
Diagnostic yield of virtual bronchoscope navigation combined with radial endobronchial ultrasound guided transbronchial cryo-biopsy for peripheral pulmonary nodules: a prospective, randomized, controlled trial
Introduction
The early stage of lung cancer often has no obvious clinical symptoms and mainly manifests as peripheral pulmonary nodules (PPNs), which are observable in chest computed tomography (CT) scans. The early diagnosis of lung cancer is the main means by which the 5-year survival rate can be approved (1,2). With the expansion of the clinical application of chest CT examinations, the detection rate of PPNs has increased significantly. A technique urgently needs to be developed to improve the positive diagnosis rate of PPN. CT-guided lung biopsy is an important means for PPN diagnosis, but it has high complications, such as pneumothorax, hemorrhage, and gas embolism (3). In recent years, the clinical application of guided bronchoscopy, including ultra-bronchoscope, endobronchial ultrasound (EBUS), virtual bronchoscope navigation (VBN), and electromagnetic navigation (ENB), combined with transbronchial lung biopsy (TBLB) has significantly increased the diagnostic yield of PPNs, however tissues from PPLs obtained by TBLB are generally small, and the positive rate of diagnosis needs to be further improved (4-6). Transbronchial cryo-biopsy (TBCB) has been widely used in the clinical diagnosis of interstitial lung disease and peripheral pulmonary lesions (PPLs) with high safety and tolerability and can obtained larger tissue specimens than that obtained by TBLB (7-11), but there are few reports on the use of TBCB in the diagnosis of PPNs. This study sought to investigate the diagnostic yield of VBN combined with rEBUS-guided TBCB for PPN and expect to explore a new diagnostic method for PPNs. We present the following article in accordance with the CONSORT reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1231/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by institutional ethics committee of Zhoukou Central Hospital (No. 20190905006) and informed consent was taken from all the patients. This study is a prospective, randomized and two-parallel study, and allocation ratio was closed to 1:1. Patients with PPNs were enrolled who were required to undergo bronchoscopy to confirm the diagnosis in Henan Provincial People’s Hospital and Zhoukou Central Hospital from January 1, 2020 to December 31, 2020. The Henan Provincial People’s Hospital was informed and agreed with this study. The enrolled patients were divided into the TBCB group (experimental group) and the TBLB group (control group) using the block randomization method. The primary endpoint was the diagnostic yield of PPNs, and the secondary endpoints included the incidence of complications, operation time and specimen surface area.
Object of the study
- PPNs was defined as pulmonary nodules that occur below the segmental bronchus detected by lung thin-slice CT, or single or non-fused multiple nodular lesions in the lung parenchyma with a diameter ≤3 cm (12).
- Using the block randomization method, the statisticians of the project generated the random distribution table using SAS software, formulated the sealed and opaque random concealment letter printed by pinhole, and submitted it to the special person designated by the project coordination center (who did not participate in the clinical observation) for safekeeping.
- To be eligible for inclusion in the study, patients had to meet the following inclusion criteria: (i) be an aged 18–70 years old; (ii) agree to undergo a TBLB or TBCB inspection; (iii) agree to receive intraoperative anesthesia (local anesthesia, intravenous sedation, or general anesthesia); (iv) sign an informed consent form and agree to participate in this study; (v) have chest CT results that suggested bronchial signs in the target lesion.
- Participants were excluded from the study if they met any of the following exclusion criteria: (i) were pregnant; (ii) had severe anemia (hemoglobin <60 g/L, and platelet <60×109/L) or coagulation dysfunction; (iii) had uncontrolled cardiac insufficiency, respiratory failure, liver insufficiency, and renal insufficiency; (iv) the intraoperative radial ultrasound probe failed to detect the target lesion; (v) the intraoperative the target lesion could be directly observed by conventional tracheoscopy; (vi) had head and face trauma or a deformity that prevented the fiberoptic bronchoscope or rigid bronchoscope being inserted through the mouth or nose; (vii) did not agree to participate in this research project; and/or (viii) refused further examination during the study or were lost during the follow-up period.
Operation method of bronchoscopy
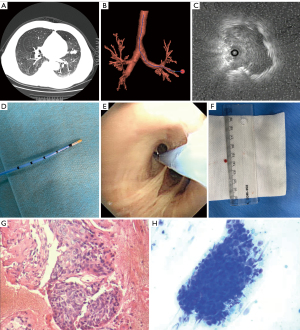
(I) VBN (Olympus DirectPath, Tōkyō-to, Japan) software was used to reconstruct bronchial 3-dimensional (3D) images and calculate the navigation path to the target lesions according to the chest CT data of the subjects; (II) under the anesthesia method, patients in the TBLB group received intravenous sedation and mucosal surface anesthesia with 5% lidocaine, while patients in the TBCB group received general anesthesia with endotracheal intubation or rigid bronchoscope ventilation, and the blocked balloon was routinely inserted into the target bronchus with the guidance of a bronchoscope before surgery; (III) the bronchoscope (Olympus BF-260) reached the target subsegment bronchus along the computer virtual navigation path. In the TBLB group, a radial ultrasound probe (Olympus UM-S20-17S) with a guided sheath (GS) was placed along the bronchoscopy biopsy channel to explore the target lesions. Following the exploration of the lesions, the ultrasound probe was withdrawn, the bronchoscope and GS were fixed, and biopsy forceps were placed for TBLB. In the TBCB group, a radial ultrasound probe without a GS was inserted into the bronchoscopy biopsy channel. After the lesions were explored, the ultrasound probe was withdrawn, the bronchoscope was fixed, and the cryoprobe (ERBE, Germany, length: 1,050 mm, diameter: 1.9 mm) was inserted for TBCB according to the distance measured by the ultrasonic probe. After 5 seconds of freezing, the bronchoscope and the cryo-probe were pulled out together, and the blocked balloon was opened at the same time. The probe with the specimen was placed in normal saline, and the maximum diameter and minimum diameter of the specimen were measured after thawing. The specimens were cut open for rapid on-site evaluation (ROSE); (IV) next the ROSE was performed. (i) In the TBLB group, the specimen was rolled on the slide, and the ROSE was performed after the first biopsy. If the diagnosis of the ROSE was malignant, 4–5 specimens were further biopsied, and all the specimens were fixed in formalin solution, and sent for pathological examination; If the diagnosis of the ROSE was benign, a second biopsy and ROSE was performed after the ultrasound probe had been re-adjusted to further explore the lesion. Regardless of whether the diagnosis of the ROSE was malignant or benign, 4–5 samples were biopsied, the operation was the terminated, and all specimens were fixed in formalin solution and sent for pathological examination; (ii) in the TBCB group, after the first TBCB, if the diagnosis of the ROSE was malignant, the operation was terminated, and the specimen was fixed with formalin, and sent for pathological examination. If no tumor cells were found, but severe bleeding occurred (13), the operation was also terminated and the specimen was fixed and sent for pathological examination; If no severe bleeding was observed, a further exploration with the ultrasound probe was performed, and the operation was terminated after the second TBCB. Both specimens were then sent for pathological examination; (V) the bronchoscope was removed after an observation of no bleeding in the target bronchus, and the operation was completed. Chest radiographs were examined 2 hours after the operation to observe whether pneumothorax appeared.
Observation index and follow-up plan
The baseline characteristics of the patients and target lesions were observed before the operation, including the age, gender, height, and weight of the patients, and the diameter, density, location, and distance from the parietal pleura of target lesion. The indexes, including the image features of the ultrasound localization of lesions, the results of the ROSE, the operation time of bronchoscopy, and the surface area of the biopsy specimens were observed.
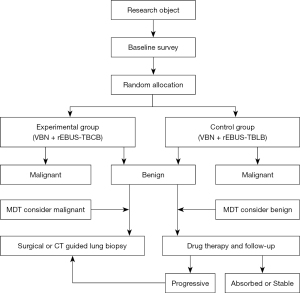
The patients were followed-up on the first day after the operation, and any complications were recorded, including bleeding, pneumothorax, postoperative fever, and pain. The histopathology from the bronchoscopic biopsy results were recorded 1 week after the operation. The patients whose histopathology results were malignant were considered to have a conclusive diagnosis, and the study was terminated. For the patients whose histopathology results were benign, multi-disciplinary team (MDT) was performed. the patient whose PPN was considered malignant by MDT underwent surgery or CT-guided lung biopsy, and after the postoperative pathological results were recorded, the study was terminated. Meanwhile, the patient whose PPN was considered benign by MDT underwent the corresponding treatment and was followed-up. A thin-slice CT of the chest was executed after 1 month, 3 months, and 6 months, and CT imaging changes of the target lesions were recorded. During the follow-up, if the CT images of the lesions of the patient were absorbed or stable, the diagnosis by bronchoscopy was considered to be a conclusive diagnosis and the study was terminated; however, if the CT images indicated progression, surgery, or CT-guided lung biopsy was performed (see Figure 1).
The bleeding grade was evaluated as follows (13): (I) no bleeding; (II) mild bleeding: negative pressure suction removed the bleeding, without other endoscopic hemostasis measures; (III) moderate bleeding: local injection of ice saline, 1:10,000 ice adrenaline dilution or bronchial occlusion balloon compression effectively stopped bleeding; or (IV) severe bleeding: hemodynamic or respiratory instability, and vascular intervention or other surgical operations, a blood transfusion, or admission to the ward was needed.
Pneumothorax was evaluated as follows: (I) the pneumothorax was self-absorbable; or (II) the pneumothorax required thoracic drainage.
Statistical analysis
SPSS 25.0 software was used for the statistical analysis. The measurement data are presented as the mean ± standard or median quartile distribution (skewness distribution), and differences between the groups were measured by the independent sample t-test or non-parametric test (skewness distribution). The counting data are presented as the number (percentage). The Chi-square or Fisher’s exact test was used for inter-group comparisons, and the Kappa test was used to evaluate the consistency of the two groups. For the test of normality of continuous variables, a two-sided P value of less than 0.05 was considered as statistically significant.
Results
Baseline comparison of population and target lesion characteristics
The recruitment date was January 1, 2020 to December 31, 2020, and the end date of follow-up was June 30, 2021. A total of 152 patients were enrolled in the study, but 14 patients were excluded during the study, and ultimately, 138 patients completed the study, including 71 patients in the TBLB group (39 males and 32 females with a mean age of 60.2±10.4 years), and 67 patients in the TBCB group (36 males and 31 females with a mean age of 61.5±11.6 years) (see Figure 2). In the TBLB group, there were 44 solid nodules (62.0%) and 27 mixed/ground glass nodules (38.0%). In the TBCB group, there were 30 solid nodules (44.8%) and 37 mixed/ground glass nodules (55.2%). In relation to the type of ultrasound image, 37 (52.1%) of the TBLB group were concentric, and 34 (47.9%) were eccentric and adjacent, and in the TBCB group, 35 (52.2%) were concentric and 32 (47.8%) were eccentric and adjacent. In the TBLB group, the target lesion diameter was 20.9±5.5 cm, and the distance to the pleura was 22.4±9.2 cm. In the TBCB group, the target lesion diameter was 19.2±6.0 cm, and the distance from the pleura was 24.5±10.0 cm. There was no significant difference between the two groups in terms of the baseline characteristics of the population and target lesions (see Table 1).
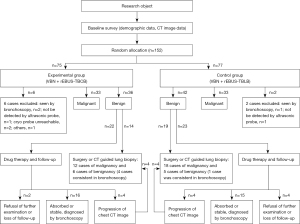
Table 1
| Subjects | Total | TBLB group | TBCB group | P |
|---|---|---|---|---|
| Population baseline characteristics | ||||
| Height (cm) | 167.5±8.8 | 166.4±8.7 | 168.5±8.9 | 0.486 |
| Weight (kg) | 65.3±9.3 | 64.3±9.2 | 66.3±9.4 | 0.728 |
| Age | 60.8±11.0 | 60.2±10.4 | 61.5±11.6 | 0.187 |
| Gender, n (%) | 0.890 | |||
| Male | 75 (54.3) | 39 (54.9) | 36 (57.3) | |
| Female | 63 (45.7) | 32(45.1) | 31(46.3) | |
| Feature of target lesion | ||||
| Density, n (%) | 0.122 | |||
| Solid | 74 (53.6) | 44 (62.0) | 30 (44.8) | |
| Mixed and ground glass | 64 (46.4) | 27 (38.0) | 37 (55.2) | |
| Location, n (%) | 0.975 | |||
| Right upper lobe | 36 (26.1) | 17 (23.9) | 19 (28.4) | |
| Right middle lobe | 21 (15.2) | 11 (15.5) | 10 (14.9) | |
| Right lower lobe | 24 (17.4) | 12 (16.9) | 12(17.9) | |
| Left upper lobe | 35 (25.4) | 19 (26.8) | 16 (23.9) | |
| Left lower lobe | 22 (15.9) | 12 (16.9) | 10 (14.9) | |
| Radial ultrasound localization, n (%) | 0.988 | |||
| Concentric | 72 (52.2) | 37 (52.1) | 35 (52.2) | |
| Eccentric and adjacent | 66 (47.8) | 34 (47.9) | 32 (47.8) | |
| Diameter (cm) | 20.10±5.8 | 20.9±5.5 | 19.2±6.0 | 0.281 |
| Distance from pleura (cm) | 23.4±9.6 | 22.4±9.2 | 24.5±10.0 | 0.232 |
TBLB, transbronchial lung biopsy; TBCB, transbronchial cryo-biopsy.
Diagnosis
In the TBLB group, 49 patients were diagnosed definitely by bronchoscopy, including 33 malignant cases and 16 benign cases. In the TBCB group, 53 cases were diagnosed definitely by bronchoscopy, including 33 malignant cases and 20 benign cases. Twenty-three cases were performed with Surgical or CT-guided lung biopsy in the TBLB group, and 18 cases in the TBCB group (see Table 2). The TBCB cases are shown in Figure 3.
Table 2
| Variables | TBLB group | TBCB group | Total |
|---|---|---|---|
| Malignant | 33 | 33 | 66 |
| Lung adenocarcinoma | 19 | 17 | 36 |
| Lung squamous cell carcinoma | 6 | 5 | 11 |
| Small cell lung cancer | 4 | 5 | 9 |
| Pulmonary metastatic carcinoma | 2 | 4 | 6 |
| Lung carcinoma in situ | 1 | 0 | 1 |
| Neuroendocrine carcinoma | 1 | 0 | 1 |
| Hematopoietic tumor | 0 | 1 | 1 |
| Adenoid cystic carcinoma | 0 | 1 | 1 |
| Benign | 16 | 20 | 36 |
| Chronic inflammation | 13 | 11 | 24 |
| TB | 1 | 3 | 4 |
| Granulomatous inflammation | 1 | 1 | 2 |
| Mechanized pneumonia | 1 | 2 | 3 |
| Acute inflammation | 0 | 2 | 2 |
| Fungal infection | 0 | 1 | 1 |
| Total | 49 | 53 | 102 |
TBLB, transbronchial lung biopsy; TBCB, transbronchial cryo-biopsy; TB, tuberculosis.
Diagnostic yield
The total diagnostic yield was 73.9% (102/138) for the two groups, 69.0% (49/71) for the TBLB group, and 79.1% (53/67) for the TBCB group; there was no statistically significant difference between the two groups. For lesions with a diameter ≥2 cm, the total diagnostic yield was 80.8% (63/78) for the two groups, 80.0% (36/45) for the TBLB group, and 81.8% (27/33) for the TBCB group; there was no statistically significant difference between the two groups. For PPNs with a diameter <2 cm, the total diagnostic yield was 65.0% (39/60) for the two groups, 50.0% (13/26) for the TBLB group, and 76.5% (26/34) for the TBCB group. Notably, the diagnostic yield of the TBCB group was higher than that of the TBLB group (P<0.05; see Table 3).
Table 3
| Variables | Diagnostic yield, % (n/N) | TBLB group, % (n/N) | TBCB group, % (n/N) | P |
|---|---|---|---|---|
| Diameter | ||||
| ≥2 cm | 80.8 (63/78) | 80.0 (36/45) | 81.8 (27/33) | 0.539 |
| <2 cm | 65.0 (39/60) | 50.0 (13/26) | 76.5 (26/34) | 0.033 |
| Density | ||||
| Solid | 82.4 (61/74) | 81.8 (36/44) | 83.3 (25/30) | 0.562 |
| Mixed and ground glass | 64.1 (41/64) | 48.1 (13/21) | 75.7 (28/37) | 0.023 |
| Localization | ||||
| Concentric | 80.5 (58/72) | 81.0 (30/37) | 80.0 (28/35) | 0.571 |
| Eccentric and adjacent | 66.7 (44/66) | 55.9 (19/34) | 78.1 (25/32) | 0.048 |
| Total | 73.9 (102/138) | 69.0 (49/71) | 79.1 (53/67) | 0.124 |
TBLB, transbronchial lung biopsy; TBCB, transbronchial cryo-biopsy.
For the solid lesions, the total diagnostic yield was 82.4% (61/74) for the two groups, 81.8% (36/44) for the TBLB group, and 83.3% (25/30) for the TBCB group; there was no statistically significant difference between the two groups. For the mixed and ground glass lesions, the total diagnostic yield was 64.1% (41/64) for the two groups, 48.1% (13/21) for the TBLB group, and 75.7% (28/37) for the TBCB group; there was no statistically significant difference between the two groups (see Table 3). The total diagnostic yield of lesions with concentric ultrasonic images was 80.5% (58/72) for the two groups, and 81.0% (30/37) for the TBLB group, and 80.0% (28/35) for the TBCB group, there was no statistically significant difference between the two groups. For the eccentric and adjacent lesions, the diagnostic yield was 66.7% (44/66) for the two groups, 55.9% (19/34) for the TBLB group, and 78.1% (25/32) for the TBCB group. Notably, the diagnostic yield for eccentric and adjacent lesions was higher in the TBCB group than the TBLB group (P<0.05; see Table 3).
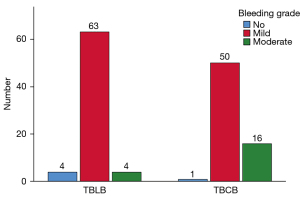
Incidence of complications
There were mild and moderate bleeding in both groups during the operation. In the TBLB group, the incidence of mild and moderate bleeding was 88.7% (63/71), and 5.6% (4/71), respectively. In the TBCB group, the incidence of mild and moderate bleeding was 74.6% (50/67) and 22.5% (16/71), respectively. The incidence of moderate bleeding in the TBCB group was higher than that in the TBLB group (P=0.006; see Figure 4). There were 2 cases of pneumothorax in the TBLB group and 3 cases in the TBCB group, none of which were treated with thoracic drainage. No serious complications were observed in either group.
The diagnostic consistency of ROSE and histopathology
Among the 152 enrolled patients, 144 patients completely underwent TBLB or TBCB with the guidance of VBN-rEBUS. Histopathology results showed 66 malignant cases in which 58 malignant cases and 8 benign cases were diagnosed by ROSE. Histopathology results showed 78 benign cases in which 69 benign cases and 9 malignant cases were diagnosed by ROSE. The ROSE results were consistent with the bronchoscopic pathological results (see Figure 5).
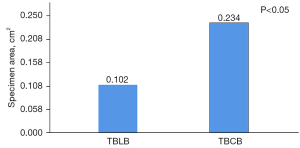
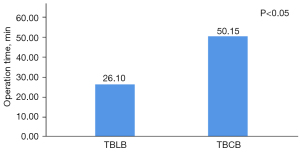
Specimen surface area and operation time
The specimen surface area of the TBLB group was 0.102±0.023 cm2, and that of the TBCB group was 0.234±0.032 cm2, and the difference between the two groups was statistically significant (P=0.030; see Figure 6). The operation time of the TBLB group was 26.10±5.40 min, and that of the TBCB group was 50.15±6.22 min, and the difference between the two groups was statistically significant (P=0.034; see Figure 7).
Discussion
The small ultrasonic probe helped to locate and sample the lesions located in the distal bronchus, bronchioles, and alveoli. Combined with the characteristics of the lesions, the radial ultrasonic localization images of PPNs can be divided into the following 3 types: concentric, eccentric, and adjacent (10). VNB is a method for forming a 3D, virtual bronchial tree image, which is generated by importing chest CT data into a special system, and can guide the bronchoscope to the peripheral lung target lesions (14). Gupta et al. reported that the diagnostic yield of rEBUS-TBLB for PPN was about 60–70%, but when used in combination with VBN, the diagnostic yield reached 63.3–84% (15). In this study, VNB-rEBUS was used, and the total diagnostic yield was 73.9% (102/138). Similar to the findings of a previous study (15), in this study, the application of VNB-rEBUS combined with GS in the TBLB group resulted in a diagnostic yield of 70.4% (57/81).
In the early stage of its clinical application, the cryo-technology was mainly applied to the cyro-biopsy of lesions in the bronchial lumen and the cryoablation treatment of central airway stenosis (16). In recent years, the technology has been applied to the diagnosis of interstitial lung disease, and has been shown to have a high diagnostic yield and safety. Indeed, a meta-analysis showed that the diagnostic yield of cyro-biopsy for interstitial lung disease was 74–98% (17). Schuhmann et al. compared TBCB to conventional biopsy for the diagnosis of PPL, and found that it significantly improved the diagnostic yield (11). Conversely, Kho et al. reviewed the diagnostic value of EBUS-guided TBCB for PPL, and found that compared to conventional biopsy, TBCB did not improve the diagnostic yield (85.7% vs. 77.1%). However, for target lesions with eccentric and adjacent radial ultrasound images, the diagnostic yield of the TBCB group was 66.7%, which was significantly higher than the 22% diagnostic yield of the biopsy group (10). The difference between the results may be related to the different proportions of radial ultrasonic image type (concentric, eccentric, and adjacent). In this study, PPNs with a diameter ≤3 cm were enrolled. The study showed that the diagnostic yield of the TBCB group was not significantly higher than that of the TBLB group (79.1% vs. 69.0%), but for the PPNs with eccentric and adjacent images, the diagnostic yield of the TBCB group was higher than that of the TBLB group (78.1% vs. 55.9 %). Similarly, for PPNs with a diameter <2 cm, the diagnostic yield of the TBCB group was higher than that of the TBLB group (76.5% vs. 50.0%), while for PPNs with a concentric ultrasonic image or a diameter ≥2 cm, there was no significant difference between the two groups (80.0% vs. 81.0% vs. 81.8% vs. 80.0%). TBLB can only sample smaller tissues, while TBCB can sample the tissue of the target lesion within 360 degrees with a larger contact area. Thus, TBCB may have a diagnostic advantage for eccentric and adjacent lesions.
Bleeding is the most common complication for TBCB. In a meta-analysis of 12 studies, moderate bleeding was observed after TBCB in 65 of 383 patients (16.9%), with an overall probability of 0.12 [95% confidence interval (CI): 0.02–0.25] (17). In addition to guiding the biopsy tool to the target lesion, EBUS can also detect whether there are large blood vessels in the biopsy area, and thus reduce the risk of bleeding (15). Schuhmann et al. performed 63 rEBUS-guided cryo-biopsies in 31 patients with PPL, and only 1 patient experienced moderate bleeding (11). In the study of TBCB application in PPL conducted by Imabayashi et al., mild bleeding occurred in 25 of 38 patients, but moderate bleeding occurred in only 1 patient. Additionally, 2 patients developed pneumothorax requiring catheterization, both of which were related to the close proximity of the patients’ lesions to the pleura (18). In this study, rEBUS was used in both groups, but the GS was only used in the TBLB group, and was not used in the TBCB group, as the GS could have prevented the cryo-probe from reaching target lesions; rather, a blocked balloon was used to prevent severe bleeding. The study showed that the incidence of moderate bleeding in the TBCB group was higher than that of the TBLB group (22.5% vs. 5.6%). No serious bleeding occurred in either group. Pneumothorax is another common complication of TBCB. A meta-analysis involving 13 studies on the application of cryotherapy in interstitial diseases showed that the incidence of pneumothorax after TBCB was 9.5% (95% CI: 5.9–14.9%) (19). In this study, there were 2 cases of pneumothorax in the TBLB group and 3 cases in the TBCB group, none of which underwent thoracic drainage.
The efficiency of TBCB is related to cryo-time, cryo-probe size, the nature of the target tissue, the local temperature, and other factors (20,21). Currently, two types of cryo-probes are commonly used (i.e., the 2.4- and 1.9-mm cryo-probes), and the cryo-time is 3–6 s. A few studies have shown that the TBCB specimens were significantly larger than the TBLB specimens used in the diagnosis of peripheral lung cancer, and the success yield of the later molecular pathological examinations was higher than that of the control group (22,23). To effectively reach the target lesions, the 1.9-mm probe was chosen in this study, and the cryo-time was 5 s. The results showed that the surface area of the TBCB specimens was larger than that of the TBLB specimens (0.234±0.031 vs. 0.102±0.023 cm2). To reduce the risk of surgery, TBCB was performed with a rigid bronchoscope or endotracheal intubation after general anesthesia, while TBLB was performed after sedation, which may be the main reason why the operation time of the TBCB group was significantly longer than that of the TBLB group (50.15±6.22 vs. 26.10±5.40 min).
ROSE provides on-site evaluations for specimens, quickly provides a preliminary diagnosis, and provides guidance on how to adjust the next steps to maximize the diagnostic yield. When ROSE was applied for the diagnosis of PPLs combined with rEBUS-TBLB, it improved the diagnostic yield and reduced the operation time (24). In this study, ROSE was applied for the preliminary diagnosis of the target lesions in both the groups. The results showed that the ROSEs and histopathology examinations were consistent in terms of the diagnosis of benign and malignant lesions (Kappa value =0.763).
However, it should be noted that this study had a number of limitations. First, the sample size of the enrolled patients was limited, and only 2 clinical hospitals participated in the study. Thus, the results need to be confirmed by more large-scale clinical studies. Second, the follow-up time was only 6 months, which is short, and some malignant PPNs remained unchanged during the follow-up period and were considered benign, which could affect the research results. Third, at present the factors affecting the diagnostic yield of TBCB for PPNs need to be examined further, including the diameter of cryo-probe and cryo-time. Additionally, the question of whether the diagnostic yield can be improved by using a cryo-probe with a diameter of 2.4 mm and extending the cryo-time needs to be further studied.
In conclusion, this study demonstrated that VBN-rEBUS-guided TBCB has a better diagnostic yield and safety for PPNs, especially for lesions with eccentric and adjacent ultrasound images and a diameter ≤2 cm. The specimens obtained by TBCB were significantly larger than those obtained by TBLB, which may be more conducive to subsequent molecular pathological examinations. The moderate bleeding rate of TBCB was higher than that of TBLB, but no serious complications were observed.
Acknowledgments
Funding: This study was supported by the Zhoukou Central Hospital Science and Technology Project (No. 20190101).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1231/rc
Trial Protocol: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1231/tp
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1231/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1231/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by institutional ethics committee of Zhoukou Central Hospital (No. 20190905006) and informed consent was taken from all the patients. The Henan Provincial People’s Hospital was informed and agreed with this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ettinger DS, Wood DE, Aisner DL, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 2.2021. J Natl Compr Canc Netw 2021;19:254-66. [Crossref] [PubMed]
- Babar L, Modi P, Anjum F. Lung Cancer Screening. StatPearls. Treasure Island (FL); 2022.
- Simoff MJ, Lally B, Slade MG, et al. Symptom management in patients with lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e455S-97S.
- Oki M, Saka H, Asano F, et al. Use of an Ultrathin vs Thin Bronchoscope for Peripheral Pulmonary Lesions: A Randomized Trial. Chest 2019;156:954-64. [Crossref] [PubMed]
- Chen Q, An Z, Cheng J, et al. Advances of Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions. Zhongguo Fei Ai Za Zhi 2020;23:440-5. [PubMed]
- Ishiwata T, Gregor A, Inage T, et al. Bronchoscopic navigation and tissue diagnosis. Gen Thorac Cardiovasc Surg 2020;68:672-8. [Crossref] [PubMed]
- Pajares V, Puzo C, Castillo D, et al. Diagnostic yield of transbronchial cryobiopsy in interstitial lung disease: a randomized trial. Respirology 2014;19:900-6. [Crossref] [PubMed]
- Hetzel J, Maldonado F, Ravaglia C, et al. Transbronchial Cryobiopsies for the Diagnosis of Diffuse Parenchymal Lung Diseases: Expert Statement from the Cryobiopsy Working Group on Safety and Utility and a Call for Standardization of the Procedure. Respiration 2018;95:188-200. [Crossref] [PubMed]
- Pajares V, Núñez-Delgado M, Bonet G, et al. Transbronchial biopsy results according to diffuse interstitial lung disease classification. Cryobiopsy versus forceps: MULTICRIO study. PLoS One 2020;15:e0239114. [Crossref] [PubMed]
- Kho SS, Chan SK, Yong MC, et al. Performance of transbronchial cryobiopsy in eccentrically and adjacently orientated radial endobronchial ultrasound lesions. ERJ Open Res 2019;5:e00135-2019. [Crossref] [PubMed]
- Schuhmann M, Bostanci K, Bugalho A, et al. Endobronchial ultrasound-guided cryobiopsies in peripheral pulmonary lesions: a feasibility study. Eur Respir J 2014;43:233-9. [Crossref] [PubMed]
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology 2017;284:228-43. [Crossref] [PubMed]
- Ernst A, Eberhardt R, Wahidi M, et al. Effect of routine clopidogrel use on bleeding complications after transbronchial biopsy in humans. Chest 2006;129:734-7. [Crossref] [PubMed]
- Jiang J, Chang SH, Kent AJ, et al. Current Novel Advances in Bronchoscopy. Front Surg 2020;7:596925. [Crossref] [PubMed]
- Gupta A, Youness H, Dhillon SS, et al. The value of using radial endobronchial ultrasound to guide transbronchial lung cryobiopsy. J Thorac Dis 2019;11:329-34. [Crossref] [PubMed]
- Hetzel J, Hetzel M, Hasel C, et al. Old meets modern: the use of traditional cryoprobes in the age of molecular biology. Respiration 2008;76:193-7. [Crossref] [PubMed]
- Ravaglia C, Bonifazi M, Wells AU, et al. Safety and Diagnostic Yield of Transbronchial Lung Cryobiopsy in Diffuse Parenchymal Lung Diseases: A Comparative Study versus Video-Assisted Thoracoscopic Lung Biopsy and a Systematic Review of the Literature. Respiration 2016;91:215-27. [Crossref] [PubMed]
- Imabayashi T, Uchino J, Yoshimura A, et al. Safety and Usefulness of Cryobiopsy and Stamp Cytology for the Diagnosis of Peripheral Pulmonary Lesions. Cancers (Basel) 2019;11:410. [Crossref] [PubMed]
- Iftikhar IH, Alghothani L, Sardi A, et al. Transbronchial Lung Cryobiopsy and Video-assisted Thoracoscopic Lung Biopsy in the Diagnosis of Diffuse Parenchymal Lung Disease. A Meta-analysis of Diagnostic Test Accuracy. Ann Am Thorac Soc 2017;14:1197-211. [Crossref] [PubMed]
- Franke KJ, Szyrach M, Nilius G, et al. Experimental study on biopsy sampling using new flexible cryoprobes: influence of activation time, probe size, tissue consistency, and contact pressure of the probe on the size of the biopsy specimen. Lung 2009;187:253-9. [Crossref] [PubMed]
- Ing M, Oliver RA, Oliver BG, et al. Evaluation of Transbronchial Lung Cryobiopsy Size and Freezing Time: A Prognostic Animal Study. Respiration 2016;92:34-9. [Crossref] [PubMed]
- Arimura K, Kondo M, Nagashima Y, et al. Comparison of tumor cell numbers and 22C3 PD-L1 expression between cryobiopsy and transbronchial biopsy with endobronchial ultrasonography-guide sheath for lung cancer. Respir Res 2019;20:185. [Crossref] [PubMed]
- Arimura K, Tagaya E, Akagawa H, et al. Cryobiopsy with endobronchial ultrasonography using a guide sheath for peripheral pulmonary lesions and DNA analysis by next generation sequencing and rapid on-site evaluation. Respir Investig 2019;57:150-6. [Crossref] [PubMed]
- Xu C, Wang W, Yuan Q, et al. Rapid On-Site Evaluation During Radial Endobronchial Ultrasound-Guided Transbronchial Lung Biopsy for the Diagnosis of Peripheral Pulmonary Lesions. Technol Cancer Res Treat 2020;19:1533033820947482. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)



