
Pubourethral and uterosacral male analogues suggest parallel male/female pelvic anatomy and symptom pathogenesis
Highlight box
Key findings
• A puboprostatic ligament (PPL) restoration by retropubic minisling cured stress urinary incontinence, as does pubourethral ligament repair in the female. The prostatosacral ligament (PSL) is analogous to the uterosacral ligament.
What is known, and what is new?
• Little is known about pathogenesis of male incontinence and “chronic prostatitis” (CP).
• The role of three reflex pelvic muscle movements and PPLs in male continence.
What is the implication, and what should change now?
• PPL should be preserved during radical prostatectomy.
• Preserve PPL during prostatectomy. Explore the role of PSL in “CP”.
Introduction
The key points of the article are summarized in the video abstract (Video S1).
The thesis for parallel male/female pelvic anatomy rests on cure of post-prostatectomy stress urinary incontinence (SUI) by retropubic minisling repair of the puboprostatic ligament (PPL) (1) and the discovery of a uterosacral male analogue during laparoscopic surgery for rectal carcinoma (2).
The hypothesis which led to the male retropubic sling operation (1) was the question, “Does post-prostatectomy SUI have the same pathogenesis as SUI in the female, i.e., a weak or damaged PPL?”.
Important follow-up questions were:
- Does the male have the same three reflex directional forces acting around the PPL on straining, as in the female?
- Does the PPL have the same anchoring role for pelvic muscle contraction as does the pubourethral ligament (PUL) in the female?
- Does digital support of PPL, via a rectal examination, control urine loss on coughing like vaginal PUL support in the female?
- Would the same minisling methodology which the authors (1) used for cure of SUI in the female, also cure post-prostatectomy incontinence in the male?
The aim of this work is to test the hypothesis of parallel anatomy.
Evidence for parallel anatomy
The evidence for parallel anatomy is detailed below.
Transperineal ultrasound
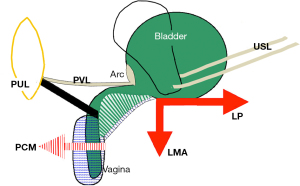
Transperineal ultrasound examinations were performed to confirm reflex directional closure vectors around the PPL. Though the patient had SUI, the same three directional forces seen during closure in the female (Figure 1), were present in the male: backward/downward movements of the proximal urethra, forwards and upwards in the distal urethra (Figure 2).

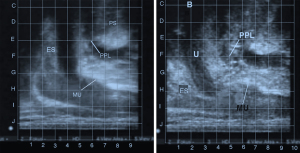
Digital support for the PPL
Digital support for the PPL rectally by pressing an index finger against the posterior wall of the symphysis controlled urine loss on coughing. Control of SUI by mechanical support of a weak PPL is similar in concept to mechanical control of PUL in the female (Figure 1 and Video S2).
Parallel backward/downward movements on straining
The downward/backward vector forces which open the bladder neck in a woman with SUI (Figure 1, middle frame) is known to contract down against the uterosacral ligament (USL) (3). The identical downward/backward vector forces noted during straining in Figure 2, also require a firm superior anchoring point. We believe this to be the PS ligament, the male USL analogue (2).
Cadaveric testing of a male midurethral sling
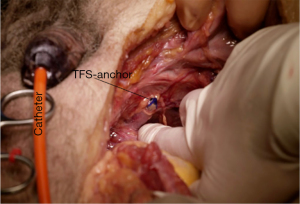
A tissue fixation system (TFS) minisling inserted perineally as in the method described for females treated with the TFS minisling, was found to penetrate the PPL (Figure 3).
The pubovesical ligament (PVL)
PVL attaches to the arc of Gilvernet to anchor the anterior wall of the bladder during straining and micturition in both males and females (Figures 4,5). The role of PVL and arc, in both male and female, is to prevent collapse of the anterior bladder wall when the backward/downward rotating forces act to close the bladder neck or open it for micturition. The three directional movements act around PPL (Figure 4) as they do around PUL (Figure 2).

Surgical validation of PUL/PPL parallel anatomy
A key validation of the parallel anatomical hypothesis was the successful surgical treatment of 22 males with post-prostatectomy stress incontinence by TFS minisling of the PPL (1) (Tables 1,2). A 7-mm TFS sling was inserted between the bladder neck and perineal membrane to reinforce the PPL (Figure 3), which gave high success rates, when reviewed at 9 months post-operatively (1) (Tables 1,2). The mean pre-operative urine (pad) loss was 3.8 pads at 9 months; the mean post-operative loss was 0.7 pads; 13/22 (59.1%) patients were 100% improved; 7/22 (31.8%) improved >50% but <100%; 2/22 (9.1%) improved ≤50%.
Table 1
| Patient | Name (initials) | Pre (pad) | Post (pad) | Difference | Improvement (%) |
|---|---|---|---|---|---|
| 1 | SM | 1 | 0 | 1 | 100.0 |
| 2 | CR | 1 | 0 | 1 | 100.0 |
| 3 | DB | 2 | 0 | 2 | 100.0 |
| 4 | BW | 6 | 2 | 4 | 66.7 |
| 5 | PM | 6 | 2 | 4 | 66.7 |
| 6 | WB | 4 | 1 | 3 | 75.0 |
| 7 | CP | 4 | 0 | 4 | 100.0 |
| 8 | BL | 4 | 0 | 4 | 100.0 |
| 9 | HL | 4 | 0 | 4 | 100.0 |
| 10 | WD | 4 | 1 | 3 | 75.0 |
| 11 | SP | 4 | 2 | 2 | 50.0 |
| 12 | SK | 4 | 0 | 4 | 100.0 |
| 13 | KR | 4 | 0 | 4 | 100.0 |
| 14 | RM | 4 | 0 | 4 | 100.0 |
| 15 | WM | 3 | 0 | 3 | 100.0 |
| 16 | EH | 3 | 1 | 2 | 66.7 |
| 17 | BB | 3 | 1 | 2 | 66.7 |
| 18 | HP | 3 | 0 | 3 | 100.0 |
| 19 | PW | 3 | 0 | 3 | 100.0 |
| 20 | LW | 3 | 0 | 3 | 100.0 |
| 21 | AS | 7 | 2 | 5 | 71.4 |
| 22 | CS | 6 | 3 | 3 | 50.0 |
| Mean | 3.8 | 0.7 | 3.1 | – | |
| Median | 4.0 | 0.0 | 3.0 | – |
Reused from (1). Copyright 2022, with permission from Karger. TFS, tissue fixation system; pre, pre-operative; post, post-operative.
Table 2
| Improvement | N | % |
|---|---|---|
| 100% | 13 | 59.1 |
| >50% but <100% | 7 | 31.8 |
| ≤50% | 2 | 9.1 |
Reused from (1). Copyright 2022, with permission from Karger.
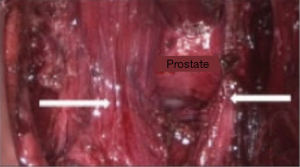
Discovery of a USL male analogue
The discovery of a USL male analogue was a consequence of the necessity to find a structure for the downward/backward vectors, demonstrated in Figure 2, to contract against. It was hypothesized that there had to be a male USL analogue. Professor Farag, described his discovery of a male USL analogue during laparoscopic surgery for rectal carcinoma as follows (2): “In the present work, we describe a new ligament in the male which has the same anatomical pathway as in the female anatomy. The male prostatosacral (PS) ligament has its origin from the back of the prostate where it passes posteriorly on both sides of the rectum before gaining its posterior attachment. The group included 27 males and 19 females, age range 31–72 years, mean 34 years. In 25 out of the 27 patients studied (92.6%), the prostatosacral ligament (PSL) originated on both sides of the median sulcus of the prostate (Figure 6) (2). In the remaining 2 male patients (7.4%), it originated from the conjoined ischio-pubic ramus without obvious attachment to the prostate. In all 27 male patients, and in all the female patients, the ligament passes lateral to the rectum being fused with the lateral margin of the mesorectum before leaving it as it thins out to be attached.”.
Parallel backward/downward straining movements require firm posterior ligament anchoring
The downward/backward vector forces which open the bladder neck in a woman with SUI (Figure 1, middle frame) is known to contract down against the USL (3). The identical downward/backward vector forces noted during straining in Figure 2, also require a firm superior anchoring point. We believe this to be the PS ligament, the male USL analogue (2), posteriorly, similar to the USL.
PSL anatomy and histology
The PSL is not, to our knowledge, described elsewhere in the literature. Nevertheless, PSL anatomy (Figure 6) was analogous to USL in the female. The histology is very similar to that of the female USL: collagen, elastin, smooth muscle, abundant blood vessels and nerves. Professor Farag also identified male pelvic visceral plexuses in an analogous position to those of the female.
Is chronic prostatitis (CP) a male analogue of the posterior fornix syndrome (PFS)?
The discovery of a male USL analogue (2) raised the question, “Is the posterior fornix syndrome a parallel condition with “chronic prostatitis?” (2). The “CP” syndrome is characterized by pelvic pain, voiding symptoms, and additional phenotypic signs that are still poorly defined (4).
Table 3 indicates that the symptoms of CP are very similar to those of PFS, with pain the predominant symptom (4). Our hypothesis is that the prostate is the analogue of the cervix, and that the male USL analogue discovered (2), has similar dysfunctions in the female as detailed in Table 3. Our hypothesis of parallel s for CP and PFS predicts that other posterior zone symptoms, such as obstructive defecation and fecal incontinence, would also be present in some CP patients.
Table 3
| CP | PFS |
|---|---|
| Pain constant or variable | Pain constant or variable |
| Frequency | Frequency |
| Urgency | Urgency |
| Nocturia | Nocturia |
| Perineal pain | Perineal pain |
| Pain in testicles/scrotum | Pain in vagina/vulva |
| Pain ejaculating | Dyspareunia |
| Low abdominal pain |
CP, chronic prostatitis; PFS, posterior fornix syndrome.
Conclusions
Other than for the pelvic organs, male and female anatomy are virtually identical. Genetic and hormonal influences have changed the morphology and function of the pelvic organs. We have presented evidence that the functional anatomy of the bladder and some ligaments are similar, if not parallel. The symptom similarities in Table 3 are suggestive that CP could be a male phenotype of the PFS. However, for now, this part of parallel male/female dysfunction remains only a hypothesis which needs to be objectively tested.
Acknowledgments
We would like to express our thanks to Vani Bardetta for her proofreading and administrative services for this article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1888/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1888/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. P.P. serves as an unpaid editorial board member of Annals of Translational Medicine from October 2022 to September 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images. Human participation in the video was by patient permission on the basis it was deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Muctar S, Ende D, Petros P. Retropubic TFS Minisling for Postprostatectomy Male Incontinence: First Report. Urol Int 2022;106:249-55. [Crossref] [PubMed]
- Farag A, Nasr SE, Elbarmelgi MY, et al. Prostato-sacral Ligament, description of a new anatomy in males, its clinical significance and anatomic similarity to female anatomy. Pelviperineology 2019;38:115-7.
- Petros PE, Ulmsten U. The posterior fornix syndrome: a multiple symptom complex of pelvic pain and abnormal urinary symptoms deriving from laxity in the posterior fornix. Scand J Urol Nephrol 1993;27:89-93.
- Wagenlehner FM, van Till JW, Magri V, et al. National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) symptom evaluation in multinational cohorts of patients with chronic prostatitis/chronic pelvic pain syndrome. Eur Urol 2013;63:953-9. [Crossref] [PubMed]


