
A comparison of native vaginal and ligament surgery for cure of pelvic organ prolapse and overactive bladder
Highlight box
Key findings
• Native ligament surgery gives good cure rates for pelvic organ prolapse (POP) and overactive bladder (OAB) pre-menopausally, but low cure rates post-menopausally.
What is known and what is new?
• Vaginal surgery has poor results for POP repair.
• Ligament surgery gives good cure rates for OAB and POP, but only in premenopausal women, not postmenopausal women.
What is the implication, and what should change now?
• In postmenopausal women, collagen-creating methods are needed to structurally reinforce weakened ligaments for POP repair.
Introduction
The key points of the article are summarized in the video abstract (Video S1).
“Ligaments are for structure, vagina for function”. Integral Theory (1).
The incidence of pelvic organ prolapse (POP) and overactive bladder (OAB) (frequency, urge, nocturia) is increasing, parallel with the ageing of the population, more especially in Japan (2). Worldwide, about 40% of women will experience POP, and this proportion is expected to increase with the aging of the population (3). As regards surgery, in 2008, the lifetime risk for an 80-year-old woman undergoing at least one POP surgery in Denmark was 18.7% (4). Traditionally, native anterior and posterior repair of the vagina have been applied to repair prolapse, but cure rates remain dismally low. In contrast, high cure rates for POP and OAB (urge frequency nocturia) have been reported using collagen-creating sling (5) techniques to repair the uterosacral ligaments (USLs) (6-12), analogous to midurethral sling (MUS) surgery.
However, more recently, these posterior sling operations have been placed in the same category as mesh sheets. They are banned by regulatory bodies in many western countries, and in some, the MUS also. In such countries, native tissue repair remained the only available option for women who have prolapse.
Results from studies
We compare native vaginal tissue repair (12), native ligament (13) and site-specific ligament repair with collagen-producing mesh tapes (10,14).
Native vaginal repair
In 2017, the Lancet Prospect Trial assessed 430 women mean age 59 years, who had mainly standard vaginal repair for “POP” (12); 78 had co-occurring urinary incontinence (12). The failure rate for native tissue vaginal repair of the prolapse 6 months after surgery was 79% (12).
Native cardinal/uterosacral ligament (CL/USL) repair
In 2021, Shkarupa et al. studied the effect of native tissue CL/USL repair on POP and “OAB” (frequency, urgency, nocturia) and POP (Table 1) (13). An important inclusion criterion was decrease of urge symptoms following insertion of a roll gauze tampon in the posterior fornix of the vagina (“simulated operation”) (13). The importance of this preoperative test was that it linked the urge symptom to the USLs. Exclusion criteria were stress urinary incontinence (SUI), and POP grades 3–4. The surgery consisted of plication of cardinal and USLs.
Table 1
| POP/OAB symptoms | Pre-menopausal group (n=49) (%) | Post-menopausal group (n=39) (%) |
|---|---|---|
| 3 months | ||
| Frequency | 71.5 | 64.1 |
| Urgency | 85.7 | 82 |
| Nocturia | 96 | 64.1 |
| POP | 98 | 89.7 |
| 6 months | ||
| Frequency | 77.5 | 48.7 |
| Urgency | 85.7 | 64.1 |
| Nocturia | 98 | 59 |
| POP | 85.7 | 48.7 |
| 12 months | ||
| Frequency | 63.3 | 38.5 |
| Urgency | 81.6 | 33.3 |
| Nocturia | 71.5 | 25.6 |
| POP | 85.7 | 20.5 |
| 18 months | ||
| Frequency | 59.2 | 15.4 |
| Urgency | 67.3 | 17.9 |
| Nocturia | 87.7 | 20.5 |
| POP | 79.6 | 15.4 |
Reused from (13). Copyright 2021, with permission from Central European Journal of Urology. POP, pelvic organ prolapse; OAB, overactive bladder.
Prolapse was assessed by the Baden-Walker classification, and OAB by the Urinary Distress Inventory Short Form 6 (UDI-6), Overactive Bladder Questionnaire (OAB-q), Pelvic Floor Impact Questionnaire-Short Form 7 (PFIQ-7), and International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-SF) questionnaires and voiding diary. Postoperative assessment was performed at 3, 6, 12 and 18 months after surgery. There was a marked difference between the premenopausal and postmenopausal women for POP, and all the OAB symptoms, urge, frequency, nocturia (Table 1) (13).
Ligament repair alone was sufficient for cure of POP and urgency in premenopausal women, achieving cure rates of 85.7% for POP and 81.6% for urgency at 12 months. For postmenopausal women, at 12 months, the cure rate for POP was 20% and for urge 33% (Table 1) (13).
With reference to the excellent results for premenopausal women at 18 months (Table 1), the authors (13) raised the questions, “What happens after the menopause? Would collagen breakdown cause POP and OAB?” (13). Their recommendation to use collagen creating tapes for women with significant prolapse and OAB, was based on their unit’s experience (6). More comprehensive details are available in Shkarupa et al.’s paper (13).
POP repair using collagen-creating slings
A dramatic difference between native ligament repair and collagen-creating slings in post-menopausal women was demonstrated by long-term data from Japan; Inoue et al.’s 5-year data for POP and lower urinary tract symptoms (LUTS) (12) in 70-year-old Japanese women was: 91.2% for POP, 96.8% for urge at 12 months, falling to 79.0% for POP and 91.7% for urge at 60 months (11). Further validation was provided by this group’s 10-year data, 960 women with 3,100 implants (10).
Ligaments are the main structural support of the pelvic organs, while the vagina’s principal role is to transmit the pelvic muscle forces which open and close the urethra and prevent premature bladder emptying (urge incontinence) (1). Native CL/USL ligament repairs work well for premenopausal women, but not for postmenopausal women (12,13). The experience of many authors (7-13) and, in particular, the 10-year experience of Inoue et al., 3,100 tape implants in 960 70-year-old women with 3rd and 4th degree POP with no vaginal excision, indicates that collagen creation methods will be required for good POP surgery results, at least in postmenopausal women (10). Hand-cut artisan tapes can be used with individual patients where commercial kits are banned (14). An emerging technique, plication of ligaments with wide-bore polyester sutures (15), already shows great promise. If longer-term results are satisfactory, it could become an available low-cost solution for countries where all mesh products are banned for vaginal surgery. This method has already been applied to repair pubourethral ligaments for SUI (15), cardinal and USLs for prolapse and OAB symptoms, and also, deep transversus perinei ligaments for cure of descending perineal syndrome and urge fecal incontinence, as described elsewhere in this special series.
Discussion
Hitherto, the relationship between age and higher incidence of OAB and POP after the menopause was known but was never clearly defined. Shkarupa et al.’s trial (Table 1) very clearly delineated that the menopause is a defining point as regards prospects for surgical cure for both POP and OAB symptoms, and, therefore, the decision for surgery (13).
A very important part of Shkarupa et al.’s study (13) was the direct linking of USL weakness and urge by only operating on women who were screened by a preoperative test: reduction of urge by placement of a roll gauze in the vaginal fornix to mechanically support USLs. Cure of OAB by CL/USL repair provides the first experimental evidence of a direct link between USL laxity and OAB (13).
One important difference between the Lancet Prospect vaginal repair Trial (12) and the ligament repair trial (13), was the different strengths of the tissues which were repaired: ligaments have a breaking strain 300 mg/mm2 and the vagina, 60 mg/mm2 (16). Shkarupa et al. repaired the CL/USL with no vaginal excision. Ligaments are the structural components of the pelvic floor, while the vagina is concerned with function, transmitting the muscle forces which open and close the urethra (1). The structural collagen 1 in ligaments is much stronger than the collagen 3 and elastin of the vagina which provide its elasticity.
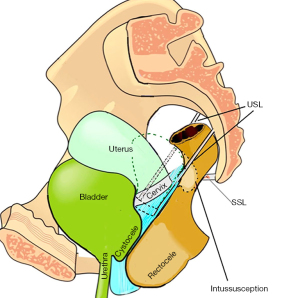
We can deduce from basic biomechanical principles, that, in order to preserve its elastic function, the vagina should be conserved, not excised. Furthermore, collagen deficient ligaments in the menopause need new collagen to be created, so as to prevent the USL ligament elongation which results in organ prolapse and even anterior rectal wall intussusception (Figure 1), and to retain their structural function. It is evident on inspecting Figure 1, that the organs are suspended by ligaments. Excising and suturing the vagina, a weak structure, cannot by itself cure either a cystocele, or a uterine prolapse, as proven by the Lancet Prospect Trial (12). Notwithstanding adherence to these surgical principles (13), the poor results in the menopausal group (Table 1), can be reasonably explained by collagen breakdown after the menopause and excretion as hydroxyproline throughout the menopausal period (17).
Conclusions
The key message from Shkarupa et al.’s CL/USL study was that in premenopausal women, ligament repair alone provides good cure rates for POP, and urgency at 12 months. However, catastrophically low cure rates were noted for both conditions in post-menopausal women. Shkarupa et al. advised that post-menopausal women required collagen-creating slings. These comments were validated by Inoue et al. Using the collagen-creating Tissue Fixation System (TFS) minisling, high 5- and 10-year surgical results for POP and urge were reported in 70-year-old Japanese women (2,11). The final question by Shkarupa et al. was “What happens to the successful POP and urge group results after the menopause?”. However, this raises another significant question, “Should collagen-creating methods be used routinely for women with POP and LUTS?”.
Acknowledgments
We would like to express our gratitude to Editors Professor Peter Petros and Vani Bardetta for their exceptional support in the design and refinement of the article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1781/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1781/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 1990;153:7-31. [Crossref] [PubMed]
- Inoue H, Nakamura R, Sekiguchi Y, et al. Tissue Fixation System ligament repair cures major pelvic organ prolapse in ageing women with minimal complications - a 10-year Japanese experience in 960 women. Cent European J Urol 2021;74:552-62. [PubMed]
- Wang B, Chen Y, Zhu X, et al. Global burden and trends of pelvic organ prolapse associated with aging women: An observational trend study from 1990 to 2019. Front Public Health 2022;10:975829. [Crossref] [PubMed]
- Løwenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J 2015;26:49-55. [Crossref] [PubMed]
- Petros PE, Ulmsten UI, Papadimitriou J. The autogenic ligament procedure: a technique for planned formation of an artificial neo-ligament. Acta Obstet Gynecol Scand Suppl 1990;153:43-51. [Crossref] [PubMed]
- Shkarupa D, Kubin N, Pisarev A, et al. The hybrid technique of pelvic organ prolapse treatment: apical sling and subfascial colporrhaphy. Int Urogynecol J 2017;28:1407-13. [Crossref] [PubMed]
- Liedl B, Inoue H, Sekiguchi Y, et al. Is overactive bladder in the female surgically curable by ligament repair? Cent European J Urol 2017;70:53-9. [PubMed]
- Petros P, Abendstein B, Swash M. Retention of urine in women is alleviated by uterosacral ligament repair: implications for Fowler's syndrome. Cent European J Urol 2018;71:436-43. [PubMed]
- Caliskan A, Ozeren M, Goeschen K. Modified posterior intravaginal slingplasty: does the additional bilateral tape attachment to the sacrospinous ligament improve the results? Cent European J Urol 2018;71:326-33. [PubMed]
- Inoue H, Kohata Y, Sekiguchi Y, et al. The TFS minisling restores major pelvic organ prolapse and symptoms in aged Japanese women by repairing damaged suspensory ligaments - 12-48 month data. Pelviperineology 2015;34:79-83.
- Inoue H, Kohata Y, Fukuda T, et al. Repair of damaged ligaments with tissue fixation system minisling is sufficient to cure major prolapse in all three compartments: 5-year data. J Obstet Gynaecol Res 2017;43:1570-7. [Crossref] [PubMed]
- Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet 2017;389:381-92. [Crossref] [PubMed]
- Shkarupa D, Zaytseva A, Kubin N, et al. Native tissue repair of cardinal/uterosacral ligaments cures overactive bladder and prolapse, but only in pre-menopausal women. Cent European J Urol 2021;74:372-8. [PubMed]
- Piñango-Luna S, Level-Córdova L, Petros PE, et al. A low cost artisan tension-free tape technique cures pelvic organ prolapse and stress urinary incontinence - proof of concept. Cent European J Urol 2020;73:490-7. [PubMed]
- Petros P, Palma P. Conceptualizing stress urinary incontinence surgery beyond midurethral slings: Very early results from simplified ligament repair without tapes. Neurourol Urodyn 2023;42:383-8. [Crossref] [PubMed]
- Yamada H. Aging rate for the strength of human organs and tissues. In: Evans FG, editor. Strength of biological materials. Baltimore: Williams & Wilkins Co; 1970:272-80.
- Sone T, Miyake M, Takeda N, et al. Urinary excretion of type I collagen crosslinked N-telopeptides in healthy Japanese adults: age- and sex-related changes and reference limits. Bone 1995;17:335-9. [Crossref] [PubMed]


