
Oncostatin M promotes the ox-LDL-induced activation of NLRP3 inflammasomes via the NF-κB pathway in THP-1 macrophages and promotes the progression of atherosclerosis
Introduction
Atherosclerosis is a chronic inflammatory disease of the blood vessels and the main underlying cause of cardiovascular diseases, including stroke, myocardial infarction, and heart failure (1). Despite the pathogenesis of atherosclerosis remaining unclear, smoking, alcohol, hyperlipidemia, hypertension, and genetic factors have been widely accepted as risk factors of atherosclerosis (2-4). Under these stimulations, low-density lipoprotein (LDL) is converted to oxidized LDL (ox-LDL) within the arterial walls, inducing endothelial cell dysfunction, platelet adhesion and aggregation, macrophage-derived foam cell formation, and smooth muscle cell migration (5). Ox-LDL, but not native LDL, is able to induce the production and release of pro-inflammatory cytokines causing inflammatory responses in macrophages and leading to chronic inflammation (6).
Inflammation plays a crucial role in the pathogenesis of atherosclerosis. Recently, NLR family pyrin domain containing 3 (NLRP3) has been considered a key regulator of the inflammatory response in atherosclerosis (7,8). NLRP3 recognizes various pathogen- and damage-associated molecular patterns to form NLRP3 inflammasomes containing NLRP3, apoptosis-associated, speck-like protein containing a caspase-1 recruitment domain (ASC), and caspase-1 (7). Pro-IL-1β and pro-IL-18 are then cleaved to the inflammatory cytokines IL-1β and IL-18, ultimately leading to an inflammatory response (9). The inhibition of NLRP3 has been shown to be effective in treating atherosclerosis and cardiovascular diseases (8,10,11). In addition, the NF-κB signaling pathway has been identified as a primary molecular mechanism of NLRP3 inflammasome activation (12,13).
Oncostatin M (OSM) is a member of the IL-6 family of cytokines generated from activated T cells, monocytes, and dendritic cells. As a cytokine secreted in response to infections and tissue injury, OSM participates in various cellular processes, including cell proliferation, death, differentiation, and hematopoiesis (14). In addition, OSM has significant roles in regulating various inflammatory diseases, such as inflammatory bowel diseases (15,16), lung inflammation (17), sepsis (18), and allergic rhinitis (19). Inhibition of the initiation and progression of atherosclerotic lesions using anti-thrombin agents leads to the downregulation of OSM (20,21). In atherosclerotic lesions, OSM is highly expressed and contributes to the proliferation and migration of smooth muscle cells (22). Moreover, OSM is able to promote endothelial activation (23) and chronic inflammation by binding to its receptors (22,24). Several studies have presented the link between OSM and atherosclerosis (14-24). The deficiency of OSM receptor β attenuated ameliorated atherosclerotic burden by inhibiting JAK2/STAT3 pathway (25). However, the roles of OSM in the pathogenesis of atherosclerosis have not been exhaustively investigated, especially the role of OSM in foam cell formation.
In the present study, a human monocytic leukemia cell line THP-1 was used and stimulated with phorbol-12-myristate-13-acetate (PMA) to induce macrophage differentiation. THP-1 macrophages were then exposed to ox-LDL, which is commonly used for mimicking a cell model of atherosclerosis (26). The effects of OSM on foam cell formation and inflammation induced by ox-LDL were evaluated. Moreover, considering OSM has been reported to be effective in inducing NLRP3 inflammasome activation (27), we further studied the involvement of NLRP3 in the effects of OSM on atherosclerosis. The findings of this study may provide a better understanding of OSM in the pathogenesis of atherosclerosis. We present the following article in accordance with the MDAR reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-560/rc).
Methods
THP-1 cell culture
Human acute monocytic leukemia cell line THP-1 was purchased from Procell Life Science & Technology Co., Ltd. (catalog number: CL-0233, Wuhan, China) and cultured in Roswell Park Memorial Institute (RPMI)-1640 medium (Gibco, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (Hyclone, Logan, UT, USA). Cells were maintained at 37 ℃ in an incubator with 5% CO2. To induce macrophage differentiation, THP-1 macrophages were incubated with 25 ng/mL PMA (MedChemExpress, Monmouth Junction, NJ, USA) for 24 hours and then incubated in a fresh culture medium for a further 24 hours.
Cells were treated with 10, 20, or 40 µg/mL of ox-LDL (Yiyuanbiotech, Shanghai, China) for 12, 24, or 48 hours. The non-treated cells were used as controls.
Cell transfection
OSM-specific small interfering RNAs (siRNAs) were purchased from GenePharma Co., (Shanghai, China). The following siRNA sequences were listed: si-OSM-1, 5'-GCCTGGATGTTCCTAAACTGA-3'; si-OSM-2, 5'-CAGACTCCT GGACCCCTATAT-3'; and si-NC, 5'-GTCGAATAGCGGTTACCACTT-3'. Full-length NLRP3 was amplified by polymerase chain reaction (PCR), and the PCR product was inserted into a pcDNA3.1 plasmid system (Invitrogen, Carlsbad, CA, USA) to construct an NLRP3 overexpression plasmid (pcNLRP3). Empty pcDNA3.1 was used as the negative control. Cell transfection was performed for 48 hours using the Lipofectamine 2000 reagent (Invitrogen).
Total cholesterol detection
Total cholesterol content was detected using a commercial kit (Nanjing Jiancheng Bioengineering Institute Co., Ltd., Nanjing, China) according to the manufacturer’s instructions.
Oil Red O staining
THP-1 macrophages were seeded in 6-well plates at a density of 2×105 cells/well. Following transfection and treatment, cells were washed twice with phosphate-buffered saline (PBS) and fixed with 4% paraformaldehyde for 30 minutes. The cells were stained with 0.5% Oil Red O (Sangon Biotech Co., Ltd., Shanghai, China) for 30 minutes at 23±2 ℃ and then incubated with 60% isopropanol for 10 seconds. The stained cells were photographed under a light microscope (Olympus, Tokyo, Japan). The intensity of the Oil Red O staining was detected at 540 nm under a microplate reader.
Enzyme-linked immunosorbent assay
The OSM, TNF-α, IL-1β, IL-6, and IL-18 content in the supernatant of THP-1 macrophages was measured using the corresponding enzyme-linked immunosorbent assay (ELISA) kits (Abcam, Cambridge, MA, USA) according to the manufacturer’s instructions.
Immunofluorescence
After transfection and treatment, the THP-1 macrophages in the 6-well plates were washed twice with PBS, fixed with 4% paraformaldehyde for 15 minutes, and incubated with 0.5% Triton X-100 for 20 minutes at 23±2 ℃. Normal goat serum was added to block the cells for 30 minutes. After removing the blocking solution, the cells were incubated with anti-NLRP3 primary antibody (1:300, catalog number: MA5-32255, Thermo Scientific, Rockford, IL, USA) overnight at 4 ℃ and with the secondary antibodies (1:500, catalog number: A32731, Thermo Scientific) for 1 hour at 37 ℃. Cell nuclei were stained by adding 4',6-diamidino-2-phenylindole (DAPI) for 5 minutes. The stained cells were photographed under a fluorescence microscope.
Quantitative reverse transcription PCR
Total RNA from the THP-1 macrophages was extracted using Trizol reagent (Beyotime, Shanghai, China). Reverse transcription (RT) was performed using the PrimeScript RT Master Mix (Perfect Real Time) (Takara, Dalian, China). Quantitative polymerase chain reaction (qPCR) was performed using the TB Green Fast qPCR Mix (Takara). The relative expression of the target genes was analyzed using the 2−ΔΔCt method and normalizing to glyceraldehyde 3-phosphate dehydrogenase (GAPDH). The primers were designed and synthesized by GenePharma. The following primer sequences were listed: OSM, 5'-GTGAACGGAACAGGTCTCCC-3' (forward), 5'-CAAGG ACCAGACCTTGTCAG-3' (reverse); NLRP3, 5'-CTGGCAT CTGGGGAAACCT-3' (forward), 5'-CTTAGGCTTCGGTCCACACA-3' (reverse); GAPDH, 5'-CCATGTTGCAACCGGGAAG-3' (forward), 5'-GCCCAAT ACGACCAAATCAGAG-3' (reverse).
Western blot analysis
Total protein from the THP-1 macrophages was extracted using radioimmunoprecipitation assay (RIPA) lysis buffer (Beyotime). The protein concentration of the extracts was analyzed using a bicinchoninic acid kit (Solarbio, Beijing, China). Equal amounts of protein extracts were loaded onto a 12% sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis and transferred onto polyvinylidene fluoride (PVDF) membranes (Millipore, Bedford, MA, USA). After blocking with 5% skim milk for 1 hour at 23±2 ℃, the membranes were incubated with the primary anti-OSM antibodies (1:1,000, catalog number: ab133748, Abcam), TNF-α (1:1,000, catalog number: ab215188, Abcam), IL-1β (1:1,000, catalog number: ab283818, Abcam), IL-6 (1:1,000, catalog number: ab233706, Abcam), IL-18 (1:1,000, catalog number: ab207324, Abcam), NF-κB p65 (1:1,000, catalog number: ab32536, Abcam), NF-κB p65 (phospho S529) (1:1,000, catalog number: ab109458, Abcam), NLRP3 (1:1,000, catalog number: MA5-32255, Thermo Scientific), caspase-1 (p20) (1:1,000, catalog number: PA1440, BosterBio, Pleasanton, CA, USA), ASC (1:1,000, catalog number: ab283684, Abcam), gasdermin-D (GSDMD)-N (1:1,000, catalog number: ab215203, Abcam), and GAPDH (1:1,000, catalog number: ab8245, Abcam). Following incubation with the secondary antibodies (1:1,000, catalog number: ab7090 and ab96879, Abcam), targeted bands were developed using the BeyoECL Plus kit (Beyotime).
Statistical analysis
Data presented as mean ± standard deviation (SD) were collected from 3 independent experiments in triplicate. Statistical analysis was performed by one-way analysis of variance (ANOVA) using GraphPad Prism 6.0 software (GraphPad Software, San Diego, CA, USA). A P value of less than 0.05 was considered significant.
Results
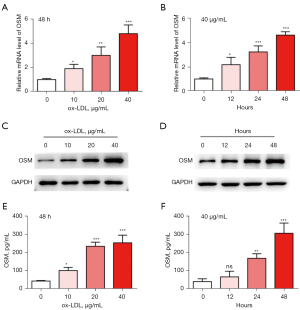
OSM is highly expressed in ox-LDL-treated THP-1 macrophages
THP-1 macrophages were subjected to various doses of ox-LDL, and the expression of OSM following 12, 24, and 48 hours of stimulation was detected. qRT-PCR results showed that the mRNA levels of OSM were significantly increased by ox-LDL treatment in both a dose- and time-dependent manner (P<0.05, Figure 1A,1B). Western blot analysis results showed that the protein levels of OSM were significantly increased by ox-LDL in a dose- and time-dependent manner (P<0.05, Figure 1C,1D). In addition, ELISA results indicated significantly high levels of OSM in the supernatant of THP-1 macrophages following ox-LDL treatment (P<0.05, Figure 1E,1F). The effects of ox-LDL on OSM levels were dose- and time-dependent. These results indicated a high expression of OSM in ox-LDL-treated THP-1 macrophages. In the following experiments, cells were treated with 40 µg/mL ox-LDL for 48 hours.
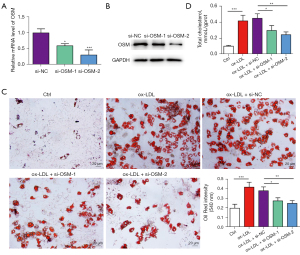
Silencing OSM inhibits ox-LDL-induced foam cell formation
Anti-OSM siRNAs were transfected into THP-1 macrophages to explore the role of OSM in atherosclerosis. Results showed that mRNA and protein levels of OSM were significantly repressed by transfection of cells with OSM siRNAs (P<0.05, Figure 2A,2B). Oil Red O staining results indicated that ox-LDL caused a significant increase in lipid accumulation (P<0.05, Figure 2C). Transfection of cells with OSM siRNAs significantly inhibited the Oil Red O staining level, compared to cells transfected with si-NC (P<0.05). We found that ox-LDL consistently caused a significant increase in total cholesterol content (P<0.05, Figure 2D). Cells transfected with OSM siRNAs showed much lower total cholesterol levels than cells transfected with si-NC (P<0.05). Taken together, these results showed that the silencing of OSM by siRNA transfection was effective in attenuating ox-LDL-induced foam cell formation.
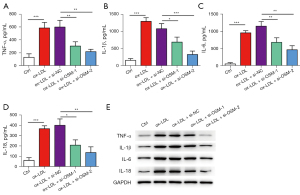
Silencing OSM inhibits ox-LDL-induced inflammation
After the indicated transfection and treatment, the supernatant of THP-1 macrophages was collected for ELISA analysis. The levels of TNF-α, IL-1β, IL-6, and IL-18 were significantly increased by ox-LDL treatment (P<0.05, Figure 3A-3D). Transfection of cells with OSM siRNAs significantly inhibited cytokine levels in contrast to transfection with si-NC (P<0.05). The protein levels of TNF-α, IL-1β, IL-6, and IL-18 were upregulated by ox-LDL in THP-1 macrophages (Figure 3E). OSM siRNAs inhibited the effects of ox-LDL on the protein expression of cytokines in contrast to si-NC. These data indicated that silencing OSM inhibited ox-LDL-induced cytokine release from THP-1 macrophages.
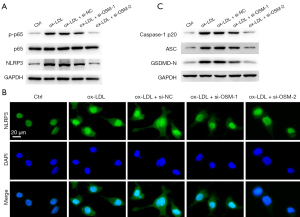
Silencing OSM inhibits ox-LDL-induced p65-NLRP3 pathway
The underlying mechanisms of OSM in the event of atherosclerosis were then detected. Western blot analysis (Figure 4A) showed that ox-LDL causes significant upregulation of NLRP3 and phosphorylated p65. Transfection of cells with OSM siRNAs repressed the activation of NLRP3 and p65, in contrast to si-NC transfection. Immunofluorescence results indicated a remarkably high expression of NLRP3 in ox-LDL-treated THP-1 macrophages (Figure 4B). In contrast to si-NC transfection, transfection of cells with OSM siRNAs inhibited NLRP3 expression induced by ox-LDL. Moreover, cleaved caspase-1 (p20), ASC, and GSDMD-N were all upregulated by ox-LDL (Figure 4C). In contrast to si-NC, OSM siRNAs remarkably inhibited the highly expressed caspase-1 (p20), ASC, and GSDMD-N.
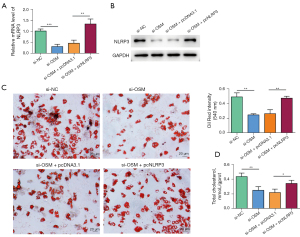
Silencing OSM inhibits foam cell formation via the inhibition of NLRP3
To further explore whether OSM exerted its effects via the regulation of NLRP3, an pcNLRP3 was transfected into THP-1 macrophages alone or in combination with OSM siRNA (si-OSM-2). Results indicated that mRNA and protein levels of NLRP3 were downregulated by OSM siRNA (P<0.05, Figure 5A) and upregulated by pcNLRP3 transfection (P<0.05, Figure 5B). Transfection of cells with pcNLRP3 significantly reversed the effects of OSM siRNA on lipid accumulation. In contrast to the si-OSM + pcDNA3.1 group, the Oil Red O staining levels and total cholesterol content were significantly increased in the si-OSM + pcNLRP3 group (P<0.05, Figure 5C,5D). These results indicated that silencing OSM inhibited foam cell formation, possibly via the inhibition of NLRP3 inflammasome activation.
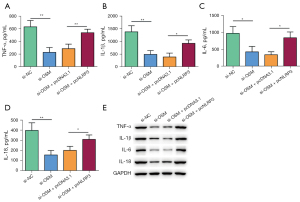
Silencing OSM inhibits inflammation via the inhibition of NLRP3
After transfection, cytokine levels in the supernatant of THP-1 macrophages were tested by ELISA. In contrast to the si-OSM + pcDNA3.1 group, the levels of TNF-α, IL-1β, IL-6, and IL-18 were significantly increased in the si-OSM + pcNLRP3 group (P<0.05, Figure 6A-6D). Consistent with this, the protein levels of TNF-α, IL-1β, IL-6, and IL-18 were upregulated in the si-OSM + pcNLRP3 group in contrast to those in the si-OSM + pcDNA3.1 group (Figure 6E). Based on these data, we concluded that silencing OSM inhibited ox-LDL-induced inflammation, possibly via the inhibition of NLRP3 inflammasome activation.
Discussion
Atherosclerosis is characterized by an imbalance in lipid metabolism, the accumulation of macrophage-derived foam cells, and inflammation of the artery walls (28). Macrophages play significant roles in atherosclerosis by participating in all stages of the disease progression (29). In the early stages of atherosclerosis, endothelial cells release chemokines to recruit monocytes and then induce macrophage differentiation. The macrophages further uptake ox-LDL and form foam cells, causing cell death and inflammation, which ultimately lead to plaque formation and instability. In the present study, THP-1 cells were treated with PMA to induce macrophage differentiation. THP-1 macrophages were exposed to ox-LDL to mimic a cell model of atherosclerosis. We found that OSM was highly expressed in the THP-1 macrophages following treatment with ox-LDL. The upregulation of OSM was time- and dose-dependent. The high expression of OSM in the cell model was consistent with several previous findings (20-22), suggesting a link between OSM and atherosclerosis. Silencing OSM expression by siRNA transfection significantly inhibited ox-LDL-induced foam cell formation, as evidenced by the decrease in the total cholesterol content and Oil Red staining levels. Silencing OSM inhibited ox-LDL-induced inflammation, as the production and release of TNF-α, IL-1β, IL-6, and IL-18 from THP-1 macrophages were significantly repressed. In addition, silencing OSM inhibited the ox-LDL-induced p65-NLRP3 signaling pathway. The effects of OSM silencing on ox-LDL-induced pathologic changes could be significantly reversed by NLRP3 overexpression. These data collectively suggested that OSM plays a role in inducing atherosclerosis by activating NLRP3 inflammasomes.
OSM, together with IL-6, IL-11, IL-31, and leukemia inhibitory factor (LIF), are members of the IL-6 family cytokines. All of them play essential roles in the immune system through cell communication and cell signaling pathways (30,31). OSM has garnered much interest due to its involvement in various inflammatory diseases. For instance, blockading OSM attenuated intestinal inflammation in an animal model of colitis (15). The administration of recombinant OSM protein in septic mice led to an increase in inflammatory tissue injury and a higher mortality rate (18). In C57Bl/6 mice, OSM induced lung inflammation by elevating IL-33 expression (17). OSM has been considered as a potential target for type 2 inflammatory diseases (32). In the present study, OSM was found to be critical in promoting the initiation and progression of atherosclerosis. OSM was highly expressed in ox-LDL-treated THP-1 macrophages in both a time- and dose-dependent fashion. Silencing OSM was effective in inhibiting ox-LDL-induced foam cell formation and inflammation in THP-1 macrophages. The effects of OSM on atherosclerosis with regard to smooth muscle cell migration (22), endothelium dysfunction (23), and chronic inflammation (22,24) have been previously reported. However, to our knowledge, this is the first study to explore the effects of OSM on promoting macrophage-derived foam cell formation.
NLRP3 plays a significant role in regulating the inflammatory response during atherosclerosis. It can be activated by various stimuli, including microbial infection, reactive oxygen species, high glucose, hypoxia, and particulate matter (13,33,34). In atherosclerotic lesions, NLRP3 can be activated by ox-LDL and cholesterol crystals (35). The activated NLRP3 forms an inflammasome complex together with ASC and caspase-1 and then cleavages pro-IL-1β and pro-IL-18 to contribute to a vascular inflammatory response. In this study, NLRP3 inflammasome activation was found in ox-LDL-treated THP-1 macrophages. This finding was consistent with previous studies (35-37), indicating the significant role of NLRP3-induced pyroptosis in atherosclerosis. We also found that silencing OSM inhibited NLRP3 inflammasome activation. The effects of OSM silencing on attenuating ox-LDL-induced foam cell formation and inflammation were reversed by NLRP3 overexpression. These data collectively suggested that OSM activated NLRP3 to promote ox-LDL-induced initiation of atherosclerosis. In addition, the expression of NF-κB p65 was detected as NF-κB is one of the main underlying signaling pathways of mediating NLRP3 inflammasome activation (12). We found that OSM silencing could inhibit the activation of NF-κB p65, indicating that OSM activated NLRP3 through the NF-κB signaling pathway.
To conclude, this study demonstrated that OSM was highly expressed in ox-LDL-treated THP-1 macrophages. Silencing OSM was effective in inhibiting ox-LDL-induced foam cell formation and inflammation in THP-1 macrophages. The beneficial effects of OSM silencing might include the inhibition of NF-κB-mediated NLRP3 inflammasome activation. Inhibition of OSM has the potential to delay the initiation and progression of atherosclerosis and related cardiovascular diseases.
Acknowledgments
Funding: This study was supported by the Clinical Medicine + X Research Project of the Affiliated Hospital of Qingdao University (project No. QDFY+X2021035).
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-560/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-560/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-560/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Frostegård J. Immunity, atherosclerosis and cardiovascular disease. BMC Med 2013;11:117. [Crossref] [PubMed]
- van Rooy MJ, Pretorius E. Obesity, hypertension and hypercholesterolemia as risk factors for atherosclerosis leading to ischemic events. Curr Med Chem 2014;21:2121-9. [Crossref] [PubMed]
- Mercado C, Jaimes EA. Cigarette smoking as a risk factor for atherosclerosis and renal disease: novel pathogenic insights. Curr Hypertens Rep 2007;9:66-72. [Crossref] [PubMed]
- Tegos TJ, Kalodiki E, Sabetai MM, et al. The genesis of atherosclerosis and risk factors: a review. Angiology 2001;52:89-98. [Crossref] [PubMed]
- Quinn MT, Parthasarathy S, Fong LG, et al. Oxidatively modified low density lipoproteins: a potential role in recruitment and retention of monocyte/macrophages during atherogenesis. Proc Natl Acad Sci U S A 1987;84:2995-8. [Crossref] [PubMed]
- Rhoads JP, Major AS. How Oxidized Low-Density Lipoprotein Activates Inflammatory Responses. Crit Rev Immunol 2018;38:333-42. [Crossref] [PubMed]
- Karasawa T, Takahashi M. Role of NLRP3 Inflammasomes in Atherosclerosis. J Atheroscler Thromb 2017;24:443-51. [Crossref] [PubMed]
- Duewell P, Kono H, Rayner KJ, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 2010;464:1357-61. [Crossref] [PubMed]
- Eren E, Özören N. The NLRP3 inflammasome: a new player in neurological diseases. Turk J Biol 2019;43:349-59. [Crossref] [PubMed]
- Sharma A, Choi JSY, Stefanovic N, et al. Specific NLRP3 Inhibition Protects Against Diabetes-Associated Atherosclerosis. Diabetes 2021;70:772-87. [Crossref] [PubMed]
- Abbate A, Toldo S, Marchetti C, et al. Interleukin-1 and the Inflammasome as Therapeutic Targets in Cardiovascular Disease. Circ Res 2020;126:1260-80. [Crossref] [PubMed]
- Afonina IS, Zhong Z, Karin M, et al. Limiting inflammation-the negative regulation of NF-κB and the NLRP3 inflammasome. Nat Immunol 2017;18:861-9. [Crossref] [PubMed]
- Luo B, Huang F, Liu Y, et al. NLRP3 Inflammasome as a Molecular Marker in Diabetic Cardiomyopathy. Front Physiol 2017;8:519. [Crossref] [PubMed]
- Stawski L, Trojanowska M. Oncostatin M and its role in fibrosis. Connect Tissue Res 2019;60:40-9. [Crossref] [PubMed]
- West NR, Hegazy AN, Owens BMJ, et al. Oncostatin M drives intestinal inflammation and predicts response to tumor necrosis factor-neutralizing therapy in patients with inflammatory bowel disease. Nat Med 2017;23:579-89. [Crossref] [PubMed]
- Li H, Feng C, Fan C, et al. Intervention of oncostatin M-driven mucosal inflammation by berberine exerts therapeutic property in chronic ulcerative colitis. Cell Death Dis 2020;11:271. [Crossref] [PubMed]
- Botelho F, Dubey A, Ayaub EA, et al. IL-33 Mediates Lung Inflammation by the IL-6-Type Cytokine Oncostatin M. Mediators Inflamm 2020;2020:4087315. [Crossref] [PubMed]
- Gong Y, Yan X, Sun X, et al. Oncostatin M Is a Prognostic Biomarker and Inflammatory Mediator for Sepsis. J Infect Dis 2020;221:1989-98. [Crossref] [PubMed]
- Kang HJ, Kang JS, Lee SH, et al. Upregulation of oncostatin m in allergic rhinitis. Laryngoscope 2005;115:2213-6. [Crossref] [PubMed]
- Preusch MR, Ieronimakis N, Wijelath ES, et al. Dabigatran etexilate retards the initiation and progression of atherosclerotic lesions and inhibits the expression of oncostatin M in apolipoprotein E-deficient mice. Drug Des Devel Ther 2015;9:5203-11. [Crossref] [PubMed]
- Kastl SP, Speidl WS, Katsaros KM, et al. Thrombin induces the expression of oncostatin M via AP-1 activation in human macrophages: a link between coagulation and inflammation. Blood 2009;114:2812-8. [Crossref] [PubMed]
- Albasanz-Puig A, Murray J, Preusch M, et al. Oncostatin M is expressed in atherosclerotic lesions: a role for Oncostatin M in the pathogenesis of atherosclerosis. Atherosclerosis 2011;216:292-8. [Crossref] [PubMed]
- van Keulen D, Pouwer MG, Pasterkamp G, et al. Inflammatory cytokine oncostatin M induces endothelial activation in macro- and microvascular endothelial cells and in APOE*3Leiden.CETP mice. PLoS One 2018;13:e0204911. [Crossref] [PubMed]
- Schnittker D, Kwofie K, Ashkar A, et al. Oncostatin M and TLR-4 ligand synergize to induce MCP-1, IL-6, and VEGF in human aortic adventitial fibroblasts and smooth muscle cells. Mediators Inflamm 2013;2013:317503. [Crossref] [PubMed]
- Zhang X, Li J, Qin JJ, et al. Oncostatin M receptor β deficiency attenuates atherogenesis by inhibiting JAK2/STAT3 signaling in macrophages. J Lipid Res 2017;58:895-906. [Crossref] [PubMed]
- Qin Z. The use of THP-1 cells as a model for mimicking the function and regulation of monocytes and macrophages in the vasculature. Atherosclerosis 2012;221:2-11. [Crossref] [PubMed]
- Lee HM, Kang J, Lee SJ, et al. Microglial activation of the NLRP3 inflammasome by the priming signals derived from macrophages infected with mycobacteria. Glia 2013;61:441-52. [Crossref] [PubMed]
- Liu X, Wu J, Tian R, et al. Targeting foam cell formation and macrophage polarization in atherosclerosis: The Therapeutic potential of rhubarb. Biomed Pharmacother 2020;129:110433. [Crossref] [PubMed]
- Kavurma MM, Rayner KJ, Karunakaran D. The walking dead: macrophage inflammation and death in atherosclerosis. Curr Opin Lipidol 2017;28:91-8. [Crossref] [PubMed]
- Houben E, Hellings N, Broux B. Oncostatin M, an Underestimated Player in the Central Nervous System. Front Immunol 2019;10:1165. [Crossref] [PubMed]
- Unver N, McAllister F. IL-6 family cytokines: Key inflammatory mediators as biomarkers and potential therapeutic targets. Cytokine Growth Factor Rev 2018;41:10-7. [Crossref] [PubMed]
- Pothoven KL, Schleimer RP. The barrier hypothesis and Oncostatin M: Restoration of epithelial barrier function as a novel therapeutic strategy for the treatment of type 2 inflammatory disease. Tissue Barriers 2017;5:e1341367. [Crossref] [PubMed]
- Franchi L, Muñoz-Planillo R, Núñez G. Sensing and reacting to microbes through the inflammasomes. Nat Immunol 2012;13:325-32. [Crossref] [PubMed]
- You Y, Huang Y, Wang D, et al. Angiotensin (1-7) inhibits arecoline-induced migration and collagen synthesis in human oral myofibroblasts via inhibiting NLRP3 inflammasome activation. J Cell Physiol 2019;234:4668-80. [Crossref] [PubMed]
- Grebe A, Hoss F, Latz E. NLRP3 Inflammasome and the IL-1 Pathway in Atherosclerosis. Circ Res 2018;122:1722-40. [Crossref] [PubMed]
- Sun Z, Li Y, Qian Y, et al. Celastrol attenuates ox-LDL-induced mesangial cell proliferation via suppressing NLRP3 inflammasome activation. Cell Death Discov 2019;5:114. [Crossref] [PubMed]
- Wu Q, He X, Wu LM, et al. MLKL Aggravates Ox-LDL-Induced Cell Pyroptosis via Activation of NLRP3 Inflammasome in Human Umbilical Vein Endothelial Cells. Inflammation 2020;43:2222-31. [Crossref] [PubMed]
(English Language Editor: L. Roberts)


