
The integral theory paradigm in practice—addressing a major health crisis in bladder/bowel/pain management
The integral theory paradigm (ITP) can be summarized as:
- Control of bladder & rectum is from outside the organ, from cortically-directed muscles and ligaments.
- Pelvic symptoms and prolapse are related.
- Defective ligament collagen is the main cause of both.
- “Repair the structure and you will restore the function”.
This special series has two main aims:
- To outline the key discoveries on which the ITP is based.
- To provide a practical guide for those seeking different, effective, anatomical methods to address bladder, bowel, chronic pelvic pain problems, whether surgical, or non-surgical.
In the context of lower urinary tract symptoms (LUTS), the ITP fits Kuhn’s concept of a scientific revolution (1), in that it addresses pathogenesis and cure of many conditions hitherto considered incurable. That one billion women on the planet suffer from these LUTS conditions is the substance of a major crisis. First line treatments such as anticholinergics for overactive bladder (OAB) are hardly effective, expensive, have bothersome complications, and can cause Alzheimer’s disease. Opioid treatments for chronic pelvic pain can lead to lifetime addictions.
The only bladder condition considered reliably curable is stress urinary incontinence (SUI) whose gold standard operation, the midurethral sling, is based on the ITP (2). Yet, a solution for other bladder, chronic pain and anorectal problems, also based on the ITP, is in plain sight. Even a cursory review of this special ITP series will show that significant anatomical solutions to the aforementioned crisis, based on the ITP are available, some since 25 years (Figure 1).
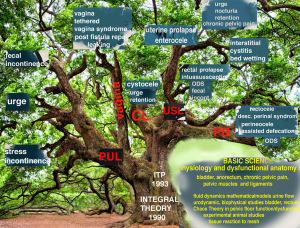
These discoveries, pictorially summarized in Figure 1, were the product of extensive collaboration over more than 25 years between many colleagues who followed the ITP, communicated closely, shared data, techniques, experiences and wrote many papers. Many of their outstanding contributions are showcased in this series.
The core to the many different discoveries was the demonstration in 1990 (2), that control of the bladder (and later the anorectum) was not from the organ itself, but from outside it, from pelvic muscles and ligaments; furthermore, LUTS dysfunctions were mainly caused by collagen defects in these ligaments, and that LUTS could be cured by repairing the ligaments. The url for the 1990 Integral Theory publication for the bladder, is https://obgyn.onlinelibrary.wiley.com/toc/16000412/1990/69/S153, and for the bowel, https://www.researchgate.net/publication/267778578_The_MusculoElastic_Theory_of_anorectal_function_and_dysfunction. By permission Pelviperineology.
How this series is structured
The aim is to present short, penetrating insights into the anatomical basis of bladder, bowel, chronic pelvic pain, prolapse dysfunctions, augmented by short explanatory videos. At the same time, the 19 papers in this series provide a practical guide for anatomically-based pathogenesis and treatment, diagnosis and treatment of the conditions in Figure 1.
A paradigm
According to Kuhn (1), “the history of science is characterized by revolutions in scientific outlook. Scientists have a worldview or ‘paradigm’. A paradigm is a universally recognizable scientific achievement that, for a time, provides model problems and solutions to a community of practitioners.”
Theories
There are two major theories for pelvic floor dysfunction. The universal theory of Swash et al. [1985] (3) state bladder/bowel dysfunctions are due to birth-induced nerve damage to muscles. Such dysfunction may improve with time but are not otherwise curable. The second is the Integral Theory which states pelvic muscles contracting against ligaments control opening and closure of bladder and the anorectum, and that damaged collagen in ligaments is the main cause of bladder/bowel/pain/prolapse dysfunctions, which can be improved or cured by collagenopoietic surgical techniques.
Definitions followed are by the International Continence Society (ICS) (4).
Acknowledgments
I would like to acknowledge the efforts of the many colleagues globally, and in particular, the authors of this special series of the Annals of Translational Medicine, who have significantly expanded the original vision of the Integral Theory into a holistic paradigm which has crossed the borders of urology, gynecology, coloproctology, pain, geriatric and pediatric disciplines.
I would like to thank Ms Vani Bardetta BA, MA (Assistant Guest Editor), for her seminal assistance with the powerpoint videos, and for her rigorous review of every aspect of the text of each paper for this special series. The final acknowledgement is to Anne Lu and her excellent team at the Annals of Translational Medicine. Over a period of almost two years, they impressively co-ordinated the difficult logistics of 20 papers from 45 authors to the highest standards, in the most professional and efficient way.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1755/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. P.P. served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Translational Medicine from October 2022 to September 2024. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kuhn T. The structure of scientific revolutions. Chicago: University of Chicago Press; 1970.
- Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 1990;153:7-31. [Crossref] [PubMed]
- Swash M, Snooks SJ, Henry MM. Unifying concept of pelvic floor disorders and incontinence. J R Soc Med 1985;78:906-11. [Crossref] [PubMed]
- Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:167-78. [Crossref] [PubMed]


