
Squatting-based exercises cure bedwetting in children and improve pain and bladder symptoms in premenopausal women
Highlight box
Key findings
• Squatting-based pelvic exercises cure up to 86% of children aged 6–11 years with bed-wetting.
• A majority of premenopausal women had 50% improvement in overactive bladder (OAB), chronic pain, retention, stress urinary incontinence (SUI).
What is known and what is new?
• Kegel exercises are voluntary, learnt, and improve only SUI.
• Squatting-based Skilling exercises strengthen the three reflex pelvic muscles and the ligaments they contract against to improve bladder/bowel/pain symptoms.
What is the implication, and what should change?
• Prima facie, squatting exercise results for children with bed-wetting seem a better option than bed alarms. For adult women, these Skilling exercises improve OAB, chronic pain, retention, as well as SUI, but only for pre-menopausal women.
Introduction
The key points of the article are summarized in the video abstracts (Videos S1,S2).
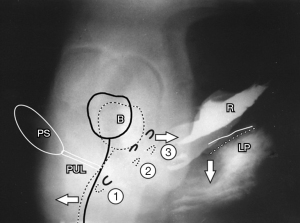
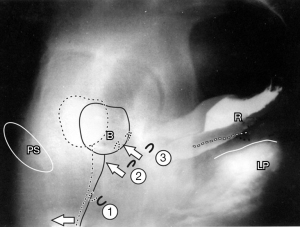
Current pelvic floor rehabilitation (PFR) methods in the female address mainly stress incontinence. Fundamental to any pelvic muscle exercise treatment for dysfunction is a clear understanding of the actions of pelvic muscle forces. During coughing or straining, three directional muscle forces are seen, forwards, backwards, downward (1,2) (Figure 1, broken lines) (see Videos S1,S2). “Squeezing”, upward pulling of the pelvic diaphragm is known as the Kegel technique (Figure 2). It has been the core exercise for all traditional pelvic exercise treatments for stress urinary incontinence (SUI). Squeezing is unidirectional and is not the natural closure mechanism, so it must be learnt, gaining the description, “the knack”. In contrast, the natural closure mechanism, which is trained by the squatting-based Skilling technique, is activated by the three opposite directional forces as shown in Figure 1, as described in the 1990 Integral Theory (1).
As regards urge, frequency and nocturia, the current PFR view is that such symptoms should be treated with “bladder training”, a methodology which trains the inhibitory circuits of the brain. The patient is taught to “hold on”. Pain treatment depends on the site. It consists of biofeedback, identifying and treating “trigger points” in the pelvis and often psychological treatment.
The Skilling PFR method for adult women
The origins of the Skilling method were the high cure rates obtained surgically for SUI, overactive bladder (OAB) (urge, frequency, nocturia), bladder emptying problems and chronic pelvic pain by repairing the pubourethral ligament (PUL) and uterosacral ligament (USL) based on the Integral Theory (1-4). It was reasoned that squatting would strengthen the three directional forces (arrows in Figure 1) and, in turn, the PULs and USLs they contract against. The Skilling method is based on squatting, with adjunctive electrotherapy, if available, using a probe inserted into the posterior vaginal fornix. A 50% symptomatic improvement has been demonstrated for SUI, and also, chronic pelvic pain, urge, nocturia, abnormal emptying (5) (see Table 1).
Table 1
| Fate of individual symptoms | Condition, n | >50% improvement, n [%] or mean |
|---|---|---|
| Stress incontinence | 69 | 57 [82] |
| Urge incontinence | 44 | 33 [68] |
| Frequency only | 12 | 10 [83] |
| Nocturia | 32 | 29 [90] |
| Pelvic pain | 17 | 13 [76] |
| Residual urine 202 mL | 23 | 71 mL |
Reused from (5). Copyright 2017, with permission from Pelviperineology.
URL for Skilling exercises (5): https://cms.galenos.com.tr/Uploads/Article_36478/Pelviperineology-36-79-En.pdf.
Note: much of the information which follows has been taken from the original descriptions (5,6).
Electrotherapy was used in the first month to “kick start” the response. A simple low-cost battery-operated electrical stimulator that delivered a square 50-Hz pulse every two seconds, was used for 4 weeks. For SUI, the probe was placed just inside the introitus for 20 minutes every second day, and into the posterior fornix for 20 minutes every second day. For posterior zone symptoms, (e.g., pelvic pain, high residual urine, nocturia), the probe was inserted into the posterior fornix for 20 minutes per day. Bladder suppressant drugs were never used.
Squatting was the core exercise, 20 minutes per day in divided segments, preferably while performing some household tasks. In patients who could not or would not squat, sitting on a large rubber “fit-ball” during work or household duties was encouraged. Time management was improved by encouraging patients to perform one group of twelve exercises on waking, retiring, and on visiting the toilet. The patient was encouraged to substitute squatting for bending at all times. If a patient had arthritis, she was encouraged to sit on the end of a chair or on a fitball with legs apart.
There were 147 patients, mainly premenopausal women, mean age 52.5 years (range, 25–76 years) and mean parity 2.25 times (range, 0–5 times), who commenced the full regime. Ten patients were nulliparous. The dropout rate was 47% (Table 1).
The Results are summarized in Table 1. A 50% self-estimated improvement was the cut-off point for Table 1. The percentage (%) is calculated on the original number of women who achieved >50% improvement in the particular symptom.
Cure of day/night enuresis in children by modified Skilling pelvic floor regime
The URL for day/night enuresis https://pubmed.ncbi.nlm.nih.gov/33133658/ (6).
The Skilling method, based on strengthening the three reflex pelvic muscles and ligaments, was applied in a modified way to treat children with day/night enuresis. The hypothesis was an inability of pelvic muscles/ligaments to control an inappropriately activated micturition reflex. The anatomical basis of this method was the demonstrated role of pelvic muscles and ligaments in the closure and micturition reflexes in adults (1).
Forty-eight children, aged 7.6±2.5 years, 34 females, 14 males, with day/night enuresis, had strictly supervised exercises twice daily, 10 squats, 10 bridge exercises for 4 months (6). As can be seen in Table 2, at the first review (4 weeks) 12/24 in the treatment group reported total cure of wetting; 41/48 children (85%) were cured of both daytime/night-time enuresis (P<0.001) at 4 months. There were no adverse events. Secondary outcomes were concomitant cure of constipation, fecal incontinence, urinary retention as predicted by the underlying Integral Theory of incontinence (1).
Table 2
| Questions | Entry | 2 weeks | 1 month | 4 months |
|---|---|---|---|---|
| Voiding daytime | 3.12±0.9 | 6.06±1.3 | 6.78±1.1 | 6.7±1.1 |
| Bedwetting days per week | 6.44±1 | 3.06±1.6 | 0.98±1.6 | 0.38±1 |
| Yes | 48 (100.0) | 24 (50.0) | 7 (14.6) | 7 (14.6) |
| Daytime leaks days per week | 7.22±2.9 | 2.28±1.6 | 0.64±1.2 | 0.3±1.2 |
| Sometimes | – | 12 (25.0) | 12 (25.0) | 0 (0.0) |
| Fecal soiling number of patients | 9 (18.8) | – | – | 0 (0.0) |
| Bladder emptying difficulty number of patients | ||||
| Yes | 15 (31.3) | – | – | 0 (0.0) |
| Post-void residual | 15 (31.3) | – | – | 0 (0.0) |
| Urge number of patients | ||||
| Yes | 46 (95.8) | 32 (66.7) | 6 (12.5) | 4 (8.3) |
| No | 2 (4.2) | 16 (33.3) | 42 (87.5) | 44 (91.7) |
| Squatting exercises total number of patients completed | ||||
| Yes | 0 (0.0) | 46 (95.8) | 46 (95.8) | 46 (95.8) |
| No | 48 (100.0) | 2 (4.2) | 2 (4.2) | 2 (4.2) |
| Number of defecations by a week | 4.34±1.9 | 5.82±1.1 | 6.30±0.9 | 6.44±0.8 |
| Characteristics of stools—Bristol scale | ||||
| Soft | 15 (31.3) | 25 (52.1) | 40 (83.3) | 46 (95.8) |
| Hard | 33 (68.8) | 23 (47.9) | 8 (16.7) | 2 (4.2) |
Data are presented as mean ± SD or n (%). Reused from (6). Copyright 2020, with from permission Central European Journal of Urology. SD, standard deviation.
Table 2 summarizes the results with this strictly supervised exercise regime, which were remarkable and unexpected, 86% cure of males and females aged 6–11 years (6), (Table 2). With reference to Table 2, it is important to note that it was not only nocturnal enuresis (bedwetting) which was cured. Daytime wetting, bladder emptying problems and constipation were also cured (6).
An important question was, how did the exercises work? The authors believed the exercises accelerated normal childhood strengthening of muscles/ligaments which control inappropriate activation of the micturition reflex which we hypothesize is the basis for daytime/night-time enuresis.
Conclusions
The Skilling exercises work best in premenopausal women because they have stronger pelvic muscles and better collagen. The authors hypothesized that what was happening with the children was an acceleration of the disappearance of bedwetting which naturally occurs when children reach puberty (3).
Acknowledgments
We would like to express our gratitude to Editors Professor Peter Petros and Vani Bardetta for their exceptional support in the design and refinement of the article.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the International Society for Pelviperineology for the series “Integral Theory Paradigm” published in Annals of Translational Medicine. Peter Petros (Editor) and Vani Bardetta (Assistant Editor) served as the unpaid Guest Editors of the series. The article has undergone external peer review.
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-1768/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-1768/coif). The series “Integral Theory Paradigm” was commissioned without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article, accompanying images and videos. Human participation in the videos was by patient permission on the basis it was deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl 1990;153:1-78. [PubMed]
- Petros P, Abendstein B, Swash M. Retention of urine in women is alleviated by uterosacral ligament repair: implications for Fowler's syndrome. Cent European J Urol 2018;71:436-43. [PubMed]
- Liedl B, Inoue H, Sekiguchi Y, et al. Is overactive bladder in the female surgically curable by ligament repair? Cent European J Urol 2017;70:53-9. [PubMed]
- Abendstein B, Brugger C, Furtschegger A, et al. Study No. 12: Role of the uterosacral ligaments in the causation of rectal intussusception, abnormal bowel emptying, and fecal incontinence. A prospective study. Pelviperineology 2008;27:118.
- Skilling PM. Pelvic floor exercises according to the Integral Theory: strengthening the 3 directional muscle forces improves chronic pelvic pain, bladder & bowel dysfunctions. Pelviperineology 2017;36:79-83.
- Garcia-Fernandez A, Petros PE. A four month squatting-based pelvic exercise regime cures day/night enuresis and bowel dysfunction in children aged 7-11 years. Cent European J Urol 2020;73:307-14. [PubMed]


