High-density lipoprotein cholesterol values independently and inversely predict cardiac troponin T and I concentration
Introduction
The most recent statistics of the American Heart Association (AHA) attests that although the mortality rate for cardiovascular disorders (CVD) has declined in the United States, the burden remains regrettably high (1). More specifically, the acute coronary syndrome (ACS) alone causes approximately 1 of every 7 deaths in the United States, averaging as many as 375,295 deaths annually. Globally, one American resident experiments a coronary event approximately every half minute and one American dies for heart attack approximately every 1 and half minute (1). Similar figures are reported at different latitudes. For example, despite the local government has taken an active part in prevention and control of CVD, the morbidity and mortality for heart attacks are both persistently increasing in China (2). In fact, it is currently reported that approximately 230 million patients suffer from CVD in this country, and 2 million patients suffer or have suffered from ACS. Notably, 3 million cases of death for heart attack are recorded each year, accounting for nearly 41% of the overall mortality in China (2).
The biochemical gold standard for diagnosing ACS, both ST-elevation myocardial infarction (STEMI), and especially non-ST-elevation myocardial infarction (NSTEMI), is represented by cardiac troponins testing. Due to their virtually absolute cardiospecificity, the assessment of either cardiac troponin T (TnT) or troponin I (TnI) is recommended by international validated guidelines for identifying myocardial injuries, thus including ACS (3-5). Despite their unquestionable role for diagnosing acute myocardial injury, several lines of evidence now attest that the concentration of cardiac troponins, especially when measured with the new high-sensitivity (HS) immunoassays, is a significant predictor of death (both total and cardiovascular), in patients with CVD (6), as well as in those without (7). This evidence is convincingly persuading that cardiac troponins may be regarded as a kind of “cholesterol of the third millennium”, which may provide clinically meaningful information not only for diagnosing ACS, but also for stratifying the cardiovascular risk in the general population, alone or in combination with traditional cardiovascular risk factors such as blood lipids, hypertension and diabetes among others (8).
The National Cholesterol Education Program (NECP) currently defines an increased risk of CVD in subjects bearing total cholesterol (TC) values greater than 5.2 mmol/L (i.e., 200 mg/dL), low-density lipoprotein cholesterol (LDL-C) values greater than 2.6 mmol/L (i.e., 100 mg/dL) and high-density lipoprotein cholesterol (HDL-C) values lower than 1.0 mmol/L (i.e., 40 mg/dL) (9). Therefore, we planned a retrospective study to establish the existence of potential associations between circulating values of cardiac troponins and those of conventional blood lipids in a population of patients admitted to inpatient clinics for routine cardiovascular risk assessment.
Materials and methods
The study population consisted of patients attending an inpatient clinic of the University Hospital of Verona during the entire year 2015, as part of routine cardiovascular risk assessment. No exclusion criteria were applied in order to collect the largest possible number of subjects and thereby increase the statistical significance of potential associations. Serum lipids, thus including TC, HDL-C and triglycerides (TG) were measured using reference enzymatic techniques on Roche Cobas 6000 (Roche Diagnostics, Basel, Switzerland), whereas LDL-C was calculated using Friedewald equation. The concentration of TnT was also measured on Roche Cobas 6000, using a HS immunoassay (Roche). The limit of blank (LOB) and the 99th percentile of the upper reference limit (URL) of this assay are 3 and 14 ng/L, respectively (10). Patients with HS-TnT values lower than the LOB and those above 100 ng/L were excluded from the statistical analysis. The 100 ng/L cut-off was arbitrarily chosen for decreasing the chance of including patients with overt myocardial injury. A threshold of 50 ng/L (i.e., ~3-times the URL of Roche HS-TnT) was prespecified.
In order to replicate results with TnI, a second analysis was performed in the second hospital of the town (i.e., Verona General Hospital), by extracting data from the local laboratory database of all patients in whom TnI and blood lipids were simultaneously measured during the entire year 2015. As for TnT analysis, no exclusion criteria were applied in order to collect the largest possible number of subjects and thereby increase the statistical significance of potential associations. In this second analysis, serum lipids were measured with Siemens Dimension Vista (Siemens Healthcare Diagnostics, Tarrytown, NY, USA) using reference enzymatic techniques, whereas LDL-C was also calculated using the Friedewald equation. The concentration of TnI was also measured on Siemens Dimension Vista (Siemens Healthcare Diagnostics), by using a contemporary-sensitive assay based on luminescent oxygen channeling (LOCI) technology (11). The LOB and URL of this assay are 15 and 45 ng/L, respectively (10). As for TnT data, patients with TnI values lower than the LOB and those above 100 ng/L were excluded from the statistical analysis. A threshold of 50 ng/L (i.e., ~3-times the LOB of Siemens Vista TnI) was prespecified.
The non-normal values distribution was verified by Kolmogorov-Smirnov test and data were finally expressed as median and interquartile range (IQR). The significance of difference between values was assessed with Mann-Whitney-Wilcoxon test. Univariate analysis was calculated using Spearman’s correlation. In multivariate linear regression analysis, the concentration of cardiac troponins (either HS-TnT or TnI) was entered as dependent variable whereas the values of other parameters with significant associations from univariate analysis were entered as independent variables. The statistical analysis was carried out using Analyse-it (Analyse-it Software Ltd, Leeds, UK). The crude odds ratio (OR) and its 95% confidence interval (95% CI) were then calculated using MedCalc version 12.3.0 (MedCalc Software, Mariakerke, Belgium). The level of statistical significance was set at P<0.05.
The study was carried out using anonymous data, in accordance with the Declaration of Helsinki and under the terms of relevant local legislation.
Results
The final study population at the University Hospital of Verona included 240 patients (median age 74 years and IQR range 64–83 years; 115 women and 125 men). The median concentration of HS-TnT was 42 ng/L (IQR, 23–66 ng/L).
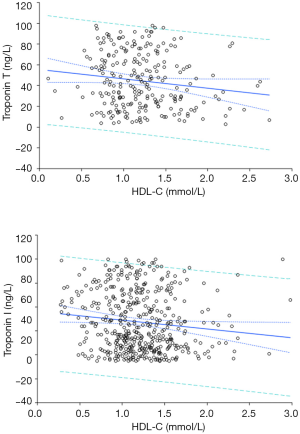
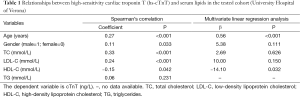
In univariate analysis, the concentration of HS-TnT was found to be significantly associated with age, sex, TC, LDL-C and HDL-C (Figure 1), but not with TG (Table 1). In multivariate linear regression analysis, in which HS-TnT concentration was entered as dependent variable and age, sex, TC, LDL-C and HDL-C were entered as independent variables, age and HDL-C were found to be significant and independent predictors of HS-TnT values, whereas no association was found with sex, TC and LDL-C (Table 1).
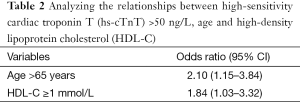
Full table
When the study population was divided according to HDL-C values (i.e., <1 or ≥1 mmol/L), subjects with HDL-C <1 mmol/L (n=61) displayed significantly higher values of HS-TnT than those with HDL-C concentration ≥1 mmol/L (n=179) (Figure 2). The frequency of HS-TnT values >50 ng/L was higher in subjects with HDL-C <1 mmol/L than in those with HDL-C ≥1 mmol/L (32/61, 52% vs. 67/179, 37%; OR, 1.84; 95% CI, 1.03–3.32; P=0.041) (Table 2). Similarly, when the study population was divided according to the age (i.e., ≤65 years and >65 years), older subjects (n=171) displayed significantly higher values of HS-TnT than those aged 65 years or younger (n=69) (Figure 2). The frequency of HS-TnT values >50 ng/L was higher in elderly subjects than in younger ones (79/171, 46% vs. 20/69, 29%; OR, 2.10; 95% CI, 1.15–3.84; P=0.015)(Table 2). Notably, the frequency of HS-TnT values >50 ng/L in elderly subjects with HDL-C values <1 mmol/L was approximately 3-fold higher than in those with of younger age and with HDL-C ≥1 mmol/L (20/35, 57% vs. 8/43, 19%; OR, 5.8; 95% CI, 2.1–16.2; P<0.001). Accordingly, the combination of age and HDL-C value explained 35% of the overall variability of TnT concentration (P<0.001).

Full table
The results of this first analysis were then replicated in a second epidemiological study carried out in the General Hospital of Verona. This study population included 463 subjects (median age 80 years and IQR range 71–87 years; 237 women and 226 men). The median concentration of TnI was 42 ng/L (IQR, 26–67 ng/L), a value that was not found to be significantly different from that of TnT (P=0.088). In univariate analysis, TnI values were found to be significantly associated with age (r=0.39; P<0.001), sex (r=−0.12; P=0.004), CT (r=0.22; P<0.001), LDL-C (r=0.31; P<0.001), HDL-C (r=−0.14; P=0.002) (Figure 1), but also with TG (r=0.09; P=0.012). However, in multivariate linear regression analysis only age (β, 0.32; P<0.001) and HDL-C (β, −7.29; P=0.010) were found to be significant predictors of TnI values. The combination of age and HDL-C value explained approximately 28% of the overall variability of TnI concentration (P<0.001).
Discussion
The role of cardiac troponins has now been firmly established for diagnosing ACS (3-5). However, emerging evidence suggests that these biomarkers, especially when assayed with HS techniques, may help predict adverse clinical outcomes (especially cardiovascular and total mortality) irrespective of the presence of baseline CVD (12). Therefore, despite the fact that the exact setting and role of cardiac troponins remain uncertain for assessing the individual risk, accumulating evidence suggests that their measurement may become more widely used in clinical practice.
A number of studies previously assessed the potential interplay between cardiac troponins and blood lipids, providing equivocal or even controversial data. Nayak et al. obtained demographic and biochemical data of 205 patients displaying increased TnT concentration at admission (13), and showed that TnT level was a significant predictor of TC (P<0.001), TG (P=0.003), LDL-C (P<0.001), but not of HDL-C (P=0.095). In a rather limited number of subjects (n=11), Ibuki et al. showed that treatment with Pitavastatin was effective to concomitantly increase HDL-C values and decrease TnT concentration, and that the relative variation of these two parameters was significantly and inversely correlated (r=−0.68; P<0.05) (14). At variance with this finding, Kumar and Sathian carried out a retrospective study including 430 patients admitted to the emergency department with suspected cardiac ischemia, who underwent both troponin and lipid profile testing (15). Patients with increased TnI values were found to have higher values of CT, LDL-C and TG than those with normal TnI, whereas the concentration of HDL-C was similar between the two study groups (39 vs. 43 mg/dL; P=0.076). More recently, McEvoy et al. measured TnT in 8,571 participants of the Atherosclerosis Risk in Communities Cohort Study (ARIC) (16), but failed to find any significant association between increased TnT concentration and high LDL-C [relative risk (RR), 0.99; 95% CI, 0.98–1.00] or high TG values (RR, 1.00; 95% CI, 0.99–1.00). Conversely, an inverse and marginally significant inverse association was reported between HDL-C values and measurable TnT concentration on follow-up (RR, 0.95; 95% CI, 0.92–0.98). In accord with these findings, Li et al. measured TnI in 2,529 consecutive patients with LDL-C <70 mg/dL and normal TnI values, who underwent elective percutaneous coronary intervention (PCI) (17). Interestingly, higher values of HDL-C were inversely associated with the risk of 5-fold post-PCI TnI increase (OR, 0.97; 95% CI, 0.95–0.99; P=0.017).
Taken together, the results of our study suggest that HDL-C values inversely predict the concentration of cardiac troponins in populations of patients admitted to inpatient clinics for routine cardiovascular risk assessment, irrespective of age, sex and other blood lipids (Figure 1), whereas no statistically significant associations were found with conventional blood lipids such as CT, LDL-C and TG in the fully adjusted multivariate linear regression analysis. Importantly, the combination of age and HDL-C value explained a considerable part of both cardiac troponins variance in blood, between 28% and 35%. This association underpins some important biologic consequences. Since cardiac troponins are significant predictors of total and cardiovascular mortality, and their concentration was found to be dependent on HDL-C values in our study, the correction of low HDL-C values by means of lifestyle changes (e.g., moderate physical activity) or pharmacologic treatment should be advocated in all patients with undesirable values (i.e., <1.0 mmol/L), regardless of their baseline cardiovascular risk. This suggestion is supported by recent evidence that even a small increase of HDL-C in patients undergoing elective coronary revascularization translates into a remarkable reduced risk of PCI-related myocardial infarction (18). The negative association observed between the values of HDL-C and those of cardiac troponins thus reinforces the well-established role of HDL-C for preventing or limiting coronary atherosclerosis and its related complications. Another important aspect emerging from our study is that the reference range and the relative URL of cardiac troponins may be different between patients with desirable or decreased HDL-C values, as well as between elderly and younger patients. It is hence reasonable to suggest conventional population-based cut-offs for diagnosing ACS using cardiac troponins should be abandoned, in favor of lower thresholds, accurately validated in well-designed clinical studies (19-20).
Conclusions
Indeed, the lack of clinical and therapeutic information should be regarded as a limitation of this study. However, the practical significance of our findings is supported by validation of the association between the values of cardiac troponins and those of HDL-C in two different hospitals and including a considerable number of patients. Moreover, irrespective of the fact that the association between HDL-C and cardiac troponins may be independent, or else mediated by additional factors such as co-morbidity or pharmacologic treatments, the interplay between these molecules underlines that consideration should be made to include cardiac troponins within the panel of biomarkers to be measured for routine cardiovascular risk assessment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective observational study was carried in accordance with the Declaration of Helsinki and under the terms of relevant local legislation.
References
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29-322. [Crossref] [PubMed]
- Li H, Ge J. Cardiovascular diseases in China: current status and future perspectives. Int J Cardiol Heart Vasc 2015;6:25-31.
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation 2012;126:2020-35. [Crossref] [PubMed]
- Casagranda I, Cavazza M, Clerico A, et al. Proposal for the use in emergency departments of cardiac troponins measured with the latest generation methods in patients with suspected acute coronary syndrome without persistent ST-segment elevation. Clin Chem Lab Med 2013;51:1727-37. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- Lippi G, Montagnana M, Aloe R, et al. Highly sensitive troponin immunoassays: navigating between the scylla and charybdis. Adv Clin Chem 2012;58:1-29. [Crossref] [PubMed]
- Ahmed AN, Blonde K, Hackam D, et al. Prognostic significance of elevated troponin in non-cardiac hospitalized patients: a systematic review and meta-analysis. Ann Med 2014;46:653-63. [Crossref] [PubMed]
- Lippi G, Cervellin G. The latest generation of troponin immunoassays: the "cholesterol" of the third millennium? J Am Coll Cardiol 2014;63:2883-4. [Crossref] [PubMed]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-421. [PubMed]
- Cardinaels EP, Mingels AM, Jacobs LH, et al. A comprehensive review of upper reference limits reported for (high-)sensitivity cardiac troponin assays: the challenges that lie ahead. Clin Chem Lab Med 2012;50:791-806. [Crossref] [PubMed]
- Arrebola MM, Lillo JA, Diez De Los Ríos MJ, et al. Analytical performance of a sensitive assay for cardiac troponin I with loci technology. Clin Biochem 2010;43:998-1002. [Crossref] [PubMed]
- Melloni C, Roe MT. Cardiac troponin and risk stratification in ischemic heart disease. N Engl J Med 2015;373:672-4. [Crossref] [PubMed]
- Nayak SB, Pinto Pereira LM, Boodoo S, et al. Association of troponin T and altered lipid profile in patients admitted with acute myocardial infarction. Arch Physiol Biochem 2010;116:21-7. [Crossref] [PubMed]
- Ibuki C, Seino Y, Otsuka T, et al. Switching to pitavastatin in statin-treated Low HDL-C patients further improves the lipid profile and attenuates minute myocardial damage. J Clin Med Res 2012;4:385-92. [PubMed]
- Kumar A, Sathian B. Correlation between lipid profile and troponin I test results in patients with chest pain in Nepal. Asian Pac J Trop Biomed 2013;3:487-91. [Crossref] [PubMed]
- McEvoy JW, Lazo M, Chen Y, et al. Patterns and determinants of temporal change in high-sensitivity cardiac troponin-T: The Atherosclerosis Risk in Communities Cohort Study. Int J Cardiol 2015;187:651-7. [Crossref] [PubMed]
- Li XL, Guo YL, Zhu CG, et al. Relationship of high-density lipoprotein cholesterol with periprocedural myocardial injury following elective percutaneous coronary intervention in patients with low-density lipoprotein cholesterol below 70 mg/dL. J Am Heart Assoc 2015;4:e001412. [Crossref] [PubMed]
- Sattler KJ, Herrmann J, Yün S, et al. High high-density lipoprotein-cholesterol reduces risk and extent of percutaneous coronary intervention-related myocardial infarction and improves long-term outcome in patients undergoing elective percutaneous coronary intervention. Eur Heart J 2009;30:1894-902. [Crossref] [PubMed]
- Lippi G. Biomarkers: Novel troponin immunoassay for early ACS rule-out. Nat Rev Cardiol 2016;13:9-10. [Crossref] [PubMed]
- Lippi G, Cervellin G. Cardiospecific troponin immunoassays: How low is it worth to go? Eur J Intern Med 2016;30:e7-8. [Crossref] [PubMed]


