
Further developments of pubourethral ligament surgery for stress urinary incontinence
Highlight box
Key findings
• Strengthening pubourethral ligament (PUL) is required for cure of stress urinary incontinence (SUI).
What is known, and what is new?
• Cure of SUI at present is by midurethral slings (MUS).
• New directions are: an artisan single incision minisling and PUL plication with wide-bore sutures without need for a tape.
What is the implication, and what should change now?
• Two low-cost simple operations for SUI are presented and these could be performed now.
• These methods can be adopted now in countries, with few resources, as well as in countries such as the United Kingdom where MUS are banned.
Introduction
The key points of the article are summarized in the visual abstract (Video S1).
“Precise, almost mathematical knowledge of anatomy is a highly fertile source of surgical applications, suggesting new techniques and helping perfect and simplify existing surgical methods, making them less mutilating and more benign and, in short, raising surgery to the rank of true science.”
What is it for? Salvador Gil Vernet [1892–1987], famous Spanish anatomist/surgeon.
“Repair the structure and you will restore the function”—Integral Theory.
The counsel from Salvador Gil Vernet is more than “Repair the structure”. The surgeon must ask “what is it for?” and understand the function of each anatomical component which he/she is going to operate on. Otherwise, there can be no improvement in any surgical technique or outcome. All the daycare stress urinary incontinence (SUI) operations described in this special series of Annals of Translational Medicine evolved from three basic science discoveries in the 1990 Integral Theory (1-3) available free online at: https://obgyn.onlinelibrary.wiley.com/toc/16000412/1990/69/S153.
- Three opposite reflex forces contract against firm pubourethral ligaments (PULs) and uterosacral ligaments (USLs) to close or open the urethra and to stretch the vagina like a trampoline to prevent the urothelial stretch receptors from activating micturition at low bladder volumes (urgency).
- Collagen deficiency was the main source of weak ligaments.
- A new surgical method, harnessing the collagenopoietic foreign body reaction to implanted material could create new collagen to repair weak ligaments for cure of SUI, pelvic symptoms and prolapse.
A short history
Evolution of daycare surgery for cure of SUI began with the prototype midurethral sling (MUS) in 1988 at the Royal Perth Hospital (1). Investigation of anomalous data led to the 1990 Integral Theory (2). Parallel with the discoveries of bladder function, dysfunction and control, a new surgical principle was described in 1990 (2). It used an implanted tape to create a collagenous pubourethral ligament (PUL) (3). By 1996, the prototype procedures had become the tension-free vaginal tape (TVT). By 2008, an estimated 10 million operations had been performed worldwide (4).
Pathogenesis of SUI
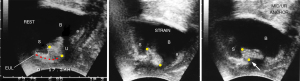
With reference to Figure 1, a loose or weakened PUL, lengthens on effort (middle frame). Figure 2 shows how a weak PUL is elongated to “L”. The weakened PULs cannot structurally support the midurethra. The posterior vector forces, the levator plate/conjoint longitudinal muscle of the anus (LP/LMA) contracting against USLs, forcibly pull open the posterior wall of the urethra from “C” (closed) to “O” (open). Application of a hemostat as shown in Figure 2 restores anatomy and continence: the urine does not run out on coughing (2).
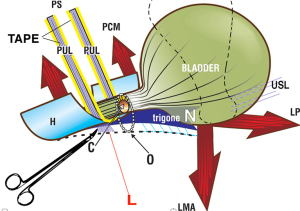
What this means is that any method which limits elongation of PUL, be it a hemostat, a sling, or PUL plication without any tapes should cure SUI.
The MUS operation
The inspiration for the MUS (Figure 2), was that urine loss was controlled by applying a unilateral hemostat vaginally (Figure 1, right frame, white arrow) (Video S2), in the exact position of the PUL as shown in Video S3. However, in the second part of Video S3, a fold of the suburethral vagina (“H”) (Figure 2), was required for total continence. The fold allowed the two pubococcygeus muscle (PCM) muscles to apply “H” more closely against the posterior urethral wall to close the distal urethra (Figure 2).
The MUS (Figure 2), as originally performed retorpubically, limits descent of the PUL, and cures SUI by restoring the bladder neck and distal closure. The MUS was first performed in prototype form in 1988 at Royal Perth Hospital, Perth, Western Australia (1). An insertion instrument (tunneller), placed a tape in the exact position of the PUL, as in Figure 2. This operation was commercialized in the late 1990s, as the “TVT”, using a different application system. In the first few years of the TVT, these insertion instruments caused many serious complications, such as nerve, vascular, urethral and intestinal perforations, with as many as 20 deaths reported.
Evolutions from the retropubic operation
In 2001, the transobturator tape (TOT) operation developed by Emmanuel Delorme (6) solved many of these problems, but became associated with bothersome hip pain. In 2005, data from the first single incision minisling was published (7) (see Video S4); it avoided most of the TVT and TOT complications, and gave equivalent cure rates for SUI at 5 years (8) and 90% for intrinsic sphincter defect (ISD) at 12 months (5). In 2020, Pinango-Luna et al. developed the single incision tension-free artisan retropubic MUS sling (9), and in 2023, Uysal et al. published longer-term data for the artisan TOT MUS sling (10). All these methods used a suburethral tape, and were subject to possible retention from such tapes, albeit with different incidence. The latest evolution of the day surgery journey is direct repair of PULs using wide-bore collagen-creating polyester sutures for cure of SUI without tapes (11).
Important points of technique for MUS operation
- Avoiding nerve and major vessel complications with a standard retropubic MUS operation. Make a tunnel toward the right or left shoulder. Perforate the perineal membrane to a depth of 1.5 cm. Insert the tip of the tunneller until it is just behind the symphysis. Immediately turn the instrument so it is vertical. Proceed gently to insert both tapes. If there is bleeding, apply digital pressure, repeatedly, until the bleeding stops.
- Avoiding post-operative urinary retention with any MUS. Inspection of the middle frame of the ultrasound Figure 1, and also, Figure 2, shows the cause of SUI is elongation of PUL on effort. The tape works by preventing the elongation “L” (Figure 2). It is essential that a No. 18 Foley catheter or No. 8 Hegar dilator be kept at all times in the urethra while the tape is being “set”, as a built-in safety measure to prevent the tape compressing the soft urethral tissue.
The non-stretch tape (advisable) is pulled up until it sits on the posterior urethral wall but does not compress it. If the surgeon over-elevates the tape, there is a high chance of narrowing the urethra and causing retention post-operatively. Even a 1 mm overextension may cause post-operative urinary retention because the resistance to flow is exponentially determined, by the 4th power of the radius (Poiseuille’s Law).
A non-stretch tape is advisable as an elastic tape extends when pulled up. In the ensuing few hours, the elastic tape restores its shape and may compress the urethra to cause urinary retention. To counteract this, scissors need to be interposed between tape and urethra and a No. 18 Foley catheter or No. 8 Hegar dilator be kept at all times in the urethra while the tape is being “set”.
If retention continues beyond 48–72 hours, it is advisable for the patient to be returned to the operating room (OR) and the tape loosened, a relatively simple operation, as scar tissue from the tape has not yet formed.
Artisan single incision tension-free minisling tapes—a low-cost method for SUI
Even in countries where the MUS kits are banned, every surgeon has the right, on consultation with the patient, to offer her an artisan MUS (9). With reference to Figure 2, a 1 cm × 10 cm strip is cut from a non-stretch mesh sheet to form an artisan tape. A standard MUS vaginal incision is made at the midurethra. Metzenbaum scissors create a tunnel, taking care to penetrate the perineal membrane. The tip of the tape is grasped by forceps (e.g., Crile) and inserted so the tape fits comfortably touching the urethra. It is important that no space be left between the tape and urethra and that a No. 18 Foley catheter be always in place during tape insertion. Occasional bleeding from injury to the venous system when encountered is controlled by digital compression of the vaginal wall against the pubis until the bleeding stops.
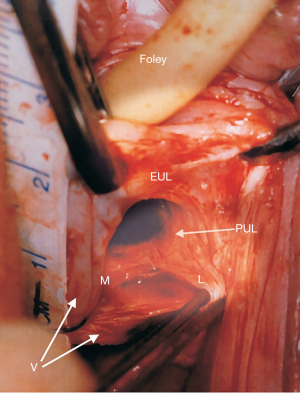
The suburethral vagina is then reconstituted. With Foley catheter in situ, the midline incision is extended to within 0.5 cm of the external meatus; the external urethral ligament (EUL) is located just lateral to the meatus and penetrated by a 00 Vicryl suture (Ethicon) which is then inserted as a continuous suture, into the right and left vaginal fascia finishing with the contralateral EUL. The vaginal wall is closed with interrupted, delayed absorption sutures (Video S5).
Recently presented data from 93 women using an artisan TOT (10). The cure rate was at mean 5.7 years, was 91.3%. Late complications included mesh erosion in four patients (4.3%) and complaints of urgency in six patients (6.4%). No patient had voiding dysfunction needing self-catheterization. The TOT artisan technique performed by Uysal et al. was as follows (10):
“A full-thickness suburethral incision starting 1 cm inferior to the external urethral meatus and approximately 1.5–2 cm in length was made. The paraurethral areas were then opened by sharp dissection. Subfascial dissection was carried out towards the posterior faces of the inferior rami of the ischiopubic bone until the obturator internus muscle was reached. A surgeon-tailored length of monofilament polypropylene mesh, 10 cm × 0.8 cm wide was grasped in the jaws of a Kelly clamp a few millimeters from the tips. The clamp was inserted into the previously dissected paraurethral space until the pop, signifying penetration of the internal obturator fascia, was felt. The clamp was advanced a few millimeters into the obturator internus muscle and then opened to release the mesh tape. The same manoeuvre was performed on the opposite side. After ensuring that the space between the mesh and the urethra was no greater than 3 mm (by inserting Metzenbaum scissors between the mesh and urethra), the pubocervical fascia was secured over the mesh with 2/0 polyglactin (Vicryl®) suture. Afterward, the suburethral incision was sutured intermittently with 2/0 polyglactin (Vicryl®) suture”.
Urethral ligament plication (ULP) procedure
The ULP is another new low-cost operation for cure of SUI. It is different in concept from the MUS operation. The MUS uses a precisely inserted tape to create an artificial collagenous PUL (pubourethral) neoligament. In contrast, the ULP operation adds new collagen to collagen-deficient PULs by harnessing the wound reaction of wide-bore No. 2 or No. 3 polyester sutures (Figure 3) (11). No tapes are required. Video S6 describes the ULP technique in principle and Video S7 describes the actual ULP technique as performed by Professor Sivaslioglu. The ULP technique (Video S7): full thickness vaginal incisions are made in the periurethral sulci extending from the bladder neck to the urethral meatus. Local anesthetic (LA) infiltration of the sulcus assists access to a deep sulcus. The incision is opened with dissecting scissors to reveal descending and midurethral branches of the PUL (Figures 3,4).
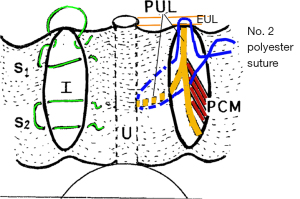
The operation was performed in a space of approximately 2.5 cm2 (Videos S6,S7). A No. 2 or No. 3 polyester suture is inserted into the urethral part of PUL, then the pubic part of the PUL, then EUL, then laterally into the PCM, then tied, but not tightly. Incisions were closed with vicryl sutures. In six women, the ULP operation was carried out with 300 mL in the bladder. In these six women, the No. 18 Foley catheter was inserted and removed as required, so cough tests could be carried out for continence at relevant stages of the operation, specifically: before starting, after the polyester suture on one side, then after suturing was completed on both sides. At 6 months postoperatively, 31/36 (86%) women with leakage on cough test were cured of SUI and 11/19 (58%) were cured of concomitant urge. Twelve-month ULP data were recently submitted for publication. There were five surgical failures, four immediately postoperatively, and one after 3 months. Reference to the original experimental animal studies (3) indicated that collagen 1, the key structural support of the PUL, had formed by 3 months, an optimistic sign for longer term cure.
Discussion
There is no better example of Salvador Gil Vernet’s famous statement than the development of the MUS over a 35-year period, “almost mathematical knowledge of anatomy is a highly fertile source of surgical applications, suggesting new techniques and helping perfect and simplify existing surgical methods”. The revolution for SUI against the Burch colposuspension, began with the prototype MUS in 1988 (1) where tapes created artificial collagenous neoligaments (3) to repair PULs. The Tissue Fixation System (TFS) minisling in 2005 (7) further reduced surgical trauma and complications, in particular, post-operative urinary retention. The artisan tension-free minisling tapes (9,10) further reduced operating time, intraoperative complications and vastly reduced postoperative urinary retention. Long-term cure rates of 91% at 5.7 years (10), as good as any studies to date, were achieved at a very low cost for the health system. The one remaining complication was 4.3% tape erosions. The ULP (11) operation uses no tapes and (differently) prevents elongation of the PUL on effort. If the No. 2 or No. 3 polyester sutures can produce sufficient collagen to reinforce the PUL, with equivalent cure rates, the last significant complication of the MUS, tape erosions, could be confined to history.
Conclusions
If it fulfils its early promise, the wide-bore polyester suture, the ULP repair, will eliminate the two persisting problems with the MUS, tape rejection, and postoperative urinary retention. Minor granulation reaction to the braised sutures is possible, which raises the question of wide monofilament sutures, but these are unlikely to be as collagenopoietic. If proven to be successful over long periods, will the ULP be the final therapeutic piece of the SUI puzzle? Probably not. Effective outpatient methods would be the next step. For example, the radiofrequency methods used for vaginal epithelium could possibly be applied into the PUL to create new collagen. However, any such method would need precise ultrasound control, significant skill, and caution not to injure the urethra. A further problem is knowing how much current is required to regenerate the collagen without destroying the smooth muscle and nerves of the ligament which the ULP conserves. Whatever the “next advance”, “Precise, almost mathematical knowledge of anatomy” is required.
Acknowledgments
We would like to thank Vani Bardetta for her proofreading and administrative services for this article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1764/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1764/coif). The series “Integral Theory Paradigm” was commissioned by the International Society for Pelviperineology without any funding or sponsorship. Peter Petros serves as an unpaid editorial board member of Annals of Translational Medicine from October 2022 to September 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images. Human participation in the video was by patient permission on the basis it was deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Petros PE, Ulmsten UI. The combined intravaginal sling and tuck operation. An ambulatory procedure for cure of stress and urge incontinence. Acta Obstet Gynecol Scand Suppl 1990;153:53-9. [Crossref] [PubMed]
- Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 1990;153:7-31. [Crossref] [PubMed]
- Petros PE, Ulmsten UI, Papadimitriou J. The autogenic ligament procedure: a technique for planned formation of an artificial neo-ligament. Acta Obstet Gynecol Scand Suppl 1990;153:43-51. [Crossref] [PubMed]
- Toozs-Hobson P, Cardozo L, Hillard T. Managing pain after synthetic mesh implants in pelvic surgery. Eur J Obstet Gynecol Reprod Biol 2019;234:49-52. [Crossref] [PubMed]
- Nakamura R, Yao M, Maeda Y, et al. Retropubic tissue fixation system tensioned mini-sling carried out under local anesthesia cures stress urinary incontinence and intrinsic sphincter deficiency: 1-year data. Int J Urol 2017;24:532-7. [Crossref] [PubMed]
- Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 2001;11:1306-13. [PubMed]
- Petros PEP, Richardson PA. The midurethral TFS sling- a ‘micro-method’ for cure of stress incontinence- preliminary report. ANZJOG 2005;45:372-5. [PubMed]
- Sivaslioglu AA, Unlubilgin E, Aydogmus S, et al. A prospective randomized controlled trial of the transobturator tape and tissue fixation mini-sling in patients with stress urinary incontinence: 5-year results. J Urol 2012;188:194-9. [Crossref] [PubMed]
- Piñango-Luna S, Level-Córdova L, Petros PE, et al. A low cost artisan tension-free tape technique cures pelvic organ prolapse and stress urinary incontinence - proof of concept. Cent European J Urol 2020;73:490-7. [PubMed]
- Uysal D, Güven CM, Akgün Kavurmaci S, et al. Long-term efficacy of the single-incision mini-sling procedure using surgeon-tailored mesh. Eur J Obstet Gynecol Reprod Biol 2023;287:59-62. [Crossref] [PubMed]
- Petros P, Palma P. Conceptualizing stress urinary incontinence surgery beyond midurethral slings: Very early results from simplified ligament repair without tapes. Neurourol Urodyn 2023;42:383-8. [Crossref] [PubMed]


