this data is not widely available. An advantage of the NRD is access to cost data as compared to other administrative datasets. There is a large difference between what a medical facility charges for an episode of care and the actual cost of the episode of care. Although charge data is widely reported, few databases are able to provide the actual cost, allowing for a more accurate comparison. There is a paucity of data comparing actual cost of readmissions or reoperations. Per episode, the cost of reoperation was approximately twice the cost of each readmission episode. The combined cost of reoperation within 1 year was comparable in magnitude to the total cost of 30-day readmissions and almost half the cost of the 90-day readmission cost. Distributing the cost of each readmission and each reoperation across the entire TKA cohort demonstrated comparable magnitude of cost as well which is surprisingly low. Similar values have been reported previously (1).
We attempted to identify if there was a relationship between patients readmitted at 90 days and patients who had a reoperation procedure. At 90 days, 46% of patients readmitted at 90 days had a reoperation. A logistic regression analysis identified age, diabetes, LOS more than 5 days, and primary payer variables as variables that predicted patients readmitted at 90 days at risk for reoperation.
Our findings should be interpreted in the context of several limitations. There is a lack of laterality recorded with each revision procedure, and the ICD-9 code for TKA includes bilateral TKA and unicondylar knee procedures. This would potentially lead to revision procedures being incorrectly recorded when in fact the revision procedure was from the opposite knee or a unicondylar knee arthroplasty. As the observed revision rates in our study are comparable to other reported values in the literature (6), the incidence of this is small, and would not alter the overall interpretation of our results. A second possibility is that using ICD-9 criteria, debridement procedures are not location specific. This effect would over inflate contributions of reoperation rate to non-revision procedures. The fraction of reoperation rates was predominantly from revision procedures. Excisional and non-excisional debridements was a low percentage of reoperations. In a conservative measurement, when debridements are completely excluded, our overall conclusions would remain unchanged. A further limitation is that we were unable to track emergency room visits that resulted in a stay of less than 24 hours. By definition, any readmission that results in an inpatient stay is counted as a readmission. From this perspective, our readmission rate includes readmission for any reason outside of reoperations or revisions. Emergency room visits that do not result in an inpatient stay are not recorded. Finally, as with any database that represents a subset of the total population, there is a risk of bias due to a lack of generalizability. To help combat this issue, we used the NRD, which was specifically designed to address the lack of nationally representative readmission data for all ages and all payers. It includes 17 million readmission annually and, as a result, allowed us to evaluate over 20,000 TKA. The design of the NRD minimizes bias and allows the findings to be generalized to the majority of patients undergoing TKA in the United States.
The Center for Medicare and Medicaid Services’ Comprehensive Care for Joint Replacement bundle has specific goals for improving TKA outcomes (1). At an administrative level, hospital readmissions are being used to achieve this goal, but hospital readmission rates for TKA are low, especially in comparison to other episodes of care where readmission rates of 10–25% are used as a quality metric. This suggests that a floor effect has been approached and other metrics may be useful, in addition to readmission rates, to assess overall quality and value (1). We compared rates of readmission and 1-year reoperation. The magnitude of each were similar, but we were unable to observe variables that suggested a relationship between patients readmitted at 90 days and patients that had a reoperation at 1 year. This suggests that reoperation rates add additional information in assessing overall value and quality at an administrative level. This does not suggest that reoperation rates serve as reimbursement model or that reoperation rates should replace readmission rates as a quality metric. There are a number of outside influences in both reoperation rates and readmission rates. Examining reoperation rates within the first year may not only be a useful metric to assess overall quality, but also a useful tool for surgeons to identify patients at risk for a poor clinical outcome.
Acknowledgments
Funding: KLU is supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS K08AR071494), the National Center for Advancing Translational Science (NCATS KL2TR0001856), the Orthopaedic Research and Education Foundation, and the Musculoskeletal Tissue Foundation.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-19-3463). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. There were no animal studies conducted and therefore is exempt from IACUC approval and ARRIVE guidelines. This is a basic science article that does not include human subjects and is exempt from our institution’s IRB approval process.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Urish KL, Qin Y, Li BY, et al. Predictors and Cost of Readmission in Total Knee Arthroplasty. J Arthroplasty 2018;33:2759-63. [Crossref] [PubMed]
- Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. N Engl J Med 2015;372:897-9. [Crossref] [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Crossref] [PubMed]
- Ali AM, Gibbons CE. Predictors of 30-day hospital readmission after hip fracture: a systematic review. Injury 2017;48:243-52. [Crossref] [PubMed]
- D'Apuzzo M, Westrich G, Hidaka C, et al. All-cause versus complication-specific readmission following total knee arthroplasty. J Bone Joint Surg Am 2017;99:1093-103. [Crossref] [PubMed]
- Koh CK, Zeng I, Ravi S, et al. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res 2017;475:2194-201. [Crossref] [PubMed]
- Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 2010;468:45-51. [Crossref] [PubMed]
- Mont MA, Pivec R, Issa K, et al. Long-term implant survivorship of cementless total knee arthroplasty: a systematic review of the literature and meta-analysis. J Knee Surg 2014;27:369-76. [PubMed]
- Manley M, Ong K, Lau E, et al. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. J Arthroplasty 2009;24:1061-7. [Crossref] [PubMed]
- Heck DA, Melfi CA, Mamlin LA, et al. Revision rates after knee replacement in the United States. Med Care 1998;36:661-9. [Crossref] [PubMed]
- Patterson JT, Sing D, Hansen EN, et al. The James A. Rand Young Investigator's Award: Administrative Claims vs Surgical Registry: Capturing Outcomes in Total Joint Arthroplasty. J Arthroplasty 2017;32:S11-7. [Crossref] [PubMed]
- Nichols CI, Vose JG. Clinical outcomes and costs within 90 days of primary or revision total joint arthroplasty. J Arthroplasty 2016;31:1400-6.e3. [Crossref] [PubMed]
- Kurtz SM, Lau EC, Ong KL, et al. Which Clinical and Patient Factors Influence the National Economic Burden of Hospital Readmissions After Total Joint Arthroplasty? Clin Orthop Relat Res 2017;475:2926-37. [Crossref] [PubMed]
- Courtney PM, Ashley BS, Hume EL, et al. Are bundled payments a viable reimbursement model for revision total joint arthroplasty? Clin Orthop Relat Res 2016;474:2714-21. [Crossref] [PubMed]
- Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 2014;472:181-7. [Crossref] [PubMed]
- Healthcare Cost and Utilization Project (HCUP). Overview of the National (Nationwide) Inpatient Sample (NIS). Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp
- Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Available online: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
- Yu HY, Hevelone ND, Lipsitz SR, et al. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol 2012;187:1392-8. [Crossref] [PubMed]
- Sachs T, Pomposelli F, Hamdan A, et al. Trends in the national outcomes and costs for claudication and limb threatening ischemia: angioplasty vs bypass graft. J Vasc Surg 2011;54:1021-31.e1. [Crossref] [PubMed]
- Healthcare Cost and Utilization Project (HCUP). Overview of the State Inpatient Databases (SID). Available online: http://www.hcup-us.ahrq.gov/sidoverview.jsp
- Adelani MA, Keeney JA, Nunley RM, et al. Readmission following total knee arthroplasty: venous thromboembolism as a "never event" is a counterproductive misnomer. J Arthroplasty 2013;28:747-50. [Crossref] [PubMed]
- Avram V, Petruccelli D, Winemaker M, et al. Total joint arthroplasty readmission rates and reasons for 30-day hospital readmission. J Arthroplasty 2014;29:465-8. [Crossref] [PubMed]
- Huddleston JI, Maloney WJ, Wang Y, et al. Adverse events after total knee arthroplasty: a national Medicare study. J Arthroplasty 2009;24:95-100. [Crossref] [PubMed]
- Schaeffer JF, Scott DJ, Godin JA, et al. The association of ASA class on total knee and total hip arthroplasty readmission rates in an academic hospital. J Arthroplasty 2015;30:723-7. [Crossref] [PubMed]
- Tayne S, Merrill CA, Smith EL, et al. Predictive risk factors for 30-day readmissions following primary total joint arthroplasty and modification of patient management. J Arthroplasty 2014;29:1938-42. [Crossref] [PubMed]
- Zmistowski B, Restrepo C, Hess J, et al. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am 2013;95:1869-76. [Crossref] [PubMed]
- Ravi B, Croxford R, Austin PC, et al. Increased surgeon experience with rheumatoid arthritis reduces the risk of complications following total joint arthroplasty. Arthritis Rheumatol 2014;66:488-96. [Crossref] [PubMed]
- Singh JA, Lu X, Rosenthal GE, et al. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis 2014;73:2107-15. [Crossref] [PubMed]
- Ramkumar PN, Chu CT, Harris JD, et al. Causes and rates of unplanned readmissions after elective primary total joint arthroplasty: a systematic review and meta-analysis. Am J Orthop (Belle Mead NJ) 2015;44:397-405. [PubMed]
- Postler A, Lutzner C, Beyer F, et al. Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 2018;19:55. [Crossref] [PubMed]
- Le DH, Goodman SB, Maloney WJ, et al. Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res 2014;472:2197-200. [Crossref] [PubMed]
- Fehring TK, Odum S, Griffin WL, et al. Early failures in total knee arthroplasty. Clin Orthop Relat Res 2001.315-8. [Crossref] [PubMed]
- Delanois RE, Mistry JB, Gwam CU, et al. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 2017;32:2663-8. [Crossref] [PubMed]


